A study of relationship between leptospirosis and cerebral arteritis and moyamoya disease
Outline
There have been sporadically reported cases of cerebral vasculitis of unknown causes in the rural areas of Hubei province since 1958. The cases increased remarkably from 1973. After studying the clinical characteristics, radiology, pathologic anatomy and epidemiology of the disease, we discovered it is cerebral arteritis, mainly caused by genus leptospira. We also studied so-called moyamoya disease, which named by scientists in Japan, and concluded that moyamoya disease is a clinical syndrome which might be caused by leptospiral cerebral arteritis rather than an independent disorder. We reviewed and summarized the national and international findings on this topic.
Since 1958, a disease, with the main physical signs of hemiplegy, bilateral hemiplegia and aphasia but in their right senses, was sporadically epidemic among the children, adolescent and young people in the rural areas of Hubei province; there are special changes in patients’ cerebral angiography. Its clinical presentation meets with the characteristics of cerebral vascular disease, thus it was then considered as a cerebral vasculitis of unknown causes, and some named it “obstructive cerebral vascular disease”, while some hospitals diagnosed it sporadic encephalitis or other diseases. Hubei received relatively high rainfall in 1973; outbreaks of acute leptospirosis were reported in some areas. In the same area, there was a remarkable increase of cerebral vasculitis cases, but most of the cases did not have apparent history of leptospirosis. It was urgent to make clear whether these so-called cerebral vasculitis cases were related to the leptospirosis, and it has theoretical and pragmatic implications to prevent this disease.
Scientists from the Wuhan Medical College (WHMC) systematically researched the disease from clinical, radiological, pathologic anatomical and epidemiologic aspects and found that it was a disorder of cerebral arteritis and mainly caused by the infections of genus leptospira.
Moyamoya disease, with unknown causes, is a diagnosis based on cerebral angiography. WHMC’s studies indicated that it is not an independent disease but a multifactoral clinical syndrome. Moyamoya disease occurred in the rural areas of Hubei was an infection mainly caused by genus leptospira.
We reviewed and summarized below the pathogenesis findings from national researches.
1. The relationship between cerebral arteritis and the leptospirosis infection
1.1 Clinical presentation of cerebral arteritis
The patients of cerebral arteritis have paralysis of central nervous system and the symptoms and physical signs of other nervous system, present with the clinical characteristics of obstructive cerebral vascular disorders and can clinically exclude known diseases that might cause the damages in cerebral vascular vessels such as arthrosclerosis, tuberculosis and arthritis. This disease was also called as obstructive cerebral vascular disorder or cerebral arteritis.
Normally these cases have no history of acute leptospirosis, but approximately 27% cases have history of acute febrile symptoms several months before the disease onset, while they do not have typical symptoms of leptospirosis. As we know now that these patients have ever had mild or asymptomatic infection of leptospirosis, this has been proved by the evidences from serological epidemiology.
The department of neurology in the second affiliated hospital of WHMC reported the results from the analysis on 616 leptospral cerebral arteritis (1). There are a wide range of clinical characteristics for this disorder. Most of patients usually are healthy before the onset of the disease and suddenly occurred the symptoms of hemiplegia, aphasia etc. A small proportion of patients have precursory symptoms of short-term febrile, headache, paroxysmal extremity numbness, weakness. Hemiplegia is predominant among all types of the paralysis, and followed by bilateral hemiplegia; all the others are paralysis of central nervous system. A considerable number of patients have motor aphasia. In the damage of brain nerves, some patients have central nervous paralysis in the 7th pair of unilateral brain nerves, or in the 7th and 12th pairs of unilateral brain nerves. It also could have central nervous paralysis in the 9th and 10th pairs of bilateral brain nerves.
Most patients are in their right senses, a small part of cases have consciousness disorder to various degrees. Regarding psychiatric symptoms, patients could also present intelligence decrease in varying degree.
Peripheral blood smear: both numerical counts of white and red blood cells have no particular change. The results of cerebral spinal fluid test are normally normal.
Most cases could recover if early treatment sought but patients normally develop some sequels. Some cases have recurrence and a minority dies from organ failure or secondary infections and so on.
Hou Zongchang et al. observed 36 latestage encephalopathy of leptospirosis(2). The clinical presentation of its encephalopathy is almost the same with aforementioned cerebral arteritis.
1.2 The changes of cerebral vascular angiography in patients with cerebral arteritis
Liu Ximin et al.(3) from the department of neurology of WHMC reported the results from the analysis of cerebral angiography for 100 cerebral arteritis. The common characteristics of cerebral arteritis are: patients’ pathological changes of cerebral
arteries are in a relatively extensive range, among which the most severe pathological changes have been observed in the terminal portions (C1-2) of internal carotid arteries, the proximal portions (A1-2, M1-2) of the anterior and middle cerebral arteries, and showed uneven inner diameters or complete occlusion at some portions of blood vessels. The surface of inner walls are rough and silkworm-bit looking. An outstanding characteristics is unusual enriched accessory circulations, these can be seen among the terminal portions of anterior, middle and posterior arteries. There are collateral circulations with varied extents between external carotid artery and radicular artery. Most patients have the blood vessel network consisted of a large amount of thin and tiny blood vessels in the base of the brain. Authors think the changes in the cerebral angiograph are completely consistent with pathological data; the number, severity and recovery possibility of physical signs of neurological system are closely associated with whether the collateral circulation is well-established and whether there are occlusions at trunk arteries at the time of disease onset.
arteries are in a relatively extensive range, among which the most severe pathological changes have been observed in the terminal portions (C1-2) of internal carotid arteries, the proximal portions (A1-2, M1-2) of the anterior and middle cerebral arteries, and showed uneven inner diameters or complete occlusion at some portions of blood vessels. The surface of inner walls are rough and silkworm-bit looking. An outstanding characteristics is unusual enriched accessory circulations, these can be seen among the terminal portions of anterior, middle and posterior arteries. There are collateral circulations with varied extents between external carotid artery and radicular artery. Most patients have the blood vessel network consisted of a large amount of thin and tiny blood vessels in the base of the brain. Authors think the changes in the cerebral angiograph are completely consistent with pathological data; the number, severity and recovery possibility of physical signs of neurological system are closely associated with whether the collateral circulation is well-established and whether there are occlusions at trunk arteries at the time of disease onset.
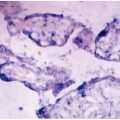
1.3 The study of the pathological anatomy of arteritis
There are three post-mortem examinations [1] have been done by the department of pathological anatomy at the WHMC since 1968. Basically they had similar pathological changes, multiple arteritis at the base of the brain and its induced damages in the brain parenchyma are the main pathological changes. There is no apparent pathological change in the vein system of the brain. The pathological changes in the arteries are distributed sectionally thus made the arteries’ diameters uneven, the pathological changes can be as long as 5 to 6 centimeters. The same arteries in both sides have similar extent of pathological changes, but the distribution is not totally symmetrical. The main change of affected arteries is apparent hyperplasia at the endothelium, thus causes the stenosis or even occlusion of the blood vessels. The pathological changes are generally mild at the tunica intima and tunica media. The tendency of forming thrombosis is not high.
Pathological changes of the brain: in the early stage of the course, it is likely to be the arteritis in blood vessels. But along with the progress of course, the main presentation is the hyperplasic inflammation in the arteritis. This kind of change does not affect the small blood vessels in the brain parenchyma.
This kind of pathological changes could not be observed in the other blood vessels, except for the bronchial pneumonia, there is no remarkable change in the other organs.
Leptospirosis (silver-plating method) has been detected at the tunica adventitia of arteries in the pathological brain parenchyma in one case. This patient had ever been tested in the laboratory for leptospirosis, the serum complement fixation test of leprospirosis were positive for two times, titer was 1:40 and 1:80 respectively; titer of serum microscopic agglutination test: 1:1600 for Pomona, 1:400 for autumnalis; 1:16 for the spinal fluid complement fixation test of leptospirosis, 1:20 for Pomona microscopic agglutination test.
The changes in the pathology can exclude the brain damages caused by arthritis, syphilis, tuberculosis, meningitis, arthrosclerosis, periarteritis nodosa.
1.4 The analysis of epidemiologic etiology of cerebral arteritis
1.4.1 The distribution of cerebral arteritis cases
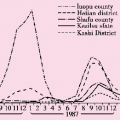
The distribution of cerebral arteritis is closely related to leptospirosis or the infection.
1.4.1.1 Regional distribution: in the past, there was very few case report of cerebral arteritis. In nationwide, there is increased number of reports from different provinces or regions due to the development of research work, the epidemics of this disease had been seen in Hebei, Hubei, Jiangsu, Shandong, Henan, Guangdong, and Guangxi[4,5,6,7,8 and 9]. Most cases are in the countryside, and more likely in the verified affected areas of leptospirosis. It normally occurred sporadically, but also often clustered in certain regions, the incidence in some villages can be as high as 1.3%, or accounts for 6.45% of all leptospirosis cases[2,4].
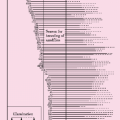
1.4.1.2 Temporal distribution: cerebral arteritis could occur at any time of the year, but most likely between October and December, it is often 2 to 5 months after the peak of leptospirosis epidemics. As seen from Table 4.1, the cases between October and December accounts for half of the cases in the whole year.
Table 4.1 Seasonal distribution of cerebral arteritis cases in Hubei | ||||||||||||||||||||||||||||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
|
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree