SUMMARY
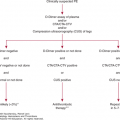
Acquired qualitative platelet disorders are frequent causes of abnormal platelet function measured in vitro, although by themselves, they are usually associated with little or no clinical bleeding. However, there are important exceptions. Nevertheless, their major clinical impact becomes apparent in the additional presence of thrombocytopenia or additional acquired or congenital disorders of hemostasis. Acquired disorders of platelet function can be conveniently classified into those that result from drugs, hematologic diseases, and systemic disorders. Drugs are the most frequent cause of acquired qualitative platelet dysfunction. Aspirin is the most notable drug in this regard because of its frequent use, its irreversible effect on platelet prostaglandin synthesis, and its documented effect on hemostatic competency, although this effect is minimal in normal individuals. Other nonsteroidal antiinflammatory drugs reversibly inhibit platelet prostaglandin synthesis and usually have little effect on hemostasis. The antiplatelet effects of a number of drugs have proven useful in preventing arterial thrombosis, but as would be anticipated, excessive bleeding can be a complication of their use. In addition to aspirin, these drugs include the P2Y12 adenosine diphosphate receptor antagonists, clopidogrel, prasugrel and ticagrelor, vorapaxar, an inhibitor of the PAR1 thrombin receptor, and drugs that specifically inhibit adhesive ligand binding to platelet integrin αIIbβ3 (GPIIb/IIIa). Other drugs used to treat thrombosis, such as heparin and fibrinolytic agents, may also impair platelet function in vitro and ex vivo, but the clinical significance of these observations is uncertain. High doses of the β-lactam antibiotics can impair platelet function in vitro, whereas clinically significant bleeding is unusual in the absence of a coexisting hemostatic defect. Similarly, a number of miscellaneous drugs, including a variety of psychotropic, chemotherapeutic, and anesthetic agents, as well as a number of foods and food additives, can affect platelet function in vitro but do not appear to be of clinical significance by themselves. Hematologic diseases associated with abnormal platelet function include marrow processes in which platelets may be intrinsically abnormal such as the myeloproliferative neoplasms, leukemias, and myelodysplastic syndromes; dysproteinemias in which monoclonal immunoglobulins can impair platelet function; and acquired forms of von Willebrand disease. Of the systemic diseases, renal failure is most prominently associated with abnormal platelet function because of the retention in the circulation of platelet inhibitory compounds. Platelet function may also be abnormal in the presence of antiplatelet antibodies, following cardiopulmonary bypass, and in association with liver disease or disseminated intravascular coagulation.
Acronyms and Abbreviations:
ADP, adenosine diphosphate; BCNU, bis-chloroethylnitrosourea; BTK, Bruton tyrosine kinase; cAMP, cyclic adenosine monophosphate; cGMP, cyclic guanosine monophosphate; COX, cyclooxygenase; coxibs, COX inhibitors; CYP, cytochrome P; DDAVP, desmopressin or 1-desamino-8-D-arginine vasopressin; DIC, disseminated intravascular coagulation; EPO, erythropoietin; GP, glycoprotein; Ig, immunoglobulin; ITP, immune thrombocytopenia; KGD, lysine-glycine-aspartic acid tripeptide; NO, nitric oxide; NSAID, nonsteroidal antiinflammatory drug; PAR, protease-activated receptor; PCI, percutaneous coronary intervention; PG, prostaglandin; PGI2, prostacyclin; PKC, protein kinase C; RGD, arginine-glycine-aspartic acid tripeptide; SLE, systemic lupus erythematosus; t-PA, tissue plasminogen activator; TTP, thrombotic thrombocytopenic purpura; TXA2, thromboxane A2; VWF, von Willebrand factor.
Platelet function may be adversely affected by drugs and by hematologic and nonhematologic diseases. Because the use of aspirin and other nonsteroidal antiinflammatory agents is pervasive, acquired platelet dysfunction is much more frequent than inherited platelet dysfunction. Acquired disorders of platelet function can be classified according to the underlying clinical conditions with which they are associated (Table 11–1).
Drugs that affect platelet function
|
Hematologic disorders associated with abnormal platelet function
|
Systemic disorders associated with abnormal platelet function
|
It is important to have a balanced view of the clinical significance of acquired disorders of platelet function. On the one hand, their severity is usually mild. On the other hand, there are important exceptions to this rule, particularly when platelet dysfunction is associated with other hemostatic defects. If a patient does not present with a history of bleeding, it may be difficult to predict the risk of future bleeding. This is not surprising since even patients with thrombocytopenia may experience little or no spontaneous bleeding until their platelet count is less than 10 × 109/L. Furthermore, clinical assessment of these disorders is made problematic by difficulties in standardization and interpretation of laboratory tests of platelet function, including platelet aggregometry. These tests are more useful in diagnosing platelet dysfunction than in predicting the risk of bleeding.1,2
Drugs are the most common cause of platelet dysfunction (Table 11–2). For example, in an analysis of 72 hospitalized patients with a prolonged bleeding time (a test no longer considered reliable), 54 percent were receiving large doses of antibiotics known to prolong the bleeding time and 10 percent were taking aspirin or other nonsteroidal antiinflammatory drugs.3 Some drugs can prolong the bleeding time and either cause or exacerbate a bleeding diathesis. Other drugs may prolong the bleeding time but not cause bleeding, while many only affect platelet function ex vivo or when added to platelets in vitro. It is important for the hematologist to understand the clinical significance of these distinctions.
Nonsteroidal antiinflammatory drugs
|
P2Y12 antagonists
|
PAR1 receptor antagonist
|
Integrin αIIbβ3 antagonists
|
Drugs that affect platelet cyclic adenosine monophosphate levels or function
|
Antibiotics
|
Anticoagulants, fibrinolytic agents, and antifibrinolytic agents
|
Cardiovascular drugs
|
Volume expanders
|
Psychotropic drugs and anesthetics
|
Oncologic drugs
|
Miscellaneous drugs
|
Antihistamines
|
Radiographic contrast agent
|
Foods and food additives
|
Aspirin irreversibly inactivates the enzyme cyclooxygenase (COX), also known as prostaglandin endoperoxide H synthase, by acetylating a serine residue at position 529.4 Two isoforms of COX have been identified (COX-1 and COX-2),5 as well as a splice variant of COX-1, COX-1b (COX-3), whose functional significance is uncertain.6 COX-1 is constitutively expressed by many tissues, including platelets, the gastric mucosa, and endothelial cells (Chap. 24 discusses the use of aspirin as an antithrombotic agent).5 COX-2 is undetectable in most tissues, but its synthesis is rapidly induced in cells such as endothelial cells, fibroblasts, and monocytes by growth factors, cytokines, endotoxin, and hormones.5 Platelets express only COX-1, whereas endothelial cells can express both COX-1 and COX-2.7,8 In the cardiovascular system, COX products regulate complex interactions between platelets and the vessel wall. The platelet product of COX-1–mediated prostaglandin synthesis, thromboxane A2 (TXA2), produces vasoconstriction and is a receptor-mediated agonist for platelet aggregation and secretion.4 Thus, inactivation of COX-1 by aspirin prevents platelet synthesis of TXA2, thereby inhibiting platelet responses that depend on this substance. Accordingly, platelet responses to adenosine diphosphate (ADP), epinephrine, low doses of collagen and thrombin, and arachidonic acid are affected (arachidonic acid completely), but there is almost no effect on the responses to higher doses of collagen or thrombin.9,10 On the other hand, the endothelial cell prostaglandin (PG) product, prostacyclin (PGI2), produces smooth muscle cell relaxation and vasodilation and increases the platelet content of cyclic adenosine monophosphate (AMP), thereby decreasing overall platelet reactivity.11
Platelet PG synthesis in an adult is nearly completely inhibited by a single 100-mg dose of aspirin or by 30 mg taken daily for 7 to 10 days.4 Although single doses of aspirin irreversibly inhibit platelet and endothelial cell COX,12 they have no lasting effect on PG synthesis by endothelial cells because of the ability of these cells to synthesize additional COX unaffected by aspirin.13 In vitro studies also suggest that the presence of erythrocytes contributes to agonist-stimulated platelet reactivity,14 an effect that can be inhibited by aspirin at doses greater than those required to inhibit platelet COX-1.15 A meta-analysis of clinical trials indicates that aspirin doses varying from 50 to 1500 mg daily are equally efficacious in preventing adverse cardiovascular and cerebrovascular events.16 This has led many to suggest that the lowest effective doses should be prescribed to minimize gastrointestinal toxicity. Nonetheless, even low doses of aspirin can be associated with significant gastrointestinal hemorrhage.17–19
Aspirin is one of the relatively few drugs that prolongs the bleeding time in humans and appears to do so by blocking aggregation rather than adhesion. In normal individuals, the effect on the bleeding time is slight (generally no more than 1.2 to 2.0 times the preaspirin bleeding time),20,21 is observed in both males and females, and requires that almost all the COX in the circulating platelets be inhibited.11 The sensitivity of the bleeding time to aspirin is dependent on such technical variables as the direction of the incision on the forearm and the degree of hydrostatic pressure applied to the arm,22 and hence the current view that the test is unreliable. The bleeding time may remain prolonged for 1 to 4 days after aspirin has been discontinued, and platelet aggregation tests may remain abnormal for up to a week until platelets affected by aspirin are replaced as the result of thrombopoiesis.23
The significance of aspirin ingestion on the hemostatic competency of normal individuals appears to be minimal. Nevertheless, patients taking aspirin chronically report significant increases in bruising, epistaxis, and gastrointestinal blood loss.17–19 Gastrointestinal blood loss appears to be the result of a direct effect of aspirin on the gastric mucosa.24,25 Furthermore, there is an increase in the incidence of hemorrhagic stroke when aspirin is used in the primary and secondary prevention of vascular disease, as well as an increase in major gastrointestinal and other extracranial bleeding.26 Aspirin may also increase bleeding in the mother and the neonate during parturition.27 In addition, some studies show that aspirin taken preoperatively increases the amount of blood loss following cardiothoracic surgery.28,29 In contrast, a retrospective analysis has documented the safety of performing epidural and spinal anesthesia in patients who had ingested aspirin.30 Aspirin may increase the amount of blood loss following general surgery.31 The significance of aspirin ingestion in this setting was tested in the POISE-2 study32 in which patients at risk for vascular complications were randomized to aspirin or placebo prior to their noncardiac surgery. Although taking aspirin did not reduce the incidence of cardiovascular events, there was a small increase in hemorrhagic complications. This suggests that discontinuing aspirin prior to surgery is a useful practice, particularly prior to plastic or neurosurgical procedures in which the limits of tolerable bleeding are narrow.33 On the other hand, patients taking aspirin and other antiplatelet agents for severe cardiovascular disease may be at risk for thrombosis if these medications are discontinued. Thus, the clinician must thoroughly weigh the potential risks and benefits of discontinuing aspirin prior to noncardiac surgery. This is especially true in patients with other hemostatic disorders; for example, aspirin precipitates hemorrhage in individuals with von Willebrand disease, hemophilia A, warfarin ingestion, uremia, and disorders of platelet function.34–36 Infusion of desmopressin (DDAVP) has been effective in correcting a prolonged bleeding time caused by aspirin.37,38
Resistance to the antiplatelet effects of aspirin (“aspirin resistance”) is a controversial topic, and whether it exists depends to large extent on whether resistance is considered from a biochemical or clinical perspective.39 Biochemical resistance to the platelet-inhibitory effects of aspirin, that is, the failure to achieve pharmacologic inhibition of TXA2 production, is uncommon.39 For example, when healthy subjects were given either standard or enteric-coated aspirin, 49 percent given a single dose of enteric-coated aspirin failed to inhibit TXA2 synthesis, whereas the failure to inhibit TXA2 synthesis was never seen in subjects given standard aspirin.40 Nevertheless, subjects given enteric-coated aspirin eventually responded when taking it daily, implying that although some patients absorb enteric-coated aspirin preparations poorly, they will ultimately absorb sufficient amounts of aspirin to prevent platelet TXA2 synthesis. Most commonly, aspirin resistance occurs because patients are nonadherent with aspirin therapy, often because of gastrointestinal toxicity.41 Clinically, the term aspirin resistance has been applied to patients who develop cardiovascular events despite taking aspirin. Given that aspirin treatment selectively inhibits platelet synthesis of only one endogenous platelet agonist, TXA2, it is not surprising that aspirin does not completely abolish platelet-mediated vascular events.
Unlike aspirin, nonsteroidal antiinflammatory drugs (NSAIDs), such as ibuprofen, naproxen, diclofenac, sulindac, piroxicam, indomethacin, and sulfinpyrazone, reversibly inhibit COX enzymes.42 Although these drugs can cause a transient prolongation of the bleeding time when given in therapeutic doses, this is usually not clinically significant.43 Population studies have suggested that concurrent treatment with NSAIDs and anticoagulants increases the risk of bleeding complication, but many bleeding events were limited to the gastrointestinal tract where NSAIDs are known to induce gastritis and peptic ulcerations.44 As evidence of the modest effect of NSAIDs on platelet function, ibuprofen has been given safely to patients with hemophilia A.45,46 Nonetheless, care must be taken when ibuprofen is given to patients with hemophilia and HIV infection receiving zidovudine because increased bleeding has been reported in this circumstance.47 Because ibuprofen, and probably other NSAIDs, binds to COX-1, blocking its acetylation by aspirin,42 coadministration of NSAIDs and aspirin may impair the irreversible, antithrombotic effects of aspirin on platelets.48 For this reason, patients who require both medications should ingest aspirin at least 2 hours prior to the ingestion of traditional NSAIDs.
COX-1 is present in the gastric mucosa where its products protect the integrity of the gastric lining cells. In inflammatory cells, COX-2 products such as PGE2 and PGI2 elicit an increased sense of pain and perpetuate the inflammatory process.40 Thus, the coxibs (COX inhibitors), designed to be relatively more specific for COX-2 versus COX-1, were intended to reduce pain and inflammation with fewer gastric side effects than traditional NSAIDs.40,42 However, clinical trials revealed that coxib administration was associated with cardiovascular toxicity (myocardial infarction, stroke, edema, exacerbation of hypertension), partly because of inhibiting PGI2 synthesis.11,49–52 On the basis of these results, rofecoxib and valdecoxib were withdrawn from the market (valdecoxib was also associated with cases of Stevens-Johnson syndrome), and a black box warning regarding serious cardiovascular events was added to prescribing information for celecoxib, the only coxib now available in the United States.50 Nonetheless, clinical evidence suggests there is no excess cardiovascular risk from daily doses of celecoxib of 200 mg or less.51 Traditional NSAIDs also inhibit COX-2 to a variable extent, and several observational trials have revealed excess cardiovascular events associated with use of these drugs.50,53–55 Thus, a warning has also been added to their prescribing information. If indicated, analgesics such as acetaminophen, sodium or choline salicylate, and narcotics may be substituted for aspirin and NSAIDs for treating musculoskeletal pain.50 One report suggests that acetaminophen can selectively inhibit COX-2,56 but the clinical significance of this observation is not clear.
Ticlopidine, clopidogrel, and prasugrel are thienopyridines that are used as antiplatelet agents in arterial diseases (Chap. 24) with results at least comparable to aspirin in the secondary prevention of cerebrovascular and cardiovascular events.16,57
Thienopyridines differ from aspirin in their mechanism of antiplatelet activity and their toxicity profile. All three thienopyridines are prodrugs that depend on oxidation by cytochrome P450 (CYP) enzymes in the liver (ticlopidine and clopidogrel) or in liver and intestine (prasugrel) to form the active metabolites that irreversibly inhibit the platelet P2Y12 ADP receptor.58–61 Ticlopidine at 250 mg twice a day, clopidogrel at 75 mg once per day, and prasugrel at 10 mg once a day inhibit platelet aggregation ex vivo in humans. The extent of this effect is equivalent to or greater than that of aspirin, and the effect of thienopyridines and aspirin appears additive.62,63 When given at their usual oral doses, the effect of thienopyridines on platelet aggregation and the bleeding time can be seen within hours of the first dose, but are not maximal for 4 to 6 days. A 300-mg loading dose of clopidogrel or 60 mg of prasugrel, followed by their usual daily doses, shortens the time required for their maximal antiplatelet effect to a few hours.64,65 The common CYP polymorphism CYP2C19 results in lower levels of active clopidogrel and ticlopidine metabolites and has been reported to be associated with decreased platelet inhibition and an elevated risk for major adverse cardiovascular events.55,66,67 Because the enzyme CYP3A is present in the intestine and can oxidize prasugrel to its pharmacologically active metabolite, intestinal metabolism may account for the rapid appearance and higher levels of the active metabolite in plasma after an oral dose.61,68–70 Furthermore, prasugrel metabolism and inhibition of platelet function are not affected by CYP2C19 polymorphisms.61,68–70
The clinical efficacy of prasugrel has been compared to clopidogrel in patients with acute coronary syndrome scheduled for percutaneous coronary intervention in the Triton-TIMI 38 trial. Patients who received prasugrel had a significantly decreased incidence of ischemic events compared to patients who received clopidogrel (9.9 percent vs. 12.1 percent, p <0.001).69 However, major bleeding was also significantly increased in patients receiving prasugrel compared to clopidogrel (2.4 percent vs. 1.8 percent, p <0.03). Thus, although prasugrel appeared to be more efficacious than clopidogrel, this benefit was partially offset by a higher rate of hemorrhage.69
The platelet-inhibitory effects of thienopyridines persist for 4 to 10 days after the drugs have been discontinued, either because of their extended half-life after multiple dosing or their irreversible effect on platelets.58 Ticlopidine administration is associated with potentially serious hematologic complications, including neutropenia (neutrophils <1200 × 109/L in 2.4 percent of individuals)58,71,72 and, less commonly, aplastic anemia and thrombocytopenia.73,74 In addition, at least one in 5000 patients develops a thrombotic thrombocytopenic purpura (TTP)-like syndrome.75–77 Results from a large clinical trial suggest that hematologic complications may be less common with clopidogrel or prasugrel.57 Clopidogrel may also be rarely associated with a TTP-like syndrome (one in 270,000),78 although this rate is close to the TTP incidence in the general population. Because of its toxicity profile, ticlopidine has been replaced by the other thienopyridines in the United States.
Because aspirin and the thienopyridines inhibit platelet function by different mechanisms, their antithrombotic effects may be additive. In theory, this would be beneficial in the treatment of diseases associated with platelet activation such as ischemic heart disease, peripheral vascular disease, and ischemic strokes.62,79,80 This hypothesis was tested in the CURE trial of patients with acute coronary syndromes.62 Although clopidogrel plus aspirin decreased the combined incidence of cardiovascular deaths, myocardial infarctions, and strokes from 11.4 percent to 9.3 percent, the benefit was partially offset by an increase in severe bleeding from 2.7 to 3.7 percent. Similarly, in the CHARISMA trial of a broad population of patients at risk for cardiovascular events, there were 94 fewer ischemic events in patients treated with both clopidogrel and aspirin, but this occurred at the expense of 93 more moderate or severe bleeding events.81 Furthermore, a meta-analysis of seven randomized controlled trials involving more than 39,000 patients confirmed that intracranial hemorrhage was more frequent in patients who received both clopidogrel plus aspirin compared to clopidogrel alone.82 Thus, except for special circumstances such as coronary artery stenting, it appears that the added benefit of dual antiplatelet therapy is small and has the added risk of increased bleeding.83
Ticagrelor, cangrelor, and elinogrel are oral, reversible, nonthienopyridine P2Y12 receptor antagonists. Because they are not prodrugs and do not require metabolic activation, the onset of their inhibitory activity is more rapid than that of the thienopyridines. A novel, and as yet unexplained, side effect of treatment with this class of the P2Y12 antagonists is the occurrence of dyspnea, which can complicate the management of patients with coronary artery disease.84
Ticagrelor, the first drug of the class, has been approved for use in acute coronary syndromes. Its efficacy versus clopidogrel was tested in the PLATO trial in which patients with an acute coronary syndrome were randomized to treatment with either ticagrelor or clopidogrel.85–87 At 1 year, the combined end point of death, myocardial infarction, and stroke was 9.8 percent in patients treated with ticagrelor compared to 11.7 percent in patients treated with clopidogrel.88 Although stent thrombosis was also decreased in the ticagrelor-treated group, major bleeding not associated with coronary artery bypass surgery was increased in this group. The incidence of fatal intracranial hemorrhage was also greater in the ticagrelor-treated patients, but it was a rare event (0.1 percent of treated patients). In the ATLANTIC trial, patients suffering from an ST-segment elevation myocardial infarction were randomized to receive ticagrelor in the ambulance or in the catheterization laboratory.89 Although initiating therapy before hospitalization was safe and lowered the incidence of stent thrombosis, there was no overall improvement in preventing major cardiovascular adverse events. Thus, ticagrelor, like prasugrel, appears to be more efficacious than clopidogrel at preventing adverse cardiovascular events but with more hemorrhagic complications.
Thrombin is the most potent physiologic platelet agonist. Three G-protein–coupled thrombin receptors have been identified in humans (protease-activated receptors [PARs] 1, 3, and 4).90 Although human platelets express both PAR-1 and PAR-4, the major platelet thrombin receptor is PAR-1 and can be activated by nanomolar concentrations of thrombin. PAR-4 signaling appears to be unnecessary for platelet activation if PAR-1 signaling is intact.90 Vorapaxar is a potent, selective, long-acting, oral PAR-1 inhibitor generated from the naturally occurring muscarinic receptor antagonist himbacine.91 A high-resolution crystal structure of vorapaxar bound to PAR-1 revealed that the binding pocket for the drug is unusual for a peptide-activated G-protein–coupled receptor in that it consists of a superficial tunnel with little of the bound drug surface exposed to aqueous solvent, perhaps accounting for the very slow dissociation rate of vorapaxar from PAR-1.92
The efficacy of vorapaxar for the secondary prevention of arterial thrombosis was examined in the phase III TRA 2P–TIMI 50 trial in which patients with a history of myocardial infarction, stroke, or peripheral arterial disease were randomized between vorapaxar and placebo.93 Most patients were also taking either aspirin or a thienopyridine. Because of a high incidence of intracranial bleeding in the first years of the study, entry criteria were modified to eliminate patients with a history of a stroke. At 3 years, the incidence of the primary end point (cardiovascular death, myocardial infarction, and stroke) was significantly reduced in vorapaxar-treated patients (9.3 percent vs. 11.2 percent, p <0.001). However, moderate to severe bleeding, including intracranial bleeding, was significantly increased in the vorapaxar-treated patients (4.2 percent vs. 2.5 percent, p <0.001). Nonetheless, based on efficacy, vorapaxar received FDA approval in 2014. Atopaxar, a second PAR-1 antagonist, is currently being evaluated in clinical trials.94 Atopaxar has a shorter half-life than vorapaxar, suggesting that potential bleeding complications might be easier to manage.
Drugs that specifically impair the function of the major platelet integrin αIIbβ3 (GPIIb/IIIa) have been developed for short-term use as antithrombotic agents in the setting of ischemic coronary artery disease.95,96 Integrin αIIbβ3 mediates platelet–platelet cohesion by binding the divalent ligand fibrinogen, thereby crosslinking the integrin on adjacent platelets, causing the formation of platelet aggregates.97 Thus, integrin αIIbβ3 is a viable therapeutic target to prevent arterial thrombosis. Abciximab, eptifibatide, and tirofiban are three FDA-approved structurally dissimilar integrin αIIbβ3 inhibitors that rapidly impair platelet aggregation. Abciximab is a human-murine chimeric Fab fragment, eptifibatide is a cyclic heptapeptide based on the sequence Lys-Gly-Asp (KGD), and tirofiban is an Arg-Gly-Asp (RGD)-based peptidomimetic. All three drugs have demonstrated efficacy in the management of patients with acute coronary syndromes, particularly in the setting of percutaneous coronary interventions (PCI) where iatrogenic artery wall injury occurs.97
Inherited integrin αIIbβ3 abnormalities cause the bleeding disorder Glanzmann thrombasthenia (Chap. 10).98,99 Thus, it is not surprising that integrin αIIbβ3 antagonists can predispose to bleeding. In EPIC, a clinical trial of abciximab in patients undergoing PCI, 14 percent of patients given abciximab experienced major bleeding compared to 7 percent of patients given placebo.100 However, patients were also given aspirin and heparin. When the heparin dose was decreased in the subsequent EPILOG trial, the incidence of major bleeding in patients receiving abciximab decreased to 2.0 percent compared to 3.1 percent in the control group receiving heparin and aspirin alone.101 Nonetheless, in both EPIC and EPILOG, minor bleeding was significantly more frequent in patients given abciximab and standard-dose heparin compared to patients given standard-dose heparin alone, attesting to the ability of an integrin αIIbβ3 antagonist to impair normal hemostasis. In the PRISM-PLUS trial of tirofiban and the PURSUIT trial of eptifibatide, major and minor bleeding were slightly more frequent in patients receiving the study drug compared to controls.102,103 Similarly, patients receiving the oral integrin αIIbβ3 inhibitors xemilofiban and sibrafiban for 30 and 28 days, respectively, frequently experienced mucocutaneous bleeding similar to that experienced by patients with congenital thrombasthenia.104,105 Although short-term use of the parenteral integrin αIIbβ3 antagonists is often beneficial in patients with acute coronary syndrome or following PCI, paradoxically, the long-term use of oral integrin αIIbβ3 inhibitors was associated with an increase in mortality.106 The cause of this paradoxical effect is not clear but has been attributed by some to an antagonist-induced conformational change in integrin αIIbβ3 simulating the effect of physiologic platelet agonists.107
The risk of bleeding in patients undergoing PCI in the presence of integrin αIIbβ3 antagonists can be minimized by using heparin on a weight basis,101 by avoiding treatment of patients who are receiving warfarin at therapeutic doses, by early vascular sheath removal, and by meticulous care of vascular puncture sites.108 Platelet transfusions can rapidly reverse the platelet function defect in patients receiving abciximab, presumably by decreasing the overall extent of integrin blockade. The ability of platelet transfusion to reverse the effects of the other integrin αIIbβ3 antagonists is less clear, but these drugs have very short half-lives if renal and hepatic function are normal.
Thrombocytopenia occurring within 24 hours of initiating therapy has been observed in small numbers of patients following the administration of all integrin αIIbβ3 antagonists.102,105,108,109 In EPIC, the incidence of platelet counts of less than 100 × 109/L and of less than 50 × 109/L in patients receiving abciximab for the first time was 3.9 percent and 0.9 percent, respectively.109 Thrombocytopenia has also been reported in patients receiving eptifibatide, tirofiban, and a variety of small-molecule RGD- and non–RGD-based integrin αIIbβ3 inhibitors with an incidence of up to 13 percent.102,105,109–113
The mechanism responsible for thrombocytopenia following the administration of these drugs is uncertain but may be related to the presence of preexisting antiintegrin αIIbβ3 antibodies that recognize epitopes exposed by the antagonist or, in the case of abciximab, to murine sequences incorporated into the abciximab Fab fragment.114 The thrombocytopenia usually reverses readily when the drug is stopped, but it may also be reversed by platelet transfusion if clinically indicated.108 Thrombocytopenia in patients receiving integrin αIIbβ3 antagonists must be differentiated from pseudothrombocytopenia as a result of drug-induced platelet clumping, from heparin-induced thrombocytopenia in patients receiving heparin concurrently, and from other causes of thrombocytopenia, depending on the clinical circumstances.115,116 It is important to identify thrombocytopenia early because integrin αIIbβ3 antagonists are administered as long infusions, and the drug should be stopped as soon as true thrombocytopenia has been confirmed. In most cases of profound thrombocytopenia, a platelet count obtained 2 to 4 hours after initiating therapy will provide evidence of a significant decrease in platelet count, although cases of delayed thrombocytopenia have been observed after treatment with abciximab.114
The pyrimidopyrimidine derivative, dipyridamole, inhibits platelet cyclic nucleotide phosphodiesterase, resulting in the intraplatelet accumulation of the inhibitory cyclic nucleotide cyclic AMP (cAMP). Dipyridamole may also inhibit the breakdown of cyclic guanosine monophosphate (cGMP), resulting in potentiation of the platelet-inhibitory effect of nitric oxide.117 Although the platelet-inhibitory effects of dipyridamole are seen in vitro, the clinical utility of dipyridamole has been controversial.118,119 A meta-analysis failed to demonstrate the clinical benefit of adding dipyridamole to aspirin.16 However, many older dipyridamole trials used formulations with limited dipyridamole bioavailability.120 In the European Stroke Prevention Study 2 (ESPS 2), dipyridamole was beneficial in preventing stroke and transient ischemic attack, but there was no difference in mortality between patients taking dipyridamole and placebo or among patients taking dipyridamole plus aspirin compared to either dipyridamole or aspirin alone.121 The basis for the benefit of dipyridamole in the ESPS 2 trial is unclear but could be from a higher dipyridamole dosage or a result of the sustained-release dipyridamole preparation used in the trial.
Intravenous infusions of PGE1, PGI2, or stable PGI2 analogues stimulate platelet adenylyl cyclase, causing an increase in platelet cAMP and a decrease in platelet responsiveness.122 These agents cause a transient inhibition of platelet shape change, aggregation, and secretion. However, their clinical utility is limited by their short half-life and side effects that include peripheral vasodilation.123 Cilostazol, a phosphodiesterase III inhibitor, has been approved in the United States for the treatment of peripheral vascular disease124 and may have utility in the prevention of cardiac stent occlusion.125 Nitric oxide (NO) and organic nitrates such as nitroglycerin inhibit platelet function in vitro, probably by activating guanylyl cyclase, thereby increasing cGMP.126 Their effect on in vivo platelet function is uncertain. High concentrations of caffeine and theophylline also inhibit platelet phosphodiesterases in vitro.
Penicillins contain a β-lactam ring and a unique side chain. Most cause a dose-dependent prolongation of the bleeding time in normal volunteers.127 Because they reduce platelet aggregation and secretion, as well as ristocetin-induced platelet agglutination, they may affect both platelet adhesion and platelet activation. Tests of platelet aggregation are abnormal in 50 to 75 percent of individuals receiving large doses (at least several grams per day) of carbenicillin, penicillin G, ticarcillin, ampicillin, nafcillin, and azlocillin and in 25 to 50 percent of patients taking piperacillin, azlocillin, or mezlocillin.127–129 Differences in the antiplatelet effects of these antibiotics probably relate to differences in blood levels and drug potency. Their effect on platelets is maximal after 1 to 3 days of administration and may remain for several days after the antibiotic has been stopped, suggesting that the effect of these antibiotics on platelets in vivo is irreversible.
Penicillins can impair the interaction of agonists and von Willebrand factor (VWF) with the platelet membrane.130 Indeed, when many penicillins are incubated with washed platelets, albeit at concentrations higher than those attained in vivo, they inhibit the interaction of VWF and agonists, such as ADP and epinephrine, with their platelet receptors.131 The relative in vitro antiplatelet potency of the penicillins correlates well with their lipid solubility and with the inhibitory potency of the isolated side chains.132 Moreover, the inhibitory effect of penicillin G on platelet function in vitro is potentiated by the presence of probenecid.133 When platelet function was tested after intravenous administration of penicillin, oxacillin, or mezlocillin for 3 to 17 days to patients or normal volunteers, irreversible inhibition of agonist-induced aggregation was noted, along with a 40 percent reduction in low-affinity TXA2 receptors.134 Thus, penicillins probably inhibit platelet function by binding to one or more membrane components necessary for adhesive interactions with the vessel wall or for stimulus-response coupling.
Although clinically significant bleeding is associated with the use of carbenicillin, penicillin G, ticarcillin, and nafcillin, it is far less common than prolongation of the bleeding time.127,135 Patients with coexisting hemostatic defects (e.g., thrombocytopenia, vitamin K deficiency, uremia) may be particularly prone to this complication. On the other hand, high doses of penicillin G did not increase gastrointestinal blood loss in a thrombocytopenic rabbit model.136 In our experience, bleeding attributable to antibiotic-induced platelet dysfunction is uncommon and unpredictable. Because β-lactam–induced platelet dysfunction resolves with time following cessation of the drug, this class of drugs should only be considered as a cause of bleeding in the appropriate clinical setting. A similar pattern of platelet dysfunction has been reported with some cephalosporins or related antibiotics, but not with others.127,137,138 Broad-spectrum antibiotics can also cause a bleeding diathesis attributable to killing of gut flora, resulting in vitamin K deficiency. Nitrofurantoin, a structurally unrelated antibiotic, may cause a mild prolongation of the bleeding time and impair platelet aggregation when blood levels of the drug are higher than 20 μM, as may occur in patients with renal insufficiency.139 Miconazole, an antifungal agent, inhibits human and rabbit platelet COX in vitro and rabbit platelet COX after intravenous infusion.140
Heparin predisposes to bleeding primarily through its anticoagulant effect, but it may also impair platelet function. For example, a bolus injection of heparin (100 U/kg) can cause a significant prolongation of the bleeding time in normal subjects and in patients prior to cardiopulmonary bypass, suggesting that therapeutic doses of heparin may impair platelet function.126 Heparin likely impairs platelet function by inhibiting the generation and action of the potent platelet agonist thrombin. On the other hand, in vitro studies suggest that heparin can enhance platelet aggregation induced by other platelet agonists.141 Heparin binds to a single class of high-affinity binding sites on resting platelets and to an additional class of lower-affinity binding sites on fully activated platelets.142 High heparin doses also impair VWF-dependent platelet function, possibly by binding to the heparin-binding domain of VWF.143 The contributions of these effects on platelet function to the bleeding complications of heparin therapy are uncertain.
Bleeding during fibrinolytic therapy is predominantly a result of the combined effects of structural lesions in blood vessels and the fibrin(ogen)olytic activity of the agent used. However, pharmacologic doses of streptokinase, urokinase, and tissue plasminogen activator (t-PA) can affect platelet function.144 High concentrations of plasmin ex vivo cause platelet aggregation.145 Moreover, marked increases in the urinary excretion of the TXA2 metabolite 2,3-dinor-TXB2 have been detected in patients receiving streptokinase or t-PA for coronary thrombolysis, suggesting that in vivo platelet activation had occurred during infusion of the drug.146,147 Nevertheless, several in vitro studies indicate that plasmin generation has an inhibitory effect on platelet function. First, very high levels of fibrin(ogen) degradation products, coupled with very low levels of fibrinogen, may impair platelet aggregation.148 Second, plasminogen can bind to platelets149 and, after its conversion to plasmin, enzymatically degrade platelet glycoprotein (GP) Ib, impairing the interaction of platelets with VWF.150,151 Third, plasmin can inhibit platelet arachidonic acid metabolism.152 Fourth, t-PA promotes the disaggregation of platelet aggregates, presumably by inducing lysis of the fibrinogen that mediates aggregate formation.153 Finally, after initial activation, platelets incubated with plasmin and recombinant t-PA in vitro become refractory to activation by other agonists.154 Whether any of these in vitro and ex vivo observations apply to the in vivo situation and are clinically significant remains uncertain.155 The antifibrinolytic drug ε-aminocaproic acid can increase the bleeding time when administered for several days at doses of 24 g/d or greater.150
Administration of nitroprusside, which increases platelet cGMP,156–160 nitroglycerine,161 and propranolol,162,163 can decrease platelet aggregation and secretion ex vivo. Nitroprusside can increase the bleeding time twofold when administered at infusion rates of 6 to 8 mcg/kg/min.156,164 Inhalation of NO advocated for the treatment of pulmonary hypertension and the adult respiratory distress syndrome, can impair agonist-induced platelet aggregation ex vivo, although the clinical significance of these observations is unclear.165–167 Calcium channel blockers such as verapamil, nifedipine, and diltiazem inhibit platelet aggregation when added at very high concentrations to washed platelets.123 This effect is seen primarily with epinephrine-induced aggregation and does not appear to be related to calcium channel blockade.168 At therapeutic doses, calcium channel blockers do not prolong the bleeding time, although one agent, nisoldipine, has been reported to inhibit agonist-induced calcium transients and platelet aggregation after 10 days of oral administration.169 At high concentrations, the antiarrhythmic drug quinidine has been reported to cause a mild prolongation of the bleeding time and to potentiate the effect of aspirin.170
Dextran is a neutral polysaccharide that is heterogeneous in molecular size. Two preparations with average molecular weights of 40,000 and 70,000 are in clinical use. Although dextran infusions may prolong the bleeding time of normal subjects and patients with von Willebrand disease, this phenomenon has not been observed in most normal subjects.9,171,172 Infused dextran adsorbs to the platelet surface and can impair platelet aggregation, secretion, and procoagulant activity. The maximal effect of dextran may require several hours, suggesting that larger molecules with a slower rate of clearance are responsible.9 Curiously, the drug has no effect when added to platelet-rich plasma.9 Dextran infusion produces a modest reduction in plasma VWF antigen levels and ristocetin cofactor activity.171 Despite these effects on primary hemostasis, prospective studies indicate that dextran is not associated with significant postoperative bleeding, unless it is administered together with low-dose heparin.173,174 Hydroxyethyl starch, another volume expander, while generally safe, may prolong the bleeding time and predispose to hemorrhage, particularly if it is administered in doses exceeding 20 mL/kg of a 6 percent solution. Lower doses of hydroxyethyl starch may contribute to bleeding if administered simultaneously with low-dose heparin or if given to patients with preexistent hemostatic defects or after major cardiothoracic surgery.175–178 Different hydroxyethyl starch preparations vary in the average number of hydroxymethyl groups per glucose unit, and this may affect both intravascular survival and effects on hemostasis.179,180
Platelets from patients taking antidepressants or phenothiazines may exhibit impaired aggregation, but this is not associated with bleeding.181,182 The effect on aggregation has been attributed to inhibition of intracellular signaling molecules such as protein kinase C (PKC).183 Selective serotonin reuptake inhibitors, such as paroxetine, have been shown to decrease platelet serotonin storage.184 Fluoxetine does not appear to impair platelet aggregation in vitro and has only rarely been associated with clinical bleeding.185,186 General anesthesia with halothane or propofol may cause a slight prolongation of the bleeding time, most likely the result of an effect on calcium signaling, but this has no adverse effect on surgical hemostasis.187,188 In addition to an association with thrombocytopenia, cocaine has been reported to either inhibit189,190 or stimulate platelet activation.191 It has been suggested that heroin decreases platelet NO production.192 The clinical relevance of these observations is unknown.
Administering mithramycin to a total dose of 6 to 21 mg decreases platelet aggregation and is associated with mucocutaneous bleeding.193 An ex vivo defect in platelet secretion and secondary aggregation has been reported in patients with solid tumors within 48 hours of receiving infusions of autologous marrow and high-dose chemotherapy consisting of cisplatin, cyclophosphamide, and either bis-chloroethylnitrosourea (BCNU; carmustine) or melphelan.194 Both daunorubicin and BCNU can inhibit platelet aggregation and secretion when added to platelet-rich plasma, but they have not been shown to cause clinically significant platelet dysfunction.195–197 Administration of recombinant forms of thrombopoietin to thrombocytopenic patients with cancer results in the production of normally functioning platelets.198,199 Dasatinib, the broad-spectrum protein tyrosine kinase inhibitor, impairs collagen-induced platelet activation in vitro and increases tail bleeding times in mice, perhaps explaining some bleeding episodes in patients with chronic myelogenous leukemia who have been treated with the drug.200 Ibrutinib, a Bruton tyrosine kinase (BTK) inhibitor efficacious in a wide variety of lymphoid malignanies,201,202 is associated with hemorrhagic complications in up to half of patients, with significant hemorrhagic toxicity in 5 percent.201–203 Exposing platelets to ibrutinib ex vivo can produce defective platelet adhesion.204 Furthermore, humans or mice lacking BTK have impaired ex vivo platelet function, although the impairment is quite mild.205,206 Whether the hemorrhagic toxicity of ibrutinib is caused by platelet BTK inhibition or by an off-target effect remains to be determined.
The immunosuppressive drug cyclosporine has been reported to enhance ADP-stimulated platelet aggregation in vitro.207 It is unclear whether this contributes to the TTP-like syndrome associated with this drug. Antihistamines,208 the serotonin antagonist ketanserin,209 and certain radiographic contrast agents210,211 can impair platelet aggregation responses ex vivo by unknown mechanisms.
Certain foods and food additives affect platelet function in vitro, and it is conceivable that some may affect hemostasis, particularly in association with other hemostatic defects. For example, diets rich in fish oils containing ω-3 fatty acids (eicosapentaenoic acid, docosahexaenoic acid) cause a slight prolongation of the bleeding time.212 These fatty acids act by reducing the platelet content of arachidonic acid and by competing with arachidonic acid for COX.213,214 Easy bruising noted after eating Chinese food has been attributed to an antiplatelet effect of the black tree fungus.215 A component of extract of onion can inhibit platelet arachidonic acid metabolism.216 Ajoene, a component of garlic, is an inhibitor of fibrinogen binding and platelet aggregation.217 Extracts of two commonly used spices, cumin and turmeric, also inhibit platelet aggregation and eicosanoid biosynthesis.218
Bleeding and thrombosis are significant causes of morbidity and mortality in the chronic myeloproliferative neoplasms, particularly in essential thrombocythemia, polycythemia vera, and primary myelofibrosis.219–221 Thrombocytosis is a constant finding in essential thrombocythemia, but the differential diagnosis includes these other myeloproliferative neoplasms, including chronic myelogenous leukemia, as well as other diseases associated with reactive thrombosis (Chap. 9).222,223 Most of the information about platelets, bleeding, and thrombosis in the myeloproliferative neoplasms comes from studies of essential thrombocythemia and polycythemia vera.
Several factors contribute to the hemostatic abnormalities in the myeloproliferative neoplasms: (1) Increased whole-blood viscosity in polycythemia vera: The engorgement of blood vessels associated with polycythemia is a risk factor for thrombosis and bleeding, particularly in postoperative situations.224–226 (2) Intrinsic defects in platelet function: Many intrinsic platelet function defects have been reported in the myeloproliferative neoplasms, although their precise relationships to clinical bleeding are generally unclear.227,228 (3) Elevated platelet counts: The contribution of an elevated platelet count, per se, to the risk of hemorrhage and thrombosis in myeloproliferative neoplasms is controversial, as the risk does not extend to patients with reactive thrombocytosis.229,230 A number of retrospective studies indicate that the risk of abnormal hemostasis cannot be confidently predicted from the degree of thrombocytosis.227 On the other hand, acquired von Willebrand syndrome, which represents a potential major cause of bleeding in the chronic myeloproliferative neoplasms, is most frequently associated with extreme elevations of the platelet count (e.g., ≥1000 to 1500 × 109/L)231–233; in some, the VWF abnormality can be corrected, albeit transiently, by infusion of DDAVP or factor VIII/VWF concentrates, while in others, it can be partially or completely corrected by cytoreductive therapy.234 (4) Leukocytosis may represent a risk factor for thrombosis in the myeloproliferative neoplasms.221,235 In this context, leukocyte and/or endothelial dysfunction may contribute to the thrombotic phenotype in some individuals with polycythemia vera236,237 or essential thrombocythemia232 through leukocyte–platelet and leukocyte–endothelial cell interactions.232,238,239
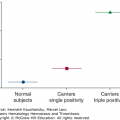
Under the light or electron microscope, platelets in these disorders may be larger or smaller than normal, may be abnormally shaped, and may exhibit a reduction in the number of storage granules.240 In essential thrombocythemia, platelet survival may be modestly reduced.241 A number of functional and biochemical abnormalities have been described in platelets from patients with myeloproliferative neoplasms. The most frequently encountered functional abnormality is a decrease in platelet aggregation and granule secretion in response to epinephrine, ADP, or collagen.227 The defect in epinephrine-induced aggregation often includes absence of the primary wave of aggregation, which is unusual in other conditions. This is not simply the result of an elevated platelet count because it is not encountered in reactive thrombocytosis.222,242 Thus, loss of platelet responsiveness to epinephrine may help to support the presence of a myeloproliferative neoplasm in otherwise ambiguous cases, although the discovery of genetic abnormalities (e.g., JAK2, thrombopoietin receptor [MPL], calreticulin) is beginning to eliminate all ambiguity in the diagnosis of a myeloproliferative neoplasm.
Reduced platelet aggregation and secretion in the myeloproliferative neoplasms is associated with one or more of the following: decreased agonist-induced release of arachidonic acid from membrane phospholipids243,244; reduced conversion of arachidonic acid to PG endoperoxides or lipoxygenase products245; reduced platelet responsiveness to TXA2246; decreased numbers of α2-adrenergic receptors associated with reduced or absent platelet responses to epinephrine247,248; deficiency of integrin α2β1, resulting in variable changes in platelet responsiveness to collagen249; diminished stimulus–response coupling downstream of several agonists associated with reduced activation of phosphatidylinositide 3′-kinase, Rap1, and integrin αIIbβ3250; and deficiency of dense or α granules.251,252 Reduction in platelet procoagulant activity has been reported in some patients with myeloproliferative neoplasms and thrombocytosis,253 as have specific platelet membrane abnormalities, including decreased expression and activation of integrin αIIbβ3,254 decreased amounts of the GPIb–V–IX complex, resulting in an acquired form of Bernard-Soulier syndrome255; decreased numbers of receptors for PGD2256; increased numbers of FcγRIIa receptors257; an increase in GPIV (CD36) with258,259 or without260 a corresponding decrease in GPIb; and impaired expression of MPL in polycythemia vera261 and essential thrombocythemia.111
On the other hand, evidence for in vitro platelet or coagulation hyperactivity has been reported in the myeloproliferative neoplasms. This includes spontaneous platelet aggregation in a patient with essential thrombocythemia and thrombosis,262 increased thromboxane biosynthesis by platelets in patients with essential thrombocythemia263 or polycythemia vera,264 and increased “procoagulant imbalance” in patients manifested by increased endogenous thrombin potential265 and increased procoagulant activity in circulating microparticles.266
Several features of these protean in vitro platelet functional defects require emphasis relative to the clinical setting. First, none are unique to a particular myeloproliferative neoplasm. Second, their relative frequencies have varied widely in reported series. Third, none has been prospectively shown to be predictive of bleeding or thrombosis. Fourth, although the chronic myeloproliferative neoplasms comprise several distinct clinicopathologic entities, they represent clonal abnormalities of hematopoiesis.267 Consequently, megakaryocytes and their platelet progeny may acquire genetic, biochemical, and structural abnormalities as they develop from clones of abnormal progenitors. Examples of clonal defects in the chronic myeloproliferative neoplasms are acquisition of activating mutations in JAK2 (e.g., V617F in polycythemia vera, essential thrombocythemia, and myelofibrosis; or in exon 12 in polycythemia vera)268–272 or MPL (W515L/K in essential thrombocythemia and myelofibrosis).273,274 Mutations in the calreticulin gene have been found in most of the essential thrombocythemia and myelofibrosis patients who lack activating mutations in JAK2 or MPL.275,276 It is biologically plausible that mutations in these or other leukocyte and platelet proteins might influence hemostatic mechanisms, including the activation state of platelets.277–279 However, the precise impact of their presence or allele burden on human platelet function and on thrombotic risk is only now beginning to be understood.232,280 For example, most,232,268 but not all,237,281 studies have concluded that the presence of the JAK2 (V617F) mutation or a high JAK2 (V617F) allele burden confers increased thrombotic risk in essential thrombocythemia, the latter in part a result of higher hemoglobin values. On the other hand, essential thrombocythemia or myelofibrosis patients with calreticulin mutations tend to have higher platelet counts, lower hemoglobin and leukocyte values, and fewer thromboses compared to patients with JAK2 mutations.275,282–285 The same may hold true for rare patients with familial essential thrombocythemia or myelofibrosis and somatically acquired calreticulin mutations.282
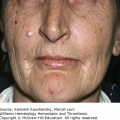
Pathologic bleeding occurs in approximately one-third of patients with myeloproliferative neoplasms and contributes to mortality in 10 percent of those affected patients. Thrombosis also occurs in one-third of patients with myeloproliferative disorders, contributing to mortality in 15 to 40 percent of affected patients.228,232 Most symptomatic patients experience either bleeding or thrombosis; however, some develop both complications during the course of their disease. Bleeding usually involves the skin or mucous membranes but may also occur after surgery or trauma. Thrombosis can involve arteries or veins and may occur in unusual locations such as abdominal wall vessels or the hepatic, portal, and mesenteric circulations.286–291 Indeed, full-blown or latent chronic myeloproliferative neoplasms account for a substantial proportion of patients with splanchnic vein thrombosis.286,291–294 Individuals with essential thrombocythemia may experience ischemia and necrosis of the fingers and toes from digital artery thrombosis, microvascular occlusion in the coronary circulation, or transient neurologic symptoms, including headaches,295 because of cerebrovascular occlusion.296 A syndrome of redness and burning pain in the extremities, termed erythromelalgia, is strongly associated with essential thrombocythemia and polycythemia vera and is thought to be partly caused by arteriolar platelet thrombi, although it may also have vasculopathic and neuropathic components.297,298 It has been difficult to predict the risk of bleeding or thrombosis in an asymptomatic patient,229 but an increase in leukocyte count221,232,235 or the number of reticulated platelets in patients with thrombocytosis, thought to reflect an increase in platelet turnover, has been associated with an increased risk for thrombosis.299 Vascular complications are also more likely to occur in patients older than 60 years of age and, most importantly, in patients with other cardiovascular risk factors, such as diabetes, hypertension, hyperlipidemia, and obesity.221,300–303
Therapy should be risk-adapted and considered for symptomatic patients, for patients with a history of thrombosis or bleeding, for those with standard cardiovascular risk factors, for patients older than 60 years of age, and for individuals about to undergo surgery. Readers are referred to expert recommendations for a summary of the treatment of essential thrombocythemia and polycythemia vera, with particular relevance to risk factors for hemostasis and thrombosis.221,232,301,303–306 Treatment includes phlebotomy to correct the polycythemia and maintenance of a normal red cell mass, with the goal to achieve a hematocrit of less than 45 percent,235,307,308 as well as therapy of the underlying disorder.228,232,309,310 Platelet count reduction to less than 400 × 109/L in patients with thrombocytosis, either by plateletpheresis or cytoreductive agents, has been considered to be a target value associated with clinical improvement in patients with essential thrombocythemia.228,302,311
Effective cytoreductive agents include the ribonuclease reductase inhibitor hydroxyurea,312 interferon-α (most recently the pegylated form of interferon alfa-2a), and anagrelide.301,311,313,314 In a prospective, randomized trial of 114 “high-risk” individuals with essential thrombocythemia who were either older than 60 years of age or had a previous history of thrombosis, hydroxyurea significantly reduced the incidence of new thrombosis from 24.0 to 3.6 percent.312 Anagrelide, an imidazoquinazoline derivative, is thought to decrease platelet counts by impairing megakaryocyte maturation.315 Anagrelide has essentially no effect on red and white cell counts and is not known to be leukemogenic. Nevertheless, 10 to 20 percent of patients experience neurologic, gastrointestinal, and cardiac side effects, in particular fluid retention, often necessitating discontinuation of the drug.314,316,317 When hydroxyurea and anagrelide were compared head-to-head in a randomized trial of 809 patients with essential thrombocythemia (all of whom were taking aspirin), subjects in the anagrelide group showed an increased rate of arterial thrombosis, major bleeding, and transformation to myelofibrosis relative to the group treated with hydroxyurea; however, the anagrelide group showed a relative decreased rate of venous thrombosis.318 Progression to myelofibrosis despite treatment with anagrelide has also been observed in a phase II study.319 However, in a newer, although relatively small, randomized, phase III study of 259 previously untreated high-risk patients with essential thrombocythemia, anagrelide was found to be noninferior to hydroxyurea in the prevention of arterial or venous thrombotic complications.320 It should be noted that this study used a long-lasting anagrelide drug that is not currently available in the United States. During an episode of acute bleeding in the chronic myeloproliferative neoplasms, DDAVP infusion may temporarily improve hemostasis if the patient has an acquired storage pool defect or acquired von Willebrand syndrome.252,321 In the case of acquired von Willebrand syndrome, cytoreduction to reduce the platelet count may also ameliorate the process, although this may take time and require more temporizing interventions including DDAVP or factor VIII/VWF concentrates.234
Low-dose aspirin (~80 to 100 mg/d) may be useful in patients with essential thrombocythemia and thrombosis, particularly those with erythromelalgia or with digital or cerebrovascular ischemia.231,232,298,322 However, the evidence to date remains largely anecdotal, and aspirin can exacerbate a bleeding tendency in patients with myeloproliferative neoplasms, particularly in individuals with acquired von Willebrand syndrome or with World Health Organization (WHO)-defined prefibrotic myelofibrosis masquerading as essential thrombocythemia.221,301,303,323 Consequently, even though a single, daily, low-dose aspirin is recommended for thromboprophylaxis in essential thrombocythemia, a risk-adapted approach is advised.221,305 In addition, because platelet volume and turnover may be enhanced in essential thrombocythemia and polycythemia vera, the platelets of some individuals may not achieve total COX-1 inhibition with a single daily dose of aspirin. In such circumstances, 12-hour dosing may be considered, although this protocol has not been formally evaluated in a prospective clinical trial.324,325
In a double-blind, placebo-controlled study of 518 patients with polycythemia vera who were judged to have no contraindications to daily low-dose (100 mg) aspirin, subjects in the aspirin arm exhibited a reduced risk of nonfatal arterial and venous cardiovascular end points. Although aspirin was well tolerated, there was no effect of aspirin on overall and cardiovascular mortality.326 As has been noted,307 this study population was heavily pretreated to normalize the platelet count, although some individuals may have had residual elevations in red cell mass. Consequently, the safety and efficacy of aspirin as observed in this study may not be relevant to all patients with polycythemia vera.
Pregnant women with essential thrombocythemia or polycythemia vera pose special challenges because of an apparent increased risk of unsuccessful pregnancy, thrombotic or bleeding complications, and potential teratogenicity of hydroxyurea.305,327 In essential thrombocythemia, the risk of first-trimester miscarriages may be higher among women with the JAK2 (V617F) mutation.328 Although evidence-based recommendations are not available, Barbui and Finazzi recommend a risk-adapted approach to management in pregnancy. High-risk women are defined as those with previous major bleeding or thrombotic episodes, previous pregnancy complications, or a platelet count greater than 1500 × 109/L.329 Low-risk individuals are recommended to be maintained at a hematocrit of less than 45 percent and to receive aspirin, 100 mg/d, during pregnancy and low-molecular-weight heparin, 4000 U/d, for 6 weeks after delivery. Interferon-α, rather than aspirin, is considered if there has been previous major bleeding or if platelets are greater than 1500 × 109/L. High-risk patients are recommended to receive low-molecular-weight heparin throughout pregnancy.
The most frequent cause of bleeding in patients with leukemia or a myelodysplastic syndrome is thrombocytopenia. However, abnormal platelet function in vitro has been described in acute myelogenous leukemia, and in some patients, this may be clinically significant. In acute myelogenous leukemia and its variants, platelets may be larger than normal, abnormally shaped, and exhibit a marked variation in the number of granules. There may be decreased aggregation and serotonin release in response to ADP, epinephrine, or collagen, decreased surface P-selectin expression in response to platelet activation via the PAR-1 thrombin receptor, and decreased platelet procoagulant activity. These functional abnormalities may be caused by either acquired storage pool deficiency or a defect in the process of platelet activation through one or more signaling pathways.330–334 These defects are intrinsic to the platelet and probably relate to the fact that the megakaryocytes from which platelets were derived originated from a leukemic stem cell. Indeed, in a familial platelet disorder with a predisposition to acute leukemia, platelet dysfunction prior to the development of leukemia occurs, at least in part, because of downregulation of genes such as NF-E2 or ALOX12, themselves target genes of RUNX1, a transcription factor that is germline-mutated in these individuals.335,336
As discussed in the section on oncology drugs, drugs used to treat acute leukemias may affect platelet function, at least in vitro.200,337,338 Bleeding in the acute leukemias usually responds to platelet transfusions and to treatment of the underlying disease. Similar in vitro platelet abnormalities may be seen in the myelodysplastic syndromes, sometimes accompanied by clinical bleeding disproportionate to that expected for the degree of thrombocytopenia.330,339–344 In these syndromes, platelets may be less uniformly affected, perhaps because there is a residual population of normal platelets admixed with those from the malignant clone.
Reduced platelet aggregation has been reported in children with acute lymphocytic leukemia.331 Unless the leukemia is biphenotypic, it is difficult to ascribe the platelet defect to the leukemic process itself. Platelets are normal in children with acute lymphoblastic leukemia in complete remission.345 Single cases have been reported of patients with acute B-lymphoblastic leukemia346 or Hodgkin lymphoma347 whose severe bleeding was attributed, in part, to acquired Glanzmann thrombasthenia associated with antiintegrin αIIbβ3 antibodies. Hairy cell leukemia is a lymphoproliferative disease in which platelet dysfunction may rarely complicate the clinical picture; bleeding is usually due to thrombocytopenia rather than platelet dysfunction.348 Some patients may exhibit storage pool deficiency or a defect in the process of platelet activation. These abnormalities have been reported to disappear following splenectomy,349 which usually corrects the thrombocytopenia as well. Acquired von Willebrand syndrome has been reported in association with hairy cell leukemia.350
Platelet dysfunction is observed in approximately one-third of patients with immunoglobulin (Ig) A multiple myeloma or Waldenström macroglobulinemia, 15 percent of patients with IgG myeloma, and in occasional patients with monoclonal gammopathy of undetermined significance.351,352 In addition to platelet dysfunction, other causes of bleeding should be considered in these patients, including the hyperviscosity syndrome,353 thrombocytopenia, complications of amyloidosis such as amyloid angiopathy354 or acquired factor X deficiency,355,356 and, rarely, a circulating heparin-like anticoagulant357–359 or systemic fibrino(gen)lysis.360,361 The monoclonal immunoglobulin may also affect in vitro coagulation tests by interfering with fibrin polymerization and with the function of other coagulation proteins. On occasion, paraproteins can impair in vivo hemostasis as well.
The bleeding time may be prolonged in patients with dysproteinemias, even in the absence of clinical bleeding. The platelet defect is caused by the monoclonal protein. It has been suggested that some monoclonal immunoglobulins interact with the platelet surface to interfere nonspecifically with platelet adhesion or stimulus–response coupling. This concept is supported by the observations that platelet dysfunction is more common when the concentration of the paraprotein in plasma or on the platelet membrane is very high362; that platelet aggregation, secretion, clot retraction, and platelet procoagulant activity may all be affected; and that normal platelets can acquire these defects when incubated with the purified monoclonal immunoglobulin.363
In some cases, specific interactions of the monoclonal protein with platelets or with components of the extracellular matrix have been described. One reported IgA myeloma protein inhibited the ability of a suspension of aortic connective tissue to aggregate normal platelets.364 The bleeding time and bleeding diathesis of the patient from whom this myeloma protein was obtained were corrected by removal of the protein by plasmapheresis. In another patient with IgDλ myeloma, λ dimers were found to bind to the A1 domain of VWF, inhibiting shear-induced platelet aggregation.365 In still another patient, an IgG myeloma protein bound specifically to the platelet integrin β3 subunit. Both the intact immunoglobulin and its F(ab’)2 fragment inhibited the binding of fibrinogen to activated integrin αIIbβ3, thus inducing a thrombasthenic-like state.366 A number of patients with myeloma, monoclonal gammopathy of undetermined significance, lymphoma, or chronic lymphocytic leukemia have been reported to have an acquired form of von Willebrand disease in which the level of plasma VWF is reduced or the high-molecular-weight multimers of VWF are selectively reduced.321,352,367–374
When clinically significant platelet dysfunction occurs in a patient with a dysproteinemia, cytoreductive therapy should be considered as a means to reduce the production and plasma level of the monoclonal immunoglobulin.351,352 Plasmapheresis can also control bleeding by reducing the level of the abnormal protein and can be lifesaving during acute bleeds.352,375,376 Cryoprecipitate, DDAVP, and/or plasmapheresis may be transiently effective in patients with acquired von Willebrand syndrome.321,368,377,378 However, high-dose intravenous gamma-globulin (IVIG) appears to be particularly effective in individuals with acquired von Willebrand syndrome associated with an IgG monoclonal gammopathy of undetermined significance, although intermittent infusions may be required at approximately 3-week intervals (Chap. 16).352,369–371,379–381 The reported experience with rituximab for the latter condition is extremely limited, but so far disappointing.382
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree