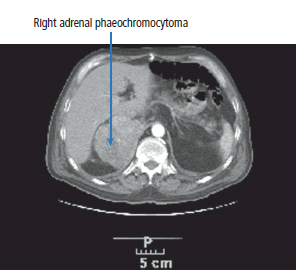
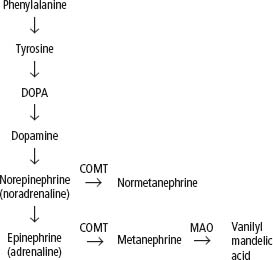
22 Adrenal cortical cancers occur with an incidence of approximately one per million of population per annum. Adrenal cortical cancers are derived from the adrenal cortex and may be secretory. The major adrenal hormone products of these tumours include androgens, aldosterone and cortisol. Serum levels of these hormones may be elevated, and 24-hour urinary cortisol secretion may be increased. Patients with adrenal cortical cancers generally present with non-specific symptoms, such as weight loss and general fatigue, or specific symptoms relating to their anatomical position, which include abdominal or loin pain. Adrenal cortical cancers may also produce symptoms related to the hormones that they secrete. Women may be virilized by the excessive production of androgenic hormones. Occasionally, adrenal cortical cancers are picked up as a result of an abdominal ultrasound or CT scan carried out for another reason. The patient with a suspected diagnosis of adrenal cortical cancer will generally be investigated in an endocrinological or surgical outpatient setting where routine blood testing together with specific endocrinological investigations will be arranged. These will include measurement of the adrenal androgens, adrenocorticotrophic hormone (ACTH) levels, 24-hour urinary cortisol levels, plain X-rays and CT scans of the abdomen, pelvis and chest (Figure 22.1). Once staging investigations have been completed, the patient with a suspected diagnosis of an adrenal cortical cancer should be referred on to a specialist endocrine surgeon. The patient will proceed to laparotomy, and an attempt is made to resect the tumour. Surgery is complex, and there may be a major morbidity and mortality associated with the procedure. There is no clinical advantage to any adjuvant treatment. Figure 22.1 Adrenal tumour. This CT scan was performed on a 28-year-old man with hypertension and shows a lobulated heterogeneous right adrenal mass which was due to phaeochromocytoma. The secretory symptoms of adrenal cortical tumours are unpleasant. Secretory symptoms are most unpleasant in women because of virilization caused by androgenic steroid production. These symptoms may include acne, hirsutism, change in habitus and increased libido. Attempts are made to block the production of hormones by an adrenal cortical cancer, using blocking agents such as metyrapone and ketoconazole, which inhibit steroidogenesis. Treatment may be given using o,p′-dichlorodiphenyl- dichloroethane (o,p′DDD), which is also called “mitotane”. Mitotane is a selective adrenal poison that is structurally related to the chlorinated insecticide dichlorodiphenyltrichloroethane (DDT). DDT is a cheap insecticide developed in the 1940s that has cumulative toxicity in mammals. It is estimated that DDT saved 500 million people globally from malaria. In 1962, however, Rachel Carson published The Silent Spring, in which she attributed the declining songbird population to widespread DDT use, and there have since been calls to ban DDT globally. The alternative insecticides are far more expensive, however, as they remain subject to patents owned by the pharmaceutical industry. Patients with adrenal cortical cancers are also prescribed chemotherapy. Approximately 40% of patients will respond and the most effective agents include doxorubicin, etoposide and cisplatin. The secretory symptoms of adrenal carcinoma can be controlled with octreotide. This agent has no effect on survival and does not lead to reductions in tumour bulk. The wingless-related integration (Wnt) and insulin-like growth factor (IGF) signalling pathways may be dysregulated in adrenal cortical cancers. Cixutumumab, an antibody directed against IGF1-receptor, may have activity in this tumour group, but trials petered out due to poor patient accrual in this rare tumour. The FIRM-ACT trial results suggest that treatment with mitotane, etoposide and cisplatin is the standard of care for patients with metastatic adrenal cortical cancer. The outlook for the majority of patients with adrenal cortical cancers is very poor, except in the patients with localized, small bulk disease. For this group of patients, the expectation is for a 70% chance of complete cure following surgery. For patients with bulky tumours, the expectation is for a median survival of 1 year. Patients with metastatic tumours survive a median period of 4 months. These uncommon tumours occurring in association with multiple endocrine neoplasia are a rare cause of hypertension. Phaeochromocytomas of the adrenal medulla produce their effects by the secretion of catecholamines, resulting in intermittent, episodic or sustained hypertension, anxiety, tremor, palpitations, sweating, flushing, headaches, gastrointestinal disturbances and polyuria. Twenty-four-hour urinary collection for urinary free catecholamines (epinephrine, norepinephrine and dopamine) is now the most widely employed diagnostic test, although some centres also measure catecholamine metabolites such as metanephrines and vanillylmandelic acid (VMA). In 15% of patients with phaeochromocytomas, there may be changes in the RET, VHL and succinic dehydrogenase subunit B and D genes. Not a lot of people know about this, and the authors of this textbook are numbered amongst the ignorant. The treatment is surgical, and the results of treatment are generally excellent. Metastatic phaeochromocytoma may be treated with 131I-MIBG (meta-iodobenzyl guanidine), a catecholamine precursor, which may also be used to image the tumour (see also Chapter 45). Treatment is generally only successful in those patients with small volume disease owing to the limited penetration of the ionizing radiation. Figure 22.2 Synthesis and breakdown of catecholamines. COMT, catechol o’methyl transferase; MAO, monoamine oxidase. Case Study: The Lebanese man with a sweet tooth.
Adrenal cancers
Epidemiology of adrenal cortical cancers
Presentation of adrenal cortical cancers
Investigations of adrenal cortical cancers
Initial treatment of adrenal cortical cancers
Treatment of metastatic or locally advanced adrenal cortical cancer
Prognosis of adrenal cortical cancers
Adrenal medullary tumours
 ONLINE RESOURCE
ONLINE RESOURCE
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


