© Springer International Publishing AG 2017
Gokhan Ozyigit and Ugur Selek (eds.)Principles and Practice of Urooncologyhttps://doi.org/10.1007/978-3-319-56114-1_1717. Adjuvant or Salvage Radiotherapy in Postoperative Prostate Cancer
(1)
Department of Radiation Oncology, Koc University, Istanbul, Turkey
(2)
Department of Radiation Oncology, The University of Texas, MD Anderson Cancer Center, Houston, TX, USA
Abstract
Prostate-specific antigen (PSA) screening increased the diagnosis of prostate cancer at a localized stage to be treated with a curative intent; approximately half of them undergo radical prostatectomy, and roughly one third of surgically treated patients are expected to experience a recurrence in 10 years’ follow-up. Once PSA failure occurs, many develop distant metastases at a median of 8 years and afterward followed by cancer-related death at a median of 5 years. Biochemical failure risk after radical prostatectomy is mainly expected mostly in men with any of the following features: detectable postoperative PSA, positive surgical margins , extraprostatic extension of tumor (T3a), seminal vesicle invasion (T3b), and Gleason score ≥ 8. The radiotherapy in the undetectable PSA environment (<0.01 ng/mL) within 4 months after prostatectomy is termed as “adjuvant, ” while radiotherapy in rising PSA within any time after prostatectomy is defined as “salvage. ”
Keywords
Prostate cancerAdjuvant radiotherapySalvage radiotherapy17.1 Introduction
Prostate cancer is the most frequent malignancy in males and a major cause of cancer-related mortality [1, 2]. Prostate-specific antigen (PSA) screening increased the diagnosis of prostate cancer at a localized stage and, therefore, treatment with a curative intent. Approximately half of the men with localized disease undergo radical prostatectomy, and roughly one third of these are expected to experience a recurrence within 10 years’ time [3, 4]. Once PSA failure occurs, the median time to distant metastasis is 8 years followed by prostate cancer-related death at a median of 5 years [5]. Biochemical failure risk after radical prostatectomy increases with the following features: detectable postoperative PSA , positive surgical margins , extraprostatic extension of tumor (T3a), seminal vesicle invasion (T3b), and Gleason score ≥ 8 [3, 6, 7]. Postoperative radiotherapy with undetectable PSA (<0.1 ng/mL) within 4 months of surgery is defined as “adjuvant, ” while radiotherapy for rising PSA at any point after prostatectomy is referred to as “salvage. ”
There have been ongoing arguments as to whether patients with unfavorable disease features benefit from adjuvant therapy and as to when the window of opportunity for salvage treatment is greatest. The American Society of Clinical Oncology Clinical Practice Guideline Endorsement in 2014 sought to clarify the confusion on four fundamentals: patient counseling, adjuvant versus salvage radiotherapy settings, an acceptable definition of biochemical recurrence , and the restaging evaluation [8].
The preference for salvage radiotherapy is based on allowing enough time for post-prostatectomy urinary and erectile function recovery, avoiding potentially unnecessary radiotherapy in a large group of patients and avoiding radiotherapy-related toxicity. Accumulation of retrospective knowledge from prostatectomy series has provided patterns of relapse and valuable information by which to define patients at high risk of recurrence in order to rationalize therapeutic measures [5, 9, 10]. A recent update of the Stephenson nomogram by Tendulkar et al. has been published on multi-institutional outcomes for salvage radiotherapy (SRT) derived from 2460 node-negative patients with a detectable post-RP PSA treated with SRT with or without concurrent androgen-deprivation therapy (ADT) with a median follow-up of 5 years [11]. Overall, the pathologic features of positive surgical margins (58%), extraprostatic tumor extension (T3a, 56%), seminal vesicle invasion (T3b, 18%), Gleason score (76%: 7, 56%; 8, 10%; 9–10, 9%), and pre-radiation PSA levels were significantly associated with biochemical failure-free survival at 5 years after treatment.
Most of the biopsy-proven biochemical failures occur in the prostate or seminal vesicle bed [12, 13]. Connolly et al. analyzed the characteristics of local recurrence after radical prostatectomy in 114 patients with an elevated PSA and a negative bone scan using ultrasound-guided prostate fossa biopsies . The authors concluded that the majority of the recurrences were at the anastomosis (66%), the bladder neck (16%), and posterior to the trigone (13%) [12]. Furthermore, the examination of pathological details demonstrated that local recurrences are associated with organ-confined disease just 20% of the time but with positive surgical margins in 66% of patients. (Leventis et al. also evaluated the accuracy of transrectal ultrasonography-guided prostatic fossa biopsy in the detection of local recurrence in their 99 patients with biochemical recurrence after radical prostatectomy [13]; they revealed positive biopsies in more than half of the suspected lesions at the urethrovesical anastomotic area and bladder neck in addition to rare lesions in the retrovesical space.) Instead of this reference which basically says that + bx is 50/50, you may want to quote the reference from MDA—Jingya Wang—Practical Radiation Oncology which looks at the location of bx-proven local recurrences on MRI and creates a map. This would go along with the Connolly reference above.
In the Johns Hopkins Hospital radical prostatectomy series of 1997 patients operated on between 1982 and 1997, 15% of the cohort recurred mainly in the first 5 years after prostatectomy and 34% with metastatic disease [5]. Three key pathologic and clinical factors delineated those likely to develop metastases: Gleason scores of 8–10, ≤2 years’ time to PSA recurrence, and ≤10 months PSA doubling time (PSADT). This study led to the clinical question as to whether a therapeutic salvage intervention might decrease the risk of metastases in these patients [9, 10]. Stephenson et al. retrospectively reviewed 501 salvage radiotherapy patients treated between 1987 and 2002 at five US academic centers and concluded that in multivariate analysis, poor response after salvage radiotherapy was directly related to these prognostic predictors of progression: Gleason score (8–10, hazard ratio [HR], 2.6), pre-radiotherapy PSA level (>2.0 ng/mL,HR, 2.3), surgical margins (negative margins, HR, 1.9), PSADT (10 months or less, HR, 1.7), and seminal vesicle invasion (HR, 1.4) [9]. Progression-free probability (PFP) of patients without adverse features was 77% at 4 years, treatment of early recurrence (PSA level ≤ 2.0 ng/mL) documented PFP of 64% for positive surgical margins and of 22% for negative margins in patients with Gleason scores ≤7 and a rapid PSADT, and PFP of 81% for longer PSADT and of 37% for shorter PSADT in patients with Gleason scores of ≥8 and positive margins [9].
Trock et al. retrospectively studied a cohort of 635 biochemically recurrent patients who had radical prostatectomy between 1982 and 2004; 397 patients had no salvage treatment, 160 were treated with radiotherapy alone, and 78 had radiotherapy plus hormonal therapy [10]. Salvage radiotherapy alone was shown to improve cancer-specific survival (PCSS) threefold (HR, 0.32) in comparison to no salvage treatment, while no benefit for adding hormonal therapy to radiotherapy was detected. The patients with improved PCSS after salvage radiotherapy had PSADT <6 months which remained significant in multivariate analysis. Delayed salvage radiotherapy, more than 2 years after recurrence, did not provide any benefit in PCSS in this cohort. Likewise, patients whose PSA did not become undetectable after salvage radiotherapy had no survival gain. In Duke cohort of 519 patients with biochemical failure after prostatectomy analyzed by Cotter et al., salvage radiotherapy was significantly associated with longer overall survival both in PSADT of <6 months and ≥6 months [14].
Since retrospective data points to the frequent need for salvage radiation in patients with high-risk features, prospective data would be helpful in determining who would benefit most from adjuvant radiotherapy. Three prospective randomized clinical trials, Southwest Oncology Group (SWOG) 8794 , European Organization for Research and Treatment of Cancer (EORTC) 22,911 , and Arbeitsgemeinschaft Radiologische Onkologie (ARO) 9602 , have been published comparing adjuvant postoperative RT versus observation in radical prostatectomy patients who had adverse pathologic features: positive margins, extracapsular extension, or seminal vesicular invasion [15–21]. These publications led to the joint guidelines of both the American Society for Radiation Oncology (ASTRO) and the American Urological Association (AUA) which encourage consideration of adjuvant radiotherapy in case of these adverse pathologic findings and also salvage radiotherapy in patients with post-prostatectomy PSA recurrence or local recurrence without distant metastasis [3, 22].
17.2 Randomized Adjuvant Radiotherapy Trials
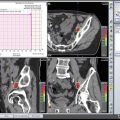
All three adjuvant radiotherapy randomized trials treated intermediate or high-risk disease patients delivering radiotherapy to the prostatic fossa encompassing the vesicourethral anastomosis , the bladder neck, and the area posterior to the trigone, with 60 Gy in 30 fractions (64 Gy allowed in SWOG 8794 ). Primary end points varied: metastasis-free survival in SWOG, local control, and clinical progression-free survival in EORTC 22911 and progression-free survival in ARO. All now have long-term follow-up, >9 years. The most recent trial, ARO 9602 (307 patients), did not allow accrual of patients with detectable PSA at the time of postoperative RT as did SWOG 8794 (425 patients) and EORTC 22911 (1005 patients) [15–18]. Approximately one third of patients in SWOG 8794 and one out of eight to ten patients in EORTC 22911 had a pre-radiation PSA ≥ 0.2 ng/mL, while ARO 9602 only included patients with “undetectable PSA” values <0.1 ng/mL [19–21]. The treatment technique was conventional RT with three or four fields in SWOG 8794 (between 1988 and 1997) and EORTC 22911 (between 1992 and 2001), while 3D-CRT planning was done in ARO 9602 (between 1997 and 2004).
Thompson et al. reported on SWOG 8794 [15, 16] with a median follow-up of more than 12 years in the most recent publication showing a significant improvement at 10 years with postoperative radiotherapy in comparison to observation alone in overall survival (74% vs. 66%; HR 0.72; p = 0.023) and in metastasis-free survival (71% vs. 61%; HR 0.71; p = 0.016). Freedom from biochemical failure (absence of a rise in PSA to >0.4 ng/mL) at 5 years was also improved significantly with postoperative radiotherapy (70% vs. 45%). Salvage hormonal therapy was given to 21% of patients in the observation arm and to only 10% in the radiotherapy arm, whereas salvage radiotherapy was applied after failure to 33% of patients in the observation arm such that some say this was actually a comparison of early versus late radiation. The reported toxicity in the SWOG trial was 11.9% in the observation arm (urethral strictures, 9.5%; total urinary incontinence, 2.8%) and 23.8% in the treatment arm (rectal, 3.3%; urethral strictures, 17.8%, RR 1.9, p = 0.02; total urinary incontinence, 6.5%, RR 2.3, p = 0.11).
Bolla et al. published EORTC 22911 [17, 18] noting a significant improvement at 10 years in biochemical progression-free survival (absence of a rise in PSA of >0.2 ng/mL over post-radiotherapy nadir), 60.6% vs. 41.1%, HR 0.49; p < 0.0001, in locoregional control (cumulative relapse rate, 7.3% vs. 16.6%, HR 0.45; p < 0.0001), and in distant metastases-free survival (cumulative metastasis rate, 10.1% vs. 11.0%, HR 0.99; p = 0.94). No significant difference in 10 year in OS was seen (76.9% vs. 80.7%, HR 1.18; p = 0.2024), and there was no difference in prostate cancer-specific mortality rates (3.9% vs. 5.4%, HR 0.78; p = 0.3407). One third of the patients in observation arm were salvaged with radiotherapy, while salvage hormonal therapy rates at 5 years were 10.1% in the radiotherapy arm and 15.5% in observation arm. Toxicity in the EORTC trial was higher as expected in postoperative RT arm (cumulative any-grade toxicity, 70.8% vs. 59.7%, p = 0.001). Most toxicities were grades 1–2, and none were grade 4. Grade 3 toxicity at 10 years with postoperative radiotherapy was 5.3% in comparison to 2.5% in the observation arm (p = 0.052).
ARO 9602 [19–21] showed a significant improvement for adjuvant radiation in 10 year progression-free survival (progression defined as two consecutive PSA rises), 56% vs. 35%, p < 0.0001, but no significant difference in metastasis-free or overall survival as SWOG 8794 did. There was a third reported arm in the ARO study which was excluded from randomization: 74 patients with persistent PSA (median 0.6, range 0.05–5.6 ng/mL) after prostatectomy. These patients received 66 Gy to the prostate bed at a median of 86 days after surgery [20]. In comparison to patients with an undetectable PSA, this group had significantly worse outcomes with a poorer 10 year metastasis-free survival (67% vs. 83%) and overall survival (68% vs. 84%). For the randomized patients, multivariate Cox regression analysis defined risk factors for progression as Gleason score ≥ 8 (HR 2.8), pT ≥ 3c (HR 2.4), and extraprostatic extension ≥2 mm (HR 3.6). ARO 9602 reported that there was no grade 4 acute toxicity and very low grade 3 acute toxicity associated with radiotherapy (single event bladder toxicity, 1/148 0.7%) and higher but acceptable late grade 1–2 toxicity with radiotherapy (late grade 1–2 genitourinary toxicity: 15.5% vs. 2.5%; late grade 1–2 gastrointestinal toxicity: 10.8% vs. 3.1%).
In summary, the SWOG trial asserted that adjuvant radiation reduced metastases and improved overall survival, although the other two trials, EORTC and ARO, with roughly 10 years of follow-up, revealed no such benefit in either end point. The SWOG study critics make the argument that a significant number of patients in the observation arm received later, salvage radiotherapy when the median PSA was >1 ng/mL and that this may have served to decrease the survival difference between the two randomized groups. Ongoing trials will answer the question whether early radiation for rising PSA is equivalent to adjuvant radiation: RADICALS (radiotherapy and androgen deprivation in combination after local surgery) [23], RAVES (radiotherapy–adjuvant versus early salvage) [24, 25], and GETUG-17 (Groupe d’ Étude des Tumeurs Uro-Génitales) [26].
17.3 Nomograms and Systematic Reviews
Stephenson et al. retrospectively studied the outcomes with salvage radiotherapy in a multi-institutional cohort of 501 patients from five US academic centers [9]. In patients treated between 1987 and 2003 for detectable and rising PSA with a median follow-up of 45 months, the 4 year progression-free probability (PFP) was 77% if no adverse features were present in comparison to 45% for the entire cohort. Multivariable analysis defined the following predictors of progression as after radiation: Gleason score of ≥8 (HR, 2.6, p < 0.001), pre-radiotherapy PSA ≥2.0 ng/mL (HR, 2.3, p < 0.001), negative surgical margins (HR, 1.9, p < 0.001), PSA doubling time (PSADT) ≤10 months (HR, 1.7, p = 0.001), and seminal vesicle invasion (HR, 1.4, p = 0.02). Earlier salvage radiation in patients with PSA ≤2.0 ng/mL, Gleason score ≤ 7, and a rapid PSADT provided better PFP at 4 years, 64%, if surgical margins were positive as compared to negative, 22%. Earlier salvage radiation in patients with PSA ≤2.0 ng/mL, Gleason scores ≥8, and positive margins produced better PFP outcome at 4 years, 81%, if PSADT was >10 months as compared to ≤10 months, 37%.
Stephenson et al. updated their analysis in a multi-institutional cohort of 1540 patients using multivariable Cox regression analysis to construct a model to predict the disease progression probability after salvage radiation [27]. The resultant nomogram produced the following significant variables: PSA level before salvage radiation(p < 0.001), prostatectomy Gleason score (p < 0.001), PSADT (p < 0.001), surgical margins (p < 0.001), androgen ablation before or during salvage radiotherapy (p < 0.001), and nodal disease (p = 0.019); the concordance index was 0.69. Salvage radiotherapy administered at the earliest sign of PSA recurrence seemed to provide a long-term PSA response in nearly half of the patients, while higher PSA levels at the time of salvage radiotherapy were found to be detrimental, and in fact PSA levels of ≥1.25 ng/mL carried a high risk of pathologic nodal metastasis [27].
King et al. also studied the timing of salvage radiotherapy in their systematic review of 41 studies containing 5597 patients in order to define the factors associated with relapse-free survival (RFS) [28]. Importantly, PSA level before salvage radiotherapy (p < 0.0001) as well as radiotherapy dose (p = 0.0052) was found to be significantly and independently associated with RFS with an average 2.6% loss in RFS for each incremental 0.1 ng/mL PSA increase prior to salvage radiotherapy. The authors noted that a PSA level of ≤0.2 ng/mL would ensure RFS of approximately 64%. Additionally, although less robust on sensitivity analysis, the salvage radiotherapy dose was important and defined by a sigmoidal dose-response curve which showed a 2% per Gy incremental improvement in RFS such that the RFS was 54% with a dose of 70 Gy but 34% with a dose of 60 Gy. This publication encouraged initiating salvage radiotherapy at the lowest possible PSA level leading to the question of early salvage radiation being equivalent to adjuvant therapy [28]. Tendulkar et al. recently published a contemporary update of the Stephenson nomogram which included 2460 node-negative patients with a median follow-up of 5 years treated with salvage radiotherapy at ten academic institutions. This work also concluded that early salvage radiotherapy at low PSA levels, especially ≤0.2 ng/mL, was significantly associated with improved freedom from biochemical failure and distant metastasis [11].
Fossati et al. recently published a retrospective review of a multi-institutional cohort of 716 node-negative patients with undetectable PSA after radical prostatectomy who subsequently experienced a PSA rise and were salvaged with early radiotherapy to the prostate and seminal vesicle bed while the PSA was still ≤0.5 ng/mL [29]. Biochemical relapse-free survival at 5 years was 82%, and in multivariable Cox regression analysis, the pre-salvage radiotherapy PSA level was very significantly associated with biochemical relapse after salvage (HR: 4.89; p < 0.0001). When stratified according to the following three pathological risk factors, ≥pT3b, Gleason score ≥ 8, and negative surgical margins, each incremental 0.1 ng/mL of PSA rise increased the risk of PSA recurrence. At 5 years after treatment, patients with ≥2 risk factors had a PSA recurrence risk of 10% as compared to only 1.5% in patients with 0–1 factor. Salvage radiotherapy at the earliest PSA rise conferred better biochemical control in patients with more adverse pathologic features although the benefit of very early salvage radiotherapy was less evident with favorable disease at radical prostatectomy.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree