Breast reconstruction continues to evolve along with advances in the detection and management of breast cancer. With more patients diagnosed with breast cancer earlier in life and increased identification of genetic mutations predisposing patients to breast cancer, patients’ desires and expectations regarding reconstruction have become more sophisticated. Restoration of the breast to a form as close as possible to its presurgical state continues to be a primary goal. The past decade has seen many advances in implant and autologous tissue–based reconstruction. The future of reconstruction for breast cancer patients is promising with continued research in ways to improve the care provided.
Key points
- •
Breast reconstruction efforts complement oncologic interventions in breast cancer patients, with the ultimate goal of restoration of breast form and function.
- •
Use of acellular dermal matrices in tissue expander/implant–based breast reconstruction represents one of the most significant advances in implant reconstruction in the past decade.
- •
Free flap and perforator flap options expand patients’ choices for reconstruction and result in breasts that are natural in both appearance and feel. These techniques are also better suited than implants for reconstruction of obese patients.
- •
Partial breast reconstruction options should be considered in all patients who opt for breast conservation therapy.
- •
Improvements in fat grafting techniques have the potential to improve on all existing forms of breast reconstruction and revolutionize the approach to breast reconstruction as a whole.
Introduction
Breast reconstruction is achieved through various reconstructive techniques that attempt to restore the breast to near-normal shape, appearance, and size after oncologic surgical resection in the form of lumpectomy or mastectomy. Several factors, including earlier detection of breast cancer and advances in radiation therapy and systemic treatments, have contributed to increased use of breast preservation and skin-sparing surgical techniques in the management of breast cancer patients. As a complement to these changes in management, breast reconstruction has evolved from procedures aimed at simply creating a breast with a satisfactory appearance when clothed to a series of procedures aimed at creating a breast that meets high aesthetic standards when bare. The psychological, social, emotional, and functional benefits of breast reconstruction have been well documented over the past 30 years. Previous studies have demonstrated the positive effects of postmastectomy reconstruction on psychological health, self-esteem, sexuality, and body image. These benefits will likely be enhanced as implant technology and surgical techniques evolve, with an improvement in the quality of the reconstructed breast. Today the surgical repertoire for breast reconstruction includes several autologous tissue flaps and prosthetic techniques using tissue expanders and implants. The most recent advances in breast reconstruction are presented.
Introduction
Breast reconstruction is achieved through various reconstructive techniques that attempt to restore the breast to near-normal shape, appearance, and size after oncologic surgical resection in the form of lumpectomy or mastectomy. Several factors, including earlier detection of breast cancer and advances in radiation therapy and systemic treatments, have contributed to increased use of breast preservation and skin-sparing surgical techniques in the management of breast cancer patients. As a complement to these changes in management, breast reconstruction has evolved from procedures aimed at simply creating a breast with a satisfactory appearance when clothed to a series of procedures aimed at creating a breast that meets high aesthetic standards when bare. The psychological, social, emotional, and functional benefits of breast reconstruction have been well documented over the past 30 years. Previous studies have demonstrated the positive effects of postmastectomy reconstruction on psychological health, self-esteem, sexuality, and body image. These benefits will likely be enhanced as implant technology and surgical techniques evolve, with an improvement in the quality of the reconstructed breast. Today the surgical repertoire for breast reconstruction includes several autologous tissue flaps and prosthetic techniques using tissue expanders and implants. The most recent advances in breast reconstruction are presented.
Reconstruction of mastectomy defects
Factors ranging from oncologic treatment plans to patient-specific factors are taken into consideration when planning a reconstructive strategy. A team-based approach with open communication between medical oncologists, radiation oncologists, oncologic surgeons, and reconstructive surgeons helps simplify planning. Key decisions that need to be made with a perspective of the treatment plan include the type and timing of reconstruction.
Decisions on Type of Reconstruction
Several options are available to women who choose breast reconstruction after mastectomy. The 2 broad categories available to patients include techniques using prosthetic implants and those involving autologous tissue flaps.
Some women have an inherent preference with regards to the technique, whereas others’ medical history or lifestyle may steer them toward a particular option. Although it is important that patients have a choice in the type of reconstruction performed, not all reconstructive options are available to every patient. Fig. 1 provides an algorithm highlighting some factors that affect the choice of reconstructive technique offered. It is the responsibility of the reconstructive surgeon to provide information to the patient about all potential options and provide guidance that allows her to make a decision that results in the safest and most aesthetically pleasing outcome.
Decisions on Timing of Reconstruction
The decision on immediate or delayed reconstruction in general is influenced by cancer staging, with delayed reconstruction favored in advanced-stage cancers that require postmastectomy radiation therapy (PMRT) or close surveillance. Most patients tend to prefer immediate reconstruction, which takes advantage of skin preservation while minimizing the length of time spent without a breast. Patients may also opt to wait on reconstruction if the combined process of oncologic treatment and reconstruction seems overwhelming. The need for PMRT tends to be the predominant reason influencing the choice for delayed reconstruction. Delayed reconstruction, for patients requiring radiation therapy, is typically advocated for several reasons, including the avoidance of untoward effects of radiation on the results of an immediate reconstruction and the potential for delaying oncologic treatment as a result of complications from reconstruction. In an attempt to take advantage of the skin preserved in a skin-sparing mastectomy in patients who require radiation, several plastic surgeons have suggested the immediate placement of tissue expanders. The skin is initially expanded and then, prior to radiation therapy, the expander is deflated temporarily if needed and re-expanded after completion of radiation. These patients can then proceed to the second stage of their reconstruction with an autologous or implant-based technique that takes advantage of the skin made available by expansion.
In recent years, a few investigators have also challenged traditional recommendations for delayed reconstruction in patients known to require PMRT, reporting equivalent clinical and aesthetic outcomes in immediate autologous tissue–based reconstructions in radiated and nonradiated patients.
Tissue Expander/Implant–Based Reconstruction
The use of prosthetic devices for breast reconstruction began in the early 1960s with silicone gel–filled implants, whereas tissue expanders were introduced in the 1970s. Currently there are several methods of prosthetic breast reconstruction and various types of implants with different shapes, textures, and fill material. The staged tissue expander/implant–based breast reconstruction represents the most commonly performed approach to implant reconstruction. A tissue expander is placed in a subpectoral pocket at the time of mastectomy or in a delayed fashion. After a period of serial expansions, the patient returns to the operating room, where the tissue expander is exchanged for a silicone- or saline-filled implant in an outpatient second-stage procedure. Subsequent procedures that could be performed to complete the reconstruction include contralateral procedures for symmetry (reductions, mastopexies, or implant augmentations in cases of unilateral reconstructions), nipple reconstruction, and nipple-areolar complex tattooing.
Prosthetic reconstructions provide distinct advantages of reduced operating times and postoperative recovery, obviating donor site surgery. Unique problems encountered with these forms of reconstruction include implant infection, exposure, capsular contracture, deflation, and migration.
Acellular Dermal Matrix
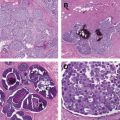
An innovation that has arguably had the most significant impact on prosthetic breast reconstruction over the past decade is the use of the acellular dermal matrix (ADM) for implant coverage. ADM is a biotechnological material obtained from human, bovine, or porcine dermis that undergoes processing to remove antigenic cellular components that cause rejection and inflammation. The resulting matrix provides the biologic scaffold required for tissue ingrowth and the biochemical components required for initiation of angiogenesis and revascularization. There are several types of ADM currently available, including AlloDerm (LifeCell, Branchburg, NJ, USA), FlexHD (Ethicon, Somerville, NJ, USA), Allomax (Davol, Warwick, RI, USA), and SurgiMend (TEI Biosciences, Waltham, MA, USA).
In general, the ideal position of a prosthetic device after mastectomy is in a subpectoral pocket. Studies have shown that placement of the implant in a purely submuscular position leads to more stable coverage and decreased complications, such as infection and seroma. There is, however, a greater potential for malposition, less control of the lower pole, and less intraoperative expansion obtained with total muscular coverage. Partial muscular coverage can be performed with or without ADM. When used, ADMs are inset within the inferior pole of the mastectomy defect for coverage of the inferolateral aspect of implants that are not covered by the pectoralis major muscle ( Fig. 2 ). This decreases the visibility of implant rippling, provides improved control of the inframammary fold, and allows for increased intraoperative fill ( Fig. 3 ). During the expansion process, use of an ADM results in easier lower pole expansion, with increased lower pole projection and the potential for an improved final aesthetic result ( Fig. 4 ).
ADMs can be used in most patients who are candidates for prosthetic reconstruction. It is less effective or relatively contraindicated in patients in whom prosthetic reconstruction may need to be delayed or avoided, including those who are morbidly obese, who are smokers, who have a history of radiation, or whose mastectomy skin flaps have questionable viability.
Single-Stage Implant Breast Reconstruction
The improvement in the ability to achieve greater intraoperative fill volumes with ADMs has enabled the development of single-stage implant techniques. Fully filled saline implants or silicone implants are placed at the time of a skin- or nipple-sparing mastectomy ( Fig. 5 ). This approach overcomes many of the disadvantages of tissue expander placement, including the need for multiple clinic visits for expansions and a subsequent operation to exchange the expander for an implant. Caution must be used, however, when counseling patients to advise them that they may require an additional operation for revisions to achieve symmetry.
Ideal candidates for single-stage implant reconstruction include those with small to medium-sized breasts with mild to moderate ptosis who are undergoing skin- or nipple-sparing mastectomies ( Fig. 6 ). Patients also have to be willing to be the same size or slightly smaller after reconstruction because the skin cannot be stretched at the time of the mastectomy without compromising flap perfusion. A moderate degree of preoperative ptosis is beneficial because expansions are not performed to increase the available skin envelope. Mastectomy flap viability is critical because the flaps must tolerate the additional weight and tension of an implant as opposed to a gradual increase in volume with a tissue expander.
The risks associated with single-stage implant reconstruction include infection, seroma, hematoma, skin necrosis, and capsular contracture. There is also a steep learning curve for surgeons. In a recent series of 439 patients undergoing this technique, the rate of reoperation was 11%, including a 3% rate of revision surgeries to deal with implant size changes, scar revisions, and inframammary fold revisions. Overall, clinical experience over the past 10 years has demonstrated the effectiveness, safety, and long-term aesthetic benefits of this approach.
Innovation in Prosthetic Devices
Since the development of breast implants as a medical technology device in the 1960s, significant improvements in safety and composition have been made. The first saline implants had shells created through high-temperature vulcanization and were prone to shell breakage, leakage, and spontaneous deflation. Contemporary saline implants are now made with stronger shells of a silicone elastomer manufactured with thicker, room-temperature vulcanized shells.
Five generations of silicone gel implants have been introduced since their development by American plastic surgeons, Thomas Cronin and Frank Gerow, and the Dow Corning Corporation in the 1960s ( Table 1 ). Key changes in implants over the years have centered on providing softer, more natural-appearing implants with a decreased risk of leakage of silicone gel.
| Generation | Time Period | Silicone Implant Characteristics |
|---|---|---|
| First | 1960s | Thick shell Thick, viscous gel Dacron patch |
| Second | 1970s | Thin shell Less viscous gel No patch |
| Third | 1980s–1992 | Thick, silica-reinforced barrier coat shells |
| Fourth | 1992–present | Stricter manufacturing standards Refined version of 3rd-generation implants |
| Fifth | 1993–present | Cohesive silicone gel–filled devices Form stable devices, with textured outer shell |
On June 14, 2013, the Food and Drug Administration (FDA) approved the MemoryShape breast implant (Mentor Worldwide, Santa Barbara, CA, USA), making it 1 of 3 approved cohesive gel implants in the United States. The implant was known as the “gummy bear” implant to the general public as it was going through the testing and approval process. Unlike past round gel implants, the MemoryShape implant has a teardrop shape intended to provide a natural-shaped breast with preferential fullness of the lower pole ( Fig. 7 ). The gel is highly cohesive secondary to increased cross-linking, leading to enhanced firmness and shape retention. Other similar implants with slight variations are made by Sientra and Allergan for use in the United States.
Early experience with these implants suggests that they provide a few advantages relative to round gel implants, including a more natural shape and less rippling. These implants, however, are firmer to the touch, require larger incisions for insertion, and occasionally rotate within the breast pocket resulting in an abnormal contour of the reconstructed breast. Implant malrotation may occur despite external shell texturing and precise pocket creation, 2 measures intended to limit implant movement.
Breast Implants and Anaplastic Large Cell Lymphoma
The relationship between implants and breast surgery has been somewhat tumultuous with the moratorium on silicone gel implants in the 1990s and more recently a possible association with a type of lymphoma. In January 2011, the FDA released a medical device safety communication regarding the possible association between breast implants and the development of anaplastic large cell lymphoma (ALCL), a rare type of non-Hodgkin lymphoma. The FDA reported that women with breast implants may have a very low but increased risk of developing ALCL adjacent to the breast implant compared with women without implants. According to the Surveillance, Epidemiology, and End Results Program of the National Cancer Institute, an estimated 1 in 500,000 women per year in the United States is diagnosed with ALCL, with only 3 in 100 million women diagnosed with the disease in the breast. Globally, there have been approximately 60 cases of ALCL identified in women with breast implants, whereas 5 to 10 million women have received implants worldwide. Currently, additional data is required to fully evaluate the possible relationship between ALCL and breast implants. All cases of ALCL reported in women with breast implants are now tracked in the FDA MedWatch Program.
Autologous Breast Reconstruction
Since Tansini first described the use of a pedicled latissimus dorsi flap in 1906 to reconstruct an anterior chest wall defect, the use of autologous flaps for breast reconstruction has evolved significantly. Today’s arsenal of possible autologous flaps includes pedicled flaps, such as the latissimus dorsi and transverse rectus abdominis myocutaneous (TRAM) flaps, and free flaps, which can be harvested from the abdomen, buttocks, or thighs ( Box 1 ). The trend toward perforator flaps over the past 20 years has also expanded the options for patients desiring reconstruction using their own tissue.