Acne
Acne vulgaris
Androgens and sebum production: At adrenarche, rising levels of dehydroepiandrosterone sulfate (DHEAS), likely after conversion to testosterone and dihydrotestosterone, cause sebaceous glands to enlarge and produce more sebum. Increased sebum production contributes to obstruction within follicles and correlates with acne severity.
Bacteria and the innate immune response: Propionibacterium acnes is an anaerobic gram-positive rod that colonizes pilosebaceous follicles following increases in sebum production. P. acnes elaborates lipases that can damage the follicle wall and releases a number of chemotactic factors and proinflammatory mediators.
Abnormal keratinization: Epithelial cells lining the follicle proliferate more rapidly and become more cohesive. The result is a collection of cells and sebum that leads to the development of the primary acne lesion, the microcomedo.1 As obstruction increases, the follicle may rupture with spread of its contents into surrounding tissues, an event that contributes to inflammation.
Obstructive lesions (comedones): Obstruction within follicles initially is microscopic (i.e., microcomedones) but ultimately becomes apparent as open and closed comedones. Open comedones (blackheads) have a dilated follicular orifice and a black color (thought to be due to oxidized melanin, altered transmission of light through epithelial cells, or the presence of certain lipids in sebum) (Fig. 21.1). Closed comedones (whiteheads) are small (1 mm in diameter) white to skin-colored papules (Fig. 21.2).
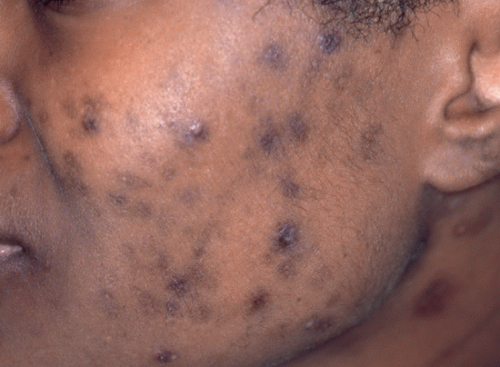
Inflammatory lesions: Rupture of obstructed follicles leads to the formation of erythematous papules (<5 mm in diameter), pustules, and nodules (>5 mm in diameter) (Fig. 21.1). As inflammatory lesions resolve, they often leave erythematous (Fig. 21.1), violaceous, or hyperpigmented (Fig. 21.3) macules that may persist for as long as a year. Patients often mistake these lesions for scars.

FIGURE 21.2 In this patient who has moderate mixed acne (inflammatory and comedonal), there are closed comedones (yellow arrows), papules (green arrow), and pustules (blue arrow).
Scars: Scarring is most likely to occur in those who have large inflammatory lesions (i.e., nodules). On the face, scars appear as small pits (Fig. 21.4), while on the trunk they are hypopigmented macules. Occasionally, patients develop hypertrophic scars (i.e., keloids) or cysts (compressible nodules that lack overlying inflammation).
Pomade acne: Caused by physical obstruction of follicles, most often from inadvertent application of hair styling products (e.g., pomades, greases) to facial skin. Comedones are concentrated on the forehead near the scalp and in the temporal fossae.
Acne conglobata: A severe form of acne in which cysts, abscesses, and draining sinuses develop on the face, chest, or back (e-Fig. 21.1). Extensive scarring and keloid formation are common.
Acne fulminans: This severe acne variant is characterized by the abrupt onset of painful nodules and cysts that become hemorrhagic and ultimately suppurate. Ulcers form and heal slowly, often leaving extensive scarring. Fever, chills, weight loss, myalgias, or arthritis may be present. Patients may have leukocytosis, anemia, elevated inflammatory markers and transaminases, and periosteal reaction suggestive of osteomyelitis.
Gram-negative folliculitis: Infection with gram-negative bacteria that complicates long-term oral antibiotic treatment of acne. The organisms most often responsible include Escherichia coli, Enterobacter spp, Serratia marcescens, and Klebsiella spp. Patients exhibit inflammatory papules and pustules concentrated around the nose.
Mild acne: A minority of the face is involved; a few papules and pustules are present, but there are no nodules or scars.
Moderate acne: Approximately one-half of the face is involved; papules and pustules are more numerous, but nodules are few (Fig. 21.1).
Severe acne: The majority of the face is involved; papules and pustules are numerous, and there are several nodules; scarring may be present (Fig. 21.4).
Keratosis pilaris (KP): Small skin-colored papules located on the cheeks. A keratin plug emanating from the follicular orifice may be seen or palpated (differentiating the lesions from those of acne) (e-Fig. 21.2). KP often also affects the upper outer arms, thighs, and buttocks, areas not involved by acne.
Periorificial dermatitis: Erythematous papules, pustules, and scaling concentrated around the mouth, nose, or eyes. Unlike in acne, lesions are not present on the forehead or cheeks (e-Fig. 21.3).
Rosacea: Erythematous papules, pustules, and scaling involve the central face. Unlike in acne, flushing and telangiectasias are present (e-Fig. 21.4).
Pityrosporum folliculitis: Folliculitis caused by Pityrosporum ovale results in pruritic erythematous papules and pustules on the back, chest, and shoulders. In contrast to acne, the face is spared (e-Fig. 21.5). A potassium hydroxide preparation performed on a pustule roof may reveal spores and short hyphae.
Facial angiofibromas (adenoma sebaceum): Erythematous papules or nodules involving the nasolabial folds, nose, and medial cheeks (e-Fig. 21.6). Lesions typically appear in childhood, earlier than would be anticipated for acne.
TABLE 21.1 Key Elements of the History | ||||||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
|
TABLE 21.2 Options for Managing Mild Acne | |||||
|---|---|---|---|---|---|
|
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree