Increasing data on treatment of liver metastases with locoregional therapies have solidified the expanding role of interventional radiologists (IRs) in the treatment of liver metastases from colorectal cancer. Ablative approaches such as radiofrequency ablation and microwave ablation have shown durable eradication of tumors. Catheter-directed therapies such as transarterial chemoembolization, drug-eluting beads, yttrium-90 radioembolization, and intra-arterial chemotherapy ports represent potential techniques for managing patients with unresectable liver metastases. Understanding the timing and role of these techniques in multidisciplinary care of patients is crucial. Implementation of IRs for consultation enables better integration of these therapies into patients’ overall care.
Treatment of limited metastatic disease can prolong survival; however, in many instances patients may not be ideally suited for surgery, may not be able to discontinue chemotherapy in the perioperative period, or may prefer a less invasive therapy to maintain quality of life. Several image-guided procedures have evolved within the last 10 years that allow the management of limited metastatic disease in nonresectable patients and those that have recurred after resection. These locoregional therapies include local tumor ablation and catheter-directed therapies, and can occasionally downstage a patient with inoperable metastases to an operable status. Ablative therapies cause focal destruction of tissue, and have increasingly been shown to successfully eradicate colorectal liver metastases. Although it has been less used than hepatic ablation, pulmonary thermal ablation has achieved promising results with respect to safety and local tumor control. An increasing number of studies evaluating local ablation for the treatment of pulmonary colorectal metastases is emerging. Definitive integration of ablative therapies into the management of metastatic colorectal cancer depends on defining the patient population in which ablation can be used instead of surgery with equivalent results. In hepatocellular carcinoma, for example, the data have suggested that for tumors smaller than 2 cm ablation may be preferable to surgery. With improving technology, similar equivalencies with ablation in colorectal metastases may arise. Catheter-directed therapies such as transarterial chemoembolization (TACE), drug-eluting beads (DEB), selective internal radiation therapy (SIRT), and intra-arterial chemotherapy ports are all potential techniques for managing the patient with unresectable liver metastases.
IRE is generally indicated for tumors that are deemed inappropriate for thermal ablation because of the relatively high risk of collateral damage caused by tumor proximity to bile ducts or other structures that would be injured by the heat. Clinical series that included patients with CLM have demonstrated a primary efficacy of 67% to 100% for tumors adjacent to major vascular/biliary structures. The risk of recurrence seems to be higher for tumors greater than 3 cm in size. Current evidence, while encouraging, is still limited, with no randomized controlled trials. Most of the series included different organs and differing pathology, making it difficult to draw any generalized conclusions.
Catheter-directed liver therapies
Arterial therapies for colorectal liver cancer metastases can be performed to complement or salvage the effects of systemic therapy. The concept of intra-arterial therapies relies on the fact that liver cancers derive their blood supply predominantly from hepatic arteries, whereas normal liver parenchyma has a predominantly portal vein source of blood supply. The most common techniques of intra-arterial therapies for CLM include intra-arterial hepatic chemotherapy (IAHC), TACE, and SIRT with yttrium-90–impregnated microspheres. Two more therapies are available, namely intraportal drug delivery and isolated liver perfusion.
Intra-arterial Hepatic Chemotherapy
IAHC aims to increase the drug concentration in liver metastases and thereby improve response rates. This approach can be best applied with drugs having a high first-pass effect. One drug that has been extensively used is floxuridine (FUDR), which has a first-pass extraction rate of 95% and can increase the liver dose by 100 to 300 times higher than the systemic perfusion. Historically, repeated or continuous IAHC has been delivered by a catheter and pump system requiring laparotomy. More recently, IAHC has become deliverable via an interventional radiology approach with a subcutaneous port placed. In one study of 36 patients with extensive nonresectable liver metastases (ie, ≥4 metastases in 86% and bilobar in 91%) using IAHC with oxaliplatin (100 mg/m 2 in 2 hours) plus intravenous 5-fluorouracil (5-FU)/leucovorin (LV) (400 mg/m 2 in 2 hours; 5-FU 400 mg/m 2 bolus then 2500 mg/m 2 in 46 hours) and cetuximab (400 mg/m 2 then 250 mg/m 2 /wk or 500 mg/m 2 every 2 weeks) as first-line treatment overall response rate was 90% and disease control rate was 100%. Forty-eight percent of patients were downstaged enough to undergo an R0 resection and/or RFA.
Conventional Transarterial Chemoembolization and Transarterial Chemoembolization with Drug-Eluting Beads
There are several different techniques under the acronym TACE. The most common procedure is the intra-arterial injection of chemotherapy emulsified with Lipiodol Ultra-Fluid (LUF; Laboratoire Guerbet, Aulnay, France) followed by injection of embolic material. With Lipiodol-TACE, the ratio of drug concentration in the tumor compared with the healthy liver and peripheral blood levels can be as high as 10 and 1000 times, respectively. Embolization after chemo-Lipiodol increases the efficacy of treatment by prolonging contact of chemotherapy to the tumor cells and by adding ischemia to the highly hypervascularized tumor usually targeted with this treatment. Such embolization has been reported to induce failure of the transmembrane pump, thus increasing drug retention inside the cells.
One group using the regimen of cisplatin, doxorubicin, mitomycin C, ethiodol, and polyvinyl alcohol has shown an overall response rate of 43%. Median survivals of 33 months from initial diagnosis, 27 months from the time of liver metastases, and 9 months from the start of chemoembolization were documented, suggesting a possible improvement over reported survival time for systemic therapies alone. Another group using mitomycin C alone (52.5%), mitomycin C with gemcitabine (33%), or mitomycin C and irinotecan (14.5%) has shown an overall response rate of 63%.
Recently, drug-eluting beads have been developed that allow drug release after the bead has been embolized into the tumor microcirculation. One of the drugs that has been loaded on these beads is irinotecan. The advantage of the beads is a reduced systemic delivery of chemotherapy. Irinotecan-loaded beads had a 75% reduced systemic plasma level compared with intra-arterial irinotecan alone.
In a randomized study of 2 courses of DEBIRI (Biocompatibles, Oxford, CT, USA) (36 patients) compared with 8 courses of intravenous irinotecan, 5-FU, and leucovorin (FOLFIRI; 38 patients) used to treat 74 patients who failed at least 2 lines of chemotherapy, the DEBIRI arm was met with statistically significant improvement of all oncologic outcomes including patient survival. Specifically, the response rates were 69% for the DEBIRI group compared with 30% for the systemic FOLFIRI group. Similarly, the 2-year OS was 56% compared with 32%, and the median OS was 22 months compared with 15 months for DEBIRI versus FOLFIRI groups. Improvement in quality of life was of longer duration for the DEBIRI group (8 months) than for the FOLFIRI group (3 months, P = .0002). Finally, overall cost was lower for the DEBIRI treatment arm.
In a multicenter, single-arm study of 55 patients who underwent DEBIRI after failing systemic chemotherapy, response rates were 66% at 6 months and 75% at 12 months, with an OS of 19 months and a PFS of 11 months.
A recent comparison study of DEBIRI versus radioembolization for salvage therapy for liver-dominant CLM including a series of 36 patients reported similar survival for both treatments, with median survival times of 7.7 months for the DEBIRI group and 6.9 months for the radioembolization (SIRT) group. The 1-, 2-, and 5-year survival rates were 43%, 10%, and 0% in the DEBIRI group and 34%, 18%, and 0% in the SIRT group.
Approximately 20% of DEBIRI sessions are associated with adverse events (most commonly CTCAE [Common Terminology Criteria for Adverse Events] grades 1 and 2) during or after the treatment. The factors predictive of adverse events and significantly longer stay in hospital are: lack of pretreatment with hepatic arterial lidocaine ( P = .005); greater than 3 treatments ( P = .05); achievement of complete stasis ( P = .04); treatment with greater than 100 mg DEBIRI in 1 session ( P = .03); bilirubin greater than 2.0 μg/dL with greater than 50% liver replaced by tumor ( P = .05).
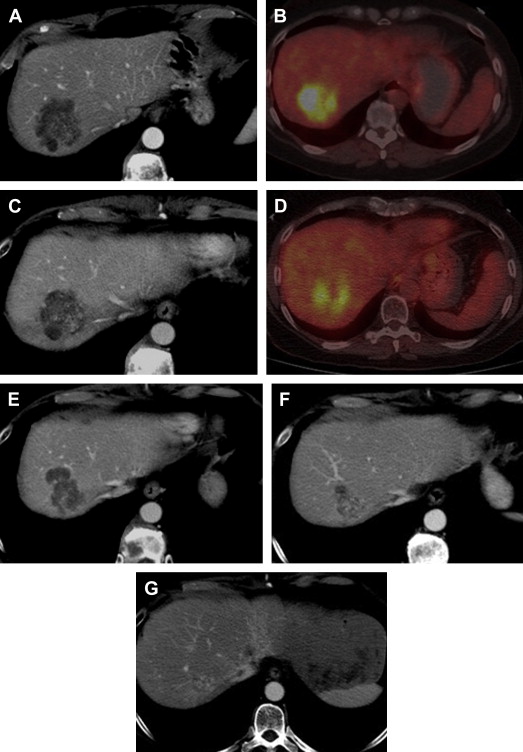
Radioembolization/Selective Internal Radiation Therapy
Traditional external beam radiation therapy in patients with diffuse hepatic malignancy does not improve OS because liver tolerance for developing radiation-induced injury is low compared with the doses required for tumoricidal effect. The usual dose to treat a tumor is 70 Gy, whereas normal liver tissue tolerance to radiation is 30 Gy. These facts resulted in the idea of selective internal transarterial radiotherapy with the delivery of yttrium-90–impregnated microspheres. Selective intra-arterial delivery enables doses higher than 120 Gy to target the tumor without reaching the liver toxicity threshold. Radioembolization allows delivery of high doses of ionizing radiation to the tumor with minimal radiation to surrounding tissue, thus causing considerably less toxicity to the normal liver. Patients referred to radioembolization have unresectable (and noneligible for ablation) CLM, liver-only or liver-dominant disease, life expectancy of at least 3 months, and acceptable liver reserve. SIRT has been safely used as a salvage therapy in heavily pretreated patients who progressed after multiple lines of systemic and hepatic arterial chemotherapy in addition to resection. Overall response of 17% to 35% and stable disease rates of 24% to 61% have been described. Median survival after radioembolization has ranged from 6.7 to 17 months. Modest effects of radioembolization were seen when it was used as a salvage monotherapy after complete failure of chemotherapy. Radioembolization alone in this setting showed an overall response of 24%, a PFS of 3.7 months, and 1- and 2-year overall survival rates of 50.4% and 19.6%, respectively. The major contribution of radioembolization was documented when it was used together with systemic chemotherapy ( Fig. 2 ). The major concept behind this combined treatment was that tumors were sensitized by one treatment for the other and, thus, a synergistic effect of SIRT with chemotherapy was seen, with better response rates. In a randomized controlled trial the combination of SIRT with protracted 5-FU had a significantly better PFS when compared with protracted 5-FU alone in patients who had previously failed regimens containing 5-FU.
Ablative therapy for colorectal lung metastases
Metastasectomy may afford a prolonged survival of up to 60% at 5 years for patients with limited pulmonary metastases from colorectal cancer. However, many patients are poor surgical candidates because of compromised pulmonary function, concurrent medical conditions, or previous lung resections. Patients with limited pulmonary metastases will require multiple repeated resections because not all of the metastatic disease is detectable at first presentation and because there is a high likelihood of tumor recurrences. However, repeat thoracotomy is technically challenging and further removes functional pulmonary tissue. In patients with unresectable isolated colorectal lung metastases, a median survival time of 19 months was observed after chemotherapy.
Ablation of pulmonary colorectal metastases is an appealing technique, as it: (1) has a limited effect on pulmonary function; (2) is repeatable; (3) does not interfere with chemotherapy; and (4) maintains patients’ quality of life. Several series have shown that RFA can be a safe and effective treatment for unresectable CLM. However, special considerations apply to thermal ablation in lung tissue because of the low thermal and electrical conductivity of air surrounding the tumors, resulting in difficulty in ablating the marginal parenchyma. Similarly to liver ablation, the presence of vessels and airways may result in a heat-sink effect, thus increasing the risk of local recurrence. An ablative margin of at least 5 mm around the tumor should always be the end point of pulmonary RFA ( Fig. 3 ). To achieve this, repositioning the electrode multiple times in an overlapping manner is frequently needed, especially for larger tumors.
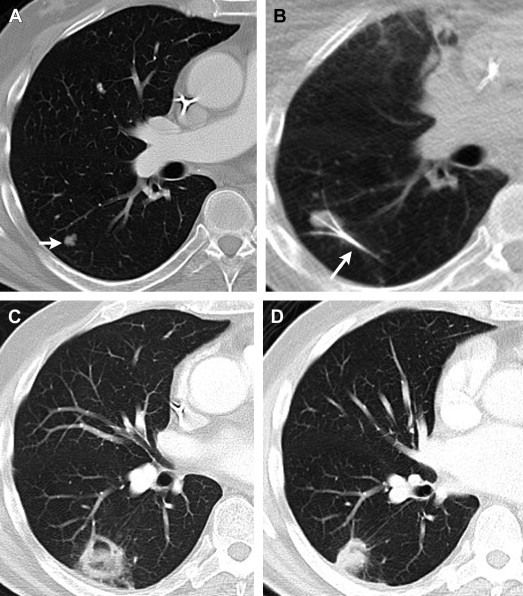
The local tumor progression rate after lung RFA varies in the literature between 9% and 38%. The size of the ablated tumor was shown to be an independent factor for local tumor progression, with significantly lower PFS rates for patients in whom the ablated lung metastasis was greater than 3 cm (61% at 1 year and 34% at 3 years vs 88% and 69%, respectively, for tumor size ≤3 cm ). A carcinoembryonic antigen level of greater than 5 ng/mL was also associated with decreased local tumor PFS. Median OS of CLM after RFA has been consistently reported to be between 31 and 46 months, with 1-, 2-, and 3-year survival rates of 84% to 95%, 54% to 72%, and 35% to 57%, respectively. A lung colorectal metastasis greater than 3 cm was independently associated with decreased OS after RFA. Patients who undergo ablation of more than 1 growing pulmonary nodule in the setting of other stable lung metastases seem to have a significantly lower OS rate at 3 years after RFA compared with patients treated with RFA to cure 1 (or more) lesion that represents the only pulmonary disease at that time (27% vs 78%, P = .05).
Because RFA often has technical challenges resulting from poor electrical conduction in the lung, both cryoablation and MWA are being explored. To date there is only one report of cryoablation for the treatment of pulmonary colorectal metastases. This study included 24 patients with 55 metastatic lung tumors, and reported a median OS of 43 months and a 3-year survival rate of 60%. These findings are very similar to those of RFA. Recently, the safety and efficacy of lung MWA have been prospectively evaluated in nonsurgical candidates with pulmonary metastases. The study included 80 patients with various lung metastases, half of which were of colorectal cancer origin. One- and 2-year survival rates were 91.3% and 75%, respectively, with no significant difference by histopathologic type. Higher survival rates were observed in patients who were tumor-free after ablation than in patients who progressed. Local tumor control rate at 18 months was 73% for the entire group and 76% in the colorectal pulmonary metastases group.
As patients with metastatic colorectal cancer are living longer, the possibility of incorporating chemotherapy breaks into their care without negatively affecting survival has to be considered. Pulmonary ablation of a solitary nodule in the setting of no extrapulmonary disease can afford patients a “chemotherapy holiday” while under rigorous imaging surveillance. Such chemotherapy breaks of up to 20 months were reported to be possible without disease progression.
Summary
Interventional radiologists are playing an increasing role in the management of patients with metastatic colorectal cancer. Implementation of the interventional radiology clinic for consultation has expanded the role of the interventional radiologist as a consultant and as an important contributor to the multidisciplinary management and customization of the treatment of these patients.
In the interventional radiologist’s armamentarium are ablative tools that can focally destroy small numbers of liver metastases. Many of the techniques offer minimally invasive treatments that maintain quality of life, do not interfere with chemotherapy regimens, and are repeatable as needed.
In view of the established impact of surgical morbidity on survival and the improved safety profile of ablation, selected patients with lesions that could be ablated with sufficient margins may benefit from the least invasive and equally effective ablative therapy. The use of ablation in a test-of-time paradigm may limit unnecessary and morbid resections, significantly contributing to the preservation of patients’ quality of life.
Locoregional arterially directed therapies for liver-dominant metastases allow the interventional radiology physician to manage the unresectable patient with the aim of extending disease-free periods and OS and, hopefully, converting him or her to a resection candidate for a potential cure. In particular, IAHC and SIRT have reported a fraction of treated patients being downstaged to resection. Both IAHC and SIRT have also been associated with best oncologic outcomes when combined with earlier lines of systemic chemotherapy.
As all of these tools and techniques have become available and have been perfected over the past decade, it will become important for them to be investigated in clinical trials to best determine their appropriate use in the care of the colorectal patient with liver or lung metastases. The selection of the best therapy for each patient requires multidisciplinary discussion, and the role of interventional radiology in this collaboration has reached the point that they may be considered the fourth pillar in oncology, along with medical, surgical, and radiation oncology.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree