Scout/localizer
Pre-contrasta
Inject
1st post contrasta
2nd post contrasta
3rd post contrasta
4th post contrasta
Axial post delayed
Non fat sat T1
T2
DWI
Full diagnostic MRI
x
x
x
x
x
x
x
x
x
x
x
Kuhl et al. abbreviated
x
x (axial, non-fat sat)
x
x (axial, non-fat sat)
Mango et al. abbreviated
x
x (sag)
x
x (sag)
Grimm et al. abbreviated 1
x
x (axial)
x
x (axial)
x
Grimm et al. abbreviated 2
x
x (axial)
x
x (axial)
x
x
Trimboli et al.
x
x
x
x
Heacock et al. abbreviated 1
x
x (sag)
x
x (sag)
Heacock et al. abbreviated 2b
x
x (sag)
x
x (sag)
Heacock et al. abbreviated 3
x
x (sag)
x
x (sag)
x(sag)
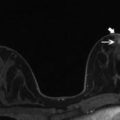
Fig. 16.1
Forty-six-year-old female with a palpable right 3:00, 1.4 cm moderately differentiated invasive ductal carcinoma (white solid arrow). Selected sequences provide an example of the abbreviated breast MRI protocol investigated by Kuhl et al. [28]. (a) Axial pre-contrast non-fat saturated T1-weighted image (b) Axial first post-contrast fat saturated T1-weighted image (c) Axial first post-contrast subtracted T1-weighted image and (d) Axial MIP image. Note the MIP shows bilateral asymmetric enhancement. The MRI demonstrates suspicious non mass enhancement in the contralateral breast (white dash arrow). (e) Axial pre-contrast non-fat saturated T1-weighted image (f) Axial first post-contrast fat saturated T1-weighted image (g) Axial first post-contrast subtracted T1-weighted image. MR biopsy of the left breast yielded fibrocystic change and marked adenosis deemed concordant with imaging findings
Table 16.2
Comparison of sensitivity, specificity, negative predictive value (NPV) and positive predictive value (PPV) of published abbreviated protocols compared to the full diagnostic MR protocol
Sensitivitya | Specificity | PPV | NPV | |
|---|---|---|---|---|
MIP (Kuhl et al.) | 90.9 | NA | NA | 99.8 |
1st post (Kuhl et al.) | 100 | 94.3 | 24.4 | 100 |
Full MR (Kuhl et al.) | 100 | 93.9 | 23.4 | 100 |
MIP (Mango et al.) | 93 | NA | NA | NA |
1st post (Mango et al.) | 96 | NA | NA | NA |
1st post sub (Mango et al.) | 96 | NA | NA | NA |
Abbreviated 1 (Grimm et al.) | 86 | 52 | NA | NA |
Abbreviated 2 (Grimm et al.) | 89 | 45 | NA | NA |
Full MR (Grimm et al.) | 95 | 52 | NA | NA |
Abbreviated (Trimboli et al.) | 78 | 87 | 74 | 90 |
abbreviated 1 (Heacock et al.) | 97.8 | NA | NA | NA |
abbreviated 2 (Heacock et al.) | 99.4 | NA | NA | NA |
abbreviated 3 (Heacock et al.) | 99.4 | NA | NA | NA |
Achieving such high sensitivity and specificity with limited MR sequences would be ideal in the screening setting. The Kuhl study also demonstrated expected decreased radiologist reading time of the abbreviated protocol, on average 2.8 s for the single MIP image and 28 s for the complete abbreviated protocol which is faster than published screening mammogram reading times of 60–120 s [29, 30] (Table 16.3). Such short reading times could allow for batch reading of MR screening exams similar to the model currently used for mammography. The reported full diagnostic protocol acquisition time was 17 min but only 3 min for the abbreviated protocol. Comparing this time to other breast cancer supplemental screening options is striking given the average ultrasound screening time of 19 min reported in the American College of Radiology Imaging Network breast ultrasound screening trial by Berg et al. [2, 31]. In this trial a doubled cancer yield (14.9 %) was achieved by adding MRI following ultrasound, showing the superiority of MRI over ultrasound for breast cancer detection.
Table 16.3
Comparison of time to acquire and read the full diagnostic breast MRI to the abbreviated protocol
Full protocol scan time | Full protocol radiologist interpretation time | Abbreviated scan time | Abbreviated protocol radiologist interpretation time | |
|---|---|---|---|---|
Kuhl et al. | 17 min | NA | 3 min | 28 s |
Mango et al. | 30–40 min | NA | 10–15 mina | 44 s |
Grimm et al. (abbreviated 1) | 30–45 min | 2.95 min | 2.98 min | |
Heacock et al. (abbreviated 1) | 35 min | 15 min | 7 min | 14–25.4 s |
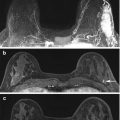
Findings in the Kuhl study are further supported in a study by Mango, et al. which examined an abbreviated protocol consisting of a pre-contrast fat saturated sagittal T1 image and single early post-contrast sagittal T1 image [32]. In this study four experienced breast radiologists reviewed 100 cases of biopsy proven unicentric breast carcinoma including the first post-contrast T1, post processed subtracted first post-contrast and subtraction MIP images. As all the patients had cancer, this study addressed cancer visualization but did not simulate a true screening environment. Nonetheless results for cancer localization and detection were promising as all 100 cancers (21 DCIS and 79 invasive cancers; mean cancer size 2.2 cm) were visualized on initial reading of the abbreviated protocol by at least one reader and 92/100 by all four readers (Fig. 16.2). This resulted in a mean sensitivity of 96 % for the first post-contrast sequence, 96 % for the first post-contrast subtraction and 93 % for the subtraction MIP sequence, the MIP sequence was statistically significantly inferior. These sequences were interpreted together as one examination and there was no significant difference between sensitivities for the different readers. Both the Kuhl and Mango studies suggest the subtraction MIP sequence alone is not sufficient for detection of all cancers. Kuhl et al. also noted that MIP images did not provide enough information for the reader to provide a BI-RADS assessment if a lesion was present and thus readers in that study simply determined the presence or absence of significant enhancement (i.e. above background parenchymal enhancement) when reading the MIP alone. However, they found just the first post-contrast image was sufficient to provide a BI-RADS assessment.
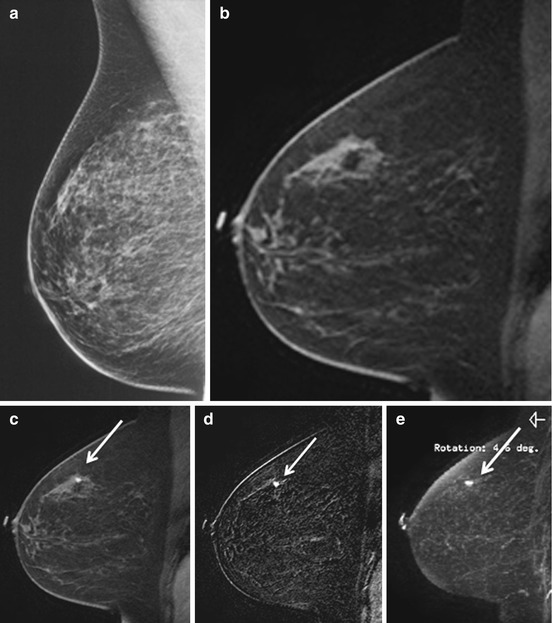
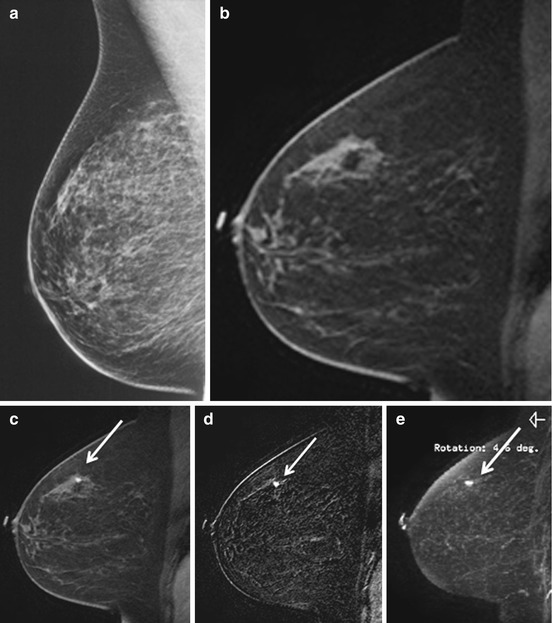
Fig. 16.2
Fifty-four-year-old woman with right 12:00, 0.7 cm invasive ductal carcinoma (white arrow). (a) Mammogram, MLO image. Cancer mammographically occult. Selected MR sequences provide an example of the abbreviated breast MRI protocol investigated by Mango et al. [32]. (b) Sagittal precontrast fat saturated T1-weighted image, cancer not visualized (c) Sagittal early postcontrast fat saturated T1-weighted image (d) Sagittal postcontrast T1-weighted subtraction image (e) Sagittal subtraction MIP
Similar to the Kuhl study, Mango et al. demonstrated decreased image acquisition and radiologist reading times. They estimated the abbreviated imaging protocol to take 10–15 min of magnet time including image acquisition, patient transitions/instructions and contrast injection compared with 30–40 min for the full protocol. Interpretation of the abbreviated protocol averaged 44 s compared with published mean time to read standard breast MRI of 4.7 min [33].
A more recent study by Heacock et al. supports these results and examines utilization of the T2-weighted sequence and history/prior imaging in an abbreviated MR protocol [34]. Their abridged protocol consisted of T1-weighted images (non-contrast, first post-contrast and first post-contrast subtraction sequences) read with and without history/prior imaging available (abbreviated protocols 1 and 2). An additional reading was performed with T2-weighted images also available (abbreviated protocol 3). Total MR acquisition time was 12 min including a reported 5 min for the T2-weighted sequence. Looking at 107 patients with known unifocal breast carcinoma they found all cancers were identified on the T1-weighted sequences by at least one reader with a mean cancer detection rate of 97.8–99.4 %. T2-weighted imaging increased lesion conspicuity but did not improve cancer detection. Given study design the effect of T2-weighted images on specificity could not be evaluated. Mean interpretation times for 3 readers for T1-weighted sequences was 14.0–25.4 s with T2-sequences adding an average of 5.0–9.9 s to the interpretation time. Improved cancer detection rates were seen for all readers with prior imaging and clinical history available.
Studies of such abbreviated protocols highlight limitations when depending on just a few sequences for interpretation. For example, a protocol consisting of a single MIP image may be insufficient for interpretation due to extensive background parenchymal enhancement (BPE) or subtraction errors secondary to patient motion. Kuhl et al. noted 3.6 % of their cases required reading of the complete abbreviated protocol due to these limitations on the MIP [28] (Fig. 16.1). Additionally, lack of the T2 sequence eliminates assessment for lesion T2 hyperintensity which may enable the benign assessment of a finding. Absence of a T1 non-fat saturated image may limit diagnosis of fat necrosis or identification of an intramammary node fatty hilum and result in patients being recalled for the full diagnostic exam [32]. In addition, only obtaining one post-contrast sequence prohibits kinetic analysis of a lesion.
Before abbreviated breast MRI is utilized as a mass population screening tool one must also consider the indirect costs of the abbreviated protocol through BI-RADS 3 follow up or biopsy recommendations. In Kuhl’s study the full diagnostic protocol and complete abbreviated protocol performed similarly for cancer detection and had similar false-positive diagnoses; however, the full protocol enabled downgrading of 37.7 % of lesions (20 of 53) to BI-RADS 2 initially characterized as BI-RADS 3 on the complete abbreviated protocol [28]. This supports the impression that the full protocol sequences assist more in lesion characterization than lesion detection. In patients with BI-RADS 3 lesions on the abbreviated MR exam a decision must be made to perform a full diagnostic exam for further lesion characterization versus 2 year abridged MR imaging follow up to assess for stability. A cost benefit analysis is necessary to see if the expense and time of the full diagnostic protocol would be worthwhile in this setting. Interestingly Kuhl et al. also demonstrated that reading the full diagnostic protocol upgraded lesion assessment to BI-RADS 4 in 4 of 53 women, leading to biopsy of a papilloma but no additional cancers. Thus the additional sequences of the full diagnostic protocol did not always improve patient outcomes and may result in additional procedures in a few cases.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree