Scott E. Brodie, Jasmine H. Francis
Aging and Disorders of the Eye
Loss of vision, one of the most feared forms of medical disability, falls disproportionately on older adults. Unfortunately, the damage to the delicate tissues of the eye from the various metabolic insults that may occur throughout life is generally cumulative. Consequently, most forms of ocular pathology occur ever more frequently, and in more debilitating forms, with increasing age.
Estimates of the prevalence of blindness from all causes vary by perhaps a factor of 13 between industrialized and Third World countries.1 Nevertheless, regardless of the degree of economic development, the prevalence rate for blindness in any society is typically 100-fold greater among individuals older than 65 years than among children in the same country.2 In developed countries, the major causes of blindness (Box 95-1) are primarily cataract, glaucoma, and retinal disease (mostly macular degeneration and diabetic retinopathy), all of which are strongly related to advancing age.3 In the Third World, the major causes of blindness are cataract, corneal scarring, glaucoma, and retinal disease.4
Delivery of adequate eye care to older adults remains an unsolved problem, even in wealthy countries. Recent surveys in the United States have identified significant rates of untreated eye disease among older adults. The nursing home population appears to be notably underserved.5,6
Discussion of age-related ocular problems is organized in this chapter by considering the visual apparatus in anatomic order, from anterior to posterior.
Eyelids
The eyelids are vital for the proper circulation of tears and maintenance of the smooth ocular surface necessary for clear image formation by the eye. With increasing age, the skin of the eyelids, as elsewhere, loses elasticity, and the lids become more loosely apposed to the globe. Atrophy of the fascial planes within the eyelids may lead to herniation of the orbital fat into the lid tissue, producing the bags under the eyes frequently seen in older adults (Figure 95-1). Atrophy or disinsertion of the aponeurosis of the levator palpebrae muscle, which ordinarily supports the upper eyelid, may cause the opened lid to fail to uncover the pupil, as seen in senile ptosis, despite normal levator muscle function (Figure 95-2). Senile ptosis must be differentiated from ptosis due to mechanical and neuromuscular causes, such as oculomotor nerve palsies and myasthenia gravis.7

Laxity of the lower lid may allow the free lid margin to rotate away from the eyeball, a condition known as ectropion (Figure 95-3). If severe, the lacrimal punctum may fail to make contact with the pool of tears adjacent to the lower lid. This prevents the normal conduction of tears into the lacrimal sac, which may result in persistent tearing (epiphora), even in the absence of lacrimal duct obstruction. More dangerous is entropion, in which a loosening of the adhesions between tissue planes in the lid allows the muscle tone of the orbicularis oculi to rotate the lid margin inward (Figure 95-4).8 Frequently, the lashes come to rub directly against the cornea or conjunctiva, producing irritation or scarring.
The treatment of eyelid malpositions is generally surgical. For senile ptosis, resection of the levator aponeurosis is generally performed.9 Ectropion and entropion are generally treated by resection of redundant lid tissue.10
Of the tumors of the eyelid skin, basal cell carcinomas are the most common; squamous cell carcinomas are also possible. Both these tumors are frequently a consequence of lifetime exposure to sunlight. If the lesions are detected early, a curative local resection is often possible. In advanced cases, the tumor may cause massive destruction of facial structures by local extension. Metastases are very rare.11
Lacrimal Apparatus
The lacrimal apparatus consists of the lacrimal glands, which secrete the tears, and lacrimal sac and ducts, which convey the tears into the nasal cavity. Secretory function of the lacrimal glands declines with age, and many older adults develop dry eye syndrome. This nonspecific reduction in tear production is much more common than the full-fledged Sjögren syndrome, which is an autoimmune disease process affecting salivary and lacrimal secretion.12 Paradoxically, many tear-deficient patients complain of excess tearing because the chronically irritated eyes may stimulate reflex tear production. Dry eyes are treated with artificial tear eye drops, as often as needed. Some patients respond well to topical treatment with cyclosporin A.13 In patients whose eyes dry out overnight, lubricant ointment at bedtime may be helpful. In severe cases, small silicone plugs may be placed to obstruct the lacrimal puncta,14 or surgical occlusion of the lacrimal puncta may be performed to conserve the available tears.
Obstruction of the lacrimal ducts also leads to epiphora. Uncomplicated mechanical stenosis may occasionally be relieved with simple probing, but severe cases (often following bacterial infection of the lacrimal sac) are treated surgically. A dacryocystorhinostomy is performed to anastomose the mucosa of the nasal cavity to the lacrimal sac through an osteotomy made in the lacrimal bone.15
Conjunctiva
Subconjunctival hemorrhage, a localized accumulation of blood seen between the conjunctiva and globe, is frequently encountered in older adults, either following minor trauma or occurring spontaneously (Figure 95-5). The Valsalva maneuver may be a precipitating event. Such hemorrhages are rarely of any consequence, but they are often alarming in appearance. They resolve spontaneously without treatment over a period of several days. Occasionally, recurrent hemorrhages may suggest an underlying disease such as hypertension or a coagulation disorder, or perhaps an occult tumor.
Chronic exposure to sunlight, particularly at tropical latitudes, may cause a degeneration of the connective tissue in the exposed sector of the conjunctiva between the eyelids, leading to thickening of the conjunctiva (pinguecula), which may grow over the cornea from the periphery toward the pupil (pterygium). If the growth threatens to cover the visual axis, surgical excision may be indicated. Recurrence after surgery is, unfortunately, not uncommon.16
Tumors such as squamous cell carcinoma and melanoma may arise from the conjunctiva. Primary acquired melanosis and squamous dysplasia must be distinguished from malignant tumors. Local excision and cryoablation may be adequate in early cases, but advanced cases may require other interventions (e.g., radiation therapy, systemic treatment with chemotherapy or potentially with targeted molecules) or even orbital exenteration.17,18
Cornea
The eye is unique in its requirement for transparent tissues, including the cornea and crystalline lens. The need for transparency places many constraints on the architecture and metabolism of these ocular structures. In particular, the eye must nourish these tissues with a cell-free fluid, because red blood cells preclude transparency. Similarly, the transparent tissues must rely primarily on anaerobic glycolytic metabolism because the enzyme systems required for oxidative phosphorylation (aptly named cytochromes) strongly absorb visible light. Even in the absence of these absorbent components, the tissues must be constructed in a highly compact and regular manner so that light scattering from tissue organelles does not cause a white opaque appearance. This requirement is met in the case of the cornea by a highly regular arrangement of collagen fibrils and an active metabolic pump in the corneal endothelial cell layer, which dehydrates the corneal stroma. Absence of these tissue features explains why the sclera, which is otherwise histologically similar to the cornea, is opaque.19
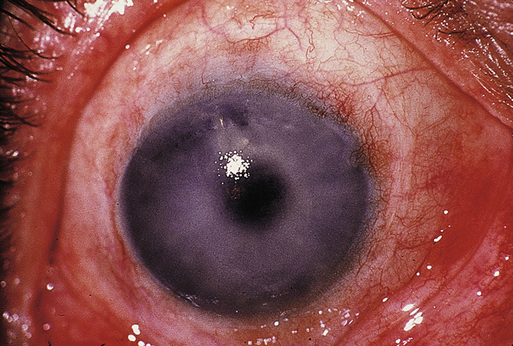
The corneal endothelial cells, on which the dehydration critical for corneal transparency depends, do not divide during adulthood. Endothelial cell density declines slowly with age.20 If the number of endothelial cells falls below a critical level, the cornea imbibes fluid, swells, and becomes cloudy (Figure 95-6). Edema fluid percolates to the epithelial surface and may coalesce into subepithelial bullae. Mild cases may be managed with the use of hypertonic saline eye drops and ointment to withdraw fluid from the cornea osmotically. If these measures fail, a corneal graft, which replaces the deficient endothelium, is necessary to restore vision.21 In addition to full-thickness corneal transplants, there are now options for partial-thickness procedures (Descemet stripping and automated endothelial keratoplasty [DSAEK] and Descemet membrane endothelial keratoplasty [DMEK]),which replace only the diseased back layer of the cornea. These procedures have the advantage of being sutureless and offer quicker recovery times.
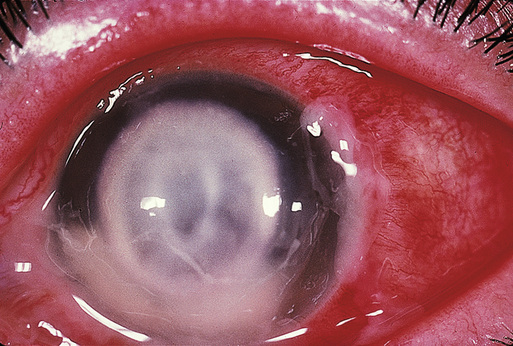
Bacterial ulcers of the cornea (Figure 95-7) seem to occur with greater frequency in older adults, perhaps reflecting impairments of tear secretion, epithelial integrity, and cellular and humoral immunity, and are associated with a poorer prognosis in older adults.22 Intensive antibiotic therapy is generally required. Fourth-generation fluoroquinolones have been shown to be as effective as fortified antibiotics23,24 and may be easier to obtain.
The ring-shaped deposition of lipid in the far periphery of the cornea, termed the arcus senilis, is completely benign.
Uveal Tract
The uveal tract (uvea) is comprised of the iris, ciliary body, and choroid, which form a continuous, highly vascular layer inside the sclera. Inflammation of the uvea occurs frequently as a primary disease process in response to infections, in many patients with rheumatic disease, and as a sequela to accidental or surgical trauma. Clinically, inflammatory cells are seen in the aqueous or vitreous humor. These inflammatory reactions can cause ocular injury by many mechanisms. They may occlude the trabecular meshwork, causing glaucoma. They may accumulate on the inner surface of the cornea as keratic precipitates, where they may injure or destroy the corneal endothelial cells and cause corneal edema. Inflamed tissues often develop pathologic adhesions, which may derange normal ocular function. Adhesions between the anterior surface of the peripheral iris and anterior chamber angle (peripheral anterior synechiae) may occlude the trabecular meshwork, leading to chronic angle-closure glaucoma. Adhesions between the posterior surface of the iris and anterior surface of the crystalline lens can seal off access of the aqueous humor to the anterior chamber (pupillary block), forcing the iris to bow forward (iris bombé). In cases in which the peripheral iris becomes apposed to the trabecular meshwork, the egress of aqueous humor from the eye is blocked, resulting in angle-closure glaucoma. In the posterior segment, inflammatory cells in the vitreous humor may obscure vision and lead to fibrovascular proliferation, which may distort the retina or even cause a retinal detachment.
Treatment in most cases of uveitis is generally empirical. Dilation of the pupil with cycloplegic eye drops is generally advisable to prevent posterior synechiae and pupillary block and relieve the discomfort (photophobia) caused by light-induced miosis of the inflamed iris. If the inflammation is confined to the anterior segment, topical corticosteroid eye drops are usually sufficient. In cases involving the posterior segment, periocular corticosteroid injections or systemic administration of corticosteroids are frequently required.25 In the most severe cases, systemic administration of immunomodulators or biologics has proven to be useful.26 Typically, a workup for associated systemic disease is appropriate. If a treatable condition is discovered, such as syphilis or tuberculosis, specific treatment for the underlying condition may simultaneously cure the uveitis.
Intraocular tumors in older adults usually occur within the uveal tract. Melanomas are the most common primary tumor. Although prompt enucleation (surgical removal of the eyeball) was long the traditional management, many authorities now recommend that eyes containing small uveal melanomas be followed closely, rather than enucleated, because they have only a low propensity for metastasis.27 Medium-sized tumors have been successfully treated in many cases with irradiation by temporary implantation of a radioactive plaque applied to the overlying sclera28 or administered by external beam x-ray or proton beam.29 A large prospective clinical trial found no difference in 5-year survival between groups of patients randomized to treatment by radioactive plaque or by enucleation.30 Primary enucleation is often recommended for large tumors. Metastatic melanoma is usually detected initially in the liver. Annual magnetic resonance imaging (MRI) of the abdomen and monitoring of hepatic enzyme activity in the serum are advisable for patients at risk.31 Traditionally, estimates of the risk of metastatic disease have been based on the clinical features and histologic architecture of the primary tumor. Recent studies have suggested that better estimates of metastatic risk may be obtained via determination of the genetic underpinnings of the intraocular tumor. This can be achieved by using DNA- and RNA-based assays.32,33 For example, a somatic mutation in BAP1 (BRCA-associated protein 1) has been implicated in tumors at high risk for metastases.34 Furthermore, a germline mutation in BAP1 has been associated with a hereditary cancer syndrome that includes uveal melanoma, lung mesothelioma, renal cell carcinoma, and gastric cancer.35 Genetic mutations within the metastatic tumor may qualify the patient for novel systemic treatments that target the aberrant molecular pathway.36
Tumors metastatic to the choroid are actually more frequent than primary intraocular tumors. Lung primaries predominate in men and breast primaries in women.37 Because the eye is seldom the sole site of metastasis, these patients generally require systemic chemotherapy. Additional treatments often used for sight-threatening lesions include radiation, anti–vascular endothelial growth factor (VEGF) injections, and lasers.38
Glaucoma
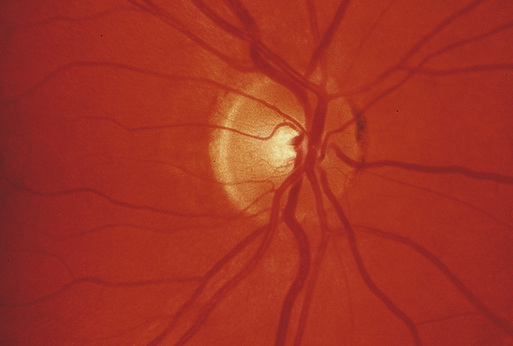
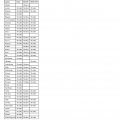
Glaucoma is a form of progressive atrophy of the optic nerve, frequently associated with increased intraocular pressure (IOP; Figures 95-8 and 95-9).
Open-Angle Glaucoma
In many cases, the primary pathology is presumed to lie in the trabecular meshwork, the ring of porous tissue located in the anterior chamber angle through which aqueous humor drains from the eye. Impaired facility of aqueous outflow through the trabecular meshwork is generally idiopathic (so-called primary open-angle glaucoma). This condition is generally reported to increase in prevalence with increasing age, at least in most Western populations.39 Loss of outflow facility may also arise from various insults to the trabecular meshwork, including trauma, uveitis, hemorrhage, and dispersion of intraocular pigment.
Visual impairment from open-angle glaucoma is generally insidious and chronic, with visual field damage occurring initially in the far periphery, where it is rarely noticeable except by formal testing. The ability to diagnose this condition in its early stages is imperfect. The actual risk of visual field loss in untreated individuals with modestly elevated IOP is only 1% to 2%/year40; conversely, histologic studies have shown that as many as 40% of the optic nerve fibers must be destroyed before any abnormality of the visual field is detectable by standard techniques.41
Initial treatment is usually medical. The goal of therapy is to lower the IOP with topical (or, rarely, systemic) medications to a level that is tolerated by the optic nerve, as demonstrated by arrest of the progressive visual field loss. Available medications include parasympathomimetic miotics (rarely used), anticholinesterase miotics (rarely used), sympathomimetics, β-adrenergic blockers, carbonic anhydrase inhibitors, and prostaglandin analogues. The potential side effects of the various topical and systemic pressure-lowering drugs are occasionally serious, particularly in older patients (see later, “Systemic Complications of Ophthalmic Medications”).
If medical treatment is unsuccessful or poorly tolerated, the IOP may be further lowered by laser treatments to the trabecular meshwork or by so-called filtering surgery, which creates a fistula between the anterior chamber and subconjunctival space, allowing easier egress of aqueous humor. Complications of filtering surgery may include hypotony, choroidal effusion, and cataract. Supplementary medical treatment after filtering surgery may also be required. The optimal stage in the disease process for surgical intervention is unclear. Some authors have reported better long-term visual results with earlier surgery.42 One large study has suggested that laser treatment to the trabecular meshwork may also be suitable as initial therapy.43
Angle-Closure Glaucoma
Occasionally, alterations in the intraocular anatomy may predispose the iris to cover the trabecular meshwork, suddenly preventing aqueous outflow and causing an acute elevation of the IOP. Common scenarios include adhesions between the iris and lens (pupillary block), which may cause the iris to bow forward so as to occlude the trabecular meshwork, and dilation of the pupil, which may occur spontaneously in the dark or following pharmacologic mydriasis. Gradual enlargement of the lens with increasing age or cataract formation is an important factor that predisposes the eye to this process in older adults. Acute angle-closure glaucoma is generally a dramatic event, with symptoms that include severe pain, blurring of vision, perception of colored haloes around lights, nausea, and vomiting. Diagnosis of acute angle-closure glaucoma is easy once attention is directed to the eye, but may be missed if attention is diverted to the gastrointestinal symptoms. Cases have been reported from the emergency departments of general hospitals where concentration on the nausea and vomiting of a patient with acute angle-closure glaucoma actually led to exploratory laparotomy.
The massive elevation of IOP following acute angle-closure glaucoma (often to triple the normal upper limit of 21 mm Hg) may cause permanent optic nerve damage within a matter of weeks. Acute angle-closure glaucoma is initially treated by lowering the IOP with systemic and topical medications, including miotic eye drops and systemic osmotic agents. In cases of pupillary block, a small hole (peripheral iridotomy) is made in the iris by laser or invasive surgery to bypass the pupillary block and allow passage of aqueous humor from the posterior segment into the anterior chamber. This prevents subsequent angle-closure glaucoma attacks. Because the anatomic factors that predispose an eye to acute angle-closure glaucoma are generally found bilaterally, it is usually considered prudent to perform a peripheral iridotomy prophylactically in the fellow eye after an attack of angle closure. However, recent evidence suggests that cataract extraction may be the optimal means of controlling IOP in eyes with primary angle-closure glaucoma.44
Prolonged episodes of angle-closure glaucoma may result in permanent damage to the trabecular meshwork or even adhesions between the iris and sectors of the trabecular meshwork, leading to chronic angle-closure glaucoma. If the angle is sufficiently compromised, filtering surgery may be necessary.
Normal-Tension Glaucoma
Although an elevated IOP has historically been the hallmark of the diagnosis of glaucoma, it has become clear in recent decades that many patients with otherwise typical glaucomatous optic atrophy and visual field loss seldom, if ever, are found to have elevated IOP. Identification and treatment of this so-called low-tension glaucoma (more accurately termed normal-tension glaucoma) remains problematic although, even in this cohort, reduction of IOP is thought to convey some benefit. This entity is probably more common than previously thought—population-based surveys have demonstrated a substantial incidence of otherwise typical glaucomatous field loss in patients with normal IOP.45
Crystalline Lens
The crystalline lens of the eye is a unique ectodermal structure that develops entirely within the primordial lens vesicle. Only the cells on the extreme periphery of the lens divide, adding cells to the outer surface of the growing lens. Thus, the center of the adult lens represents the earliest tissue laid down during embryonic development. There is no mechanism whereby these cells can turn over, unlike the situation in typical ectodermal structures, such as the skin. The metabolism of the lens is largely confined to anaerobic glycolysis because neither hemoglobin-mediated oxygen transport nor cytochrome-mediated oxidative phosphorylation is available because of the need for transparency. The lens is at a further metabolic disadvantage because of the need to maintain a state of great disequilibrium with its surroundings—the lens must maintain the highest protein concentration and one of the lowest water concentrations of any tissue in the body. Thus, relatively modest metabolic insults or osmotic stresses may overwhelm the lens metabolism, resulting in protein denaturation and cataract formation.21
The lens of the eye continues to grow and mature throughout life. As the lens ages, it becomes more rigid and responds less effectively to changes in ciliary muscle tone, decreasing the effectiveness of accommodation, the eye’s mechanism for focusing from distant to near objects. This loss of accommodation (presbyopia) is managed with reading glasses, bifocals, or other refractive strategies.
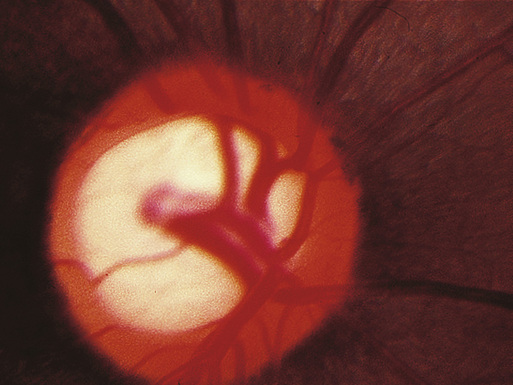
The lens responds to virtually any mechanical or metabolic insult by loss of optical clarity, resulting in the formation of a cataract (Figure 95-10). Several patterns of opacities are commonly encountered:
Oxidation (browning reactions) of lens proteins, particularly in the older, central portions of the lens, is termed nuclear sclerosis, which may result in alterations in the refractive index of the lens, as well as frank opacity. The most common refractive change is in the direction of an increase in myopia or decrease in hyperopia. In some cases, this refractive shift will allow the patient to read without reading glasses (so-called second sight). This improvement in visual performance is usually only temporary and often heralds the development of a more debilitating lens opacity. Refractive changes in the lens need not be uniform. Patients will occasionally report monocular diplopia from inhomogeneous refraction by distinct portions of the lens, resulting in two distinct images being formed on the retina. The notion that monocular diplopia is generally indicative of hysteria is incorrect.
Denaturation of lens proteins in a sector of adjacent cortical lens fibers results in wedge-shaped or cuneiform cortical opacities. These are often found in the far periphery of the lens but frequently spare the optical zone near the center.
Aberrant proliferation of lens fibers on the posterior lens capsule produces a posterior subcapsular cataract. This is often induced by topical or systemic corticosteroid treatment and is frequently seen in other disease states, such as retinitis pigmentosa.
Treatment of cataract is generally surgical. With rare exceptions, the lens proteins that constitute the opacity are irreversibly denatured, precluding medical treatment.46 Surgical strategies for removal of the lens material have evolved greatly. In all cases, an incision must be made in the eyeball. A cataract cannot be removed—even with a laser—without an ocular incision. The simplest operation is to remove the entire lens intact within its lens capsule, a so-called intracapsular procedure. At present, the extracapsular procedure, in which the opaque lens tissue is carefully aspirated from within the lens capsule, has become standard, because retention of the capsule to serve as a barrier between the anterior and posterior segments of the eye appears to reduce the rate of complications. Greater emphasis has been placed on the development of minimally invasive surgical methods for cataract extraction. Often, the cataract can be liquefied by the mechanical action of a rapidly vibrating needle (phacoemulsification) and aspirated from the eye through an incision only 3 to 4 mm in length.47 Frequently, such wounds can be constructed to be self-sealing, eliminating the need for sutures.48 The femtosecond laser has been used to assist in some of the key steps in cataract surgery, including corneal incision, opening of the lens capsule, and fragmentation of the lens material.49
Indications for cataract surgery should be determined in relation to the visual needs of each individual patient. Occasionally, cataract extraction is recommended for technical reasons, such as those rare cases when the lens itself is causing injury to the eye (as in phacolytic glaucoma, when lens proteins leak from a cataractous lens and occlude the trabecular meshwork) or when a cataractous lens prevents adequate visualization or treatment of disease of the posterior segment of the eye, such as diabetic retinopathy. Otherwise, cataract surgery is appropriate whenever the anticipated improvement in visual function would be of benefit to the patient. In general, a visual result of 6/12 (20/40) or better may be anticipated in 90% to 95% of cases without other known concurrent ocular disease; thus, surgery is generally recommended only when the acuity has fallen to the level of 6/15 (20/50) or worse. In some patients, difficulties with glare, contrast sensitivity, diplopia, or specific occupational demands may justify cataract extraction, even with less severe loss of visual acuity.
Optical rehabilitation of the aphakic eye requires replacement of the focusing power of the cataractous lens that was removed. Where economic conditions permit, this is usually provided by means of a plastic intraocular lens prosthesis, which is generally implanted at the time of the primary cataract operation. Intraocular lenses were once thought to be an inaccessible expense and an option limited to those in developed nations. However, India is now tackling its burden of cataract blindness and is able to implant 90% of its cataract patients with intraocular lenses due to low-cost, indigenous lens manufacturing.50 Recent intraocular lens designs can even restore a degree of accommodation, reducing the need for reading glasses or bifocals in many cases, and these so-called premium intraocular lenses have favorable outcomes for some patients.51,52 Alternatives include contact lenses (often worn on an extended-wear basis) and thick aphakic spectacles, which subject the patient to substantial optical distortions and, if the aphakia is unilateral, may cause substantial difficulties because of unequal perceived image size in the two eyes. Indeed, the difficulties with spectacle correction of unilateral aphakia are sufficiently severe that if spectacle correction is the only modality of optical rehabilitation available, most surgeons recommend deferral of surgery until visual acuity in the better eye falls to 6/18 (20/60) or worse. In some developing countries, local custom may discourage the use of spectacles after cataract surgery. In these situations, the attitude and customs of the patient must be taken into account in the decision about whether to perform a cataract extraction.
Some yellowing of the lens proteins is nearly universal with aging. Sufficient opacity to impair visual acuity results in more than 3.5 million cataract extractions each year in the United States, the vast majority in individuals older than 65 years. In developing countries, the rate of cataract formation appears to be even higher, so that untreated cataract is typically the largest single cause of acquired blindness.3 In India, as recently as 8 years ago, the rate of procedures each year was finally able to surpass the rate of new cataract formation in the general population.50 This feat has been attributed to a number of factors, including low procedural costs and internal manufacturing of eye care goods.
Cataract formation may occasionally reflect an underlying metabolic abnormality, such as galactosemia or renal failure. Cataract onset is accelerated in diabetic patients and may be triggered by various drugs (particularly topical or systemic corticosteroids). In addition to these specific associations, several studies have shown a nonspecific excess mortality among cataract patients compared with age-matched control patients undergoing other elective surgical procedures.53,54
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree