Fig. 15.1
Changes in serum non-stimulated thyroglobulin levels in the patient, a 70-year-old Japanese woman. RAIT radioactive iodine treatment
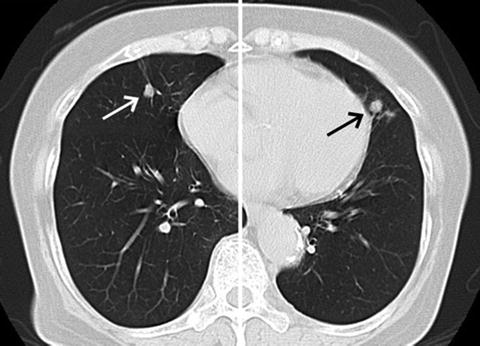
Fig. 15.2
November 2007 chest CT scan showing pulmonary metastases
In November 2012, an ultrasound examination detected suspicious lymph nodes measuring 11 mm and 9 mm in her right level II. However, fine-needle aspiration biopsy was not performed, since performing a reoperation for such small nodal metastases would be unlikely to improve her prognosis because of the presence of multiple lung metastases. Lung metastases had enlarged to 16.6 × 11.4 mm and 14.3 × 7.0 mm on the left and right sides, respectively, in December 2013 (Fig. 15.3), although the size of the suspicious nodes was unchanged.
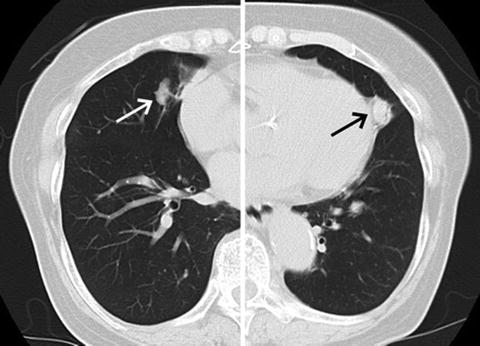
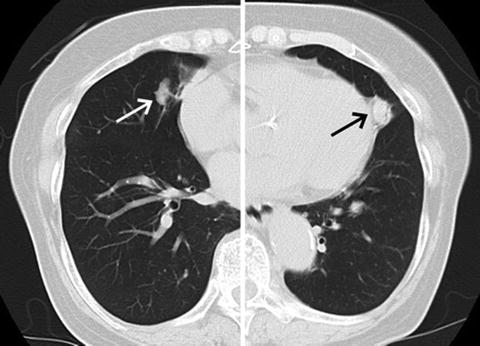
Fig. 15.3
December 2013 chest CT scan showing that the pulmonary metastases had slightly increased in size
As of June 2014, the patient was 83 years old with no symptoms of metastases, and her serum Tg level was 58.8 ng/mL (Fig. 15.1). Although she had been on prolonged TSH suppressive therapy, her bone density did not change between September 2005 and December 2012. Her TSH was suppressed to around 0.01 mIU/L.
The changes in the patient’s serum non-stimulated Tg levels showed a gradual and exponential increase over time (Fig. 15.1). When we used a log scale for the vertical axis of the graph of the patient’s Tg values, the change was basically linear and the slope of the regression line did not change between before and after the therapy (Fig. 15.4). We calculated the Tg-doubling time (DT) from the slope of the regression line, as we reported for the calcitonin DT in patients with medullary thyroid carcinoma [2]. A regression line, log y = log a + bx, was computed by nonlinear least square regression (x, years after surgery; y, Tg level), and thyroglobulin-doubling time (Tg-DT) was given as (log2)/b. The calculated Tg-DT was 2.7 years. We also calculated tumor volume DTs from the sizes of the pulmonary metastatic lesions on CT images in November 2007 and December 2013. The values were 2.6 and 2.8 years for the left and right metastatic lesions, respectively. These values were very similar to the Tg-DT.
Fig. 15.4
Semilogarithmic graph showing the linear change in the patient’s serum non-stimulated thyroglobulin levels. The vertical axis is shown in log scale for serum thyroglobulin levels. The straight line represents the regression line. The thyroglobulin-doubling time was calculated from the slope of the regression line. RAIT radioactive iodine treatment
Assessment and Literature Review
Therapies for Metastatic PTC
Papillary thyroid carcinoma (PTC) metastasizes not only to lymph nodes but also to distant sites such as the lung and bone, for which RAI therapy is the first-line treatment. However, no therapy was available for the patient’s RAI-refractory metastases except for TSH suppression. Some molecular-targeted agents were recently reported to be effective for differentiated thyroid carcinomas (DTCs), including PTCs, with RAI-refractory metastases [3, 4]. However, in clinical practice, it remains unclear whether and when molecular-targeted agents should be administered, since not all RAI-refractory cancers are rapidly progressive and life threatening.
Representative Molecular-Target Agents for RAI-Refractory PTC
It was reported that sorafenib and lenvatinib significantly prolonged the progression-free survival (PFS) of DTC patients in randomized phase III studies [3, 4]. However, these agents displayed a high frequency of various adverse events, e.g., hand-foot syndrome (76 %), diarrhea (69 %), alopecia (67 %), rash (50 %), and hypertension (41 %), for sorafenib [3] and hypertension (68 %), diarrhea (60 %), fatigue/asthenia (59 %), decreased appetite (50 %), and nausea/vomiting (46 %) for lenvatinib [4]. The median PFS and hazard ratio (HR) with 95 % confidence intervals (CI) of the DECISION (sorafenib) and SELECT (lenvatinib) trials were 10.8 months (vs. 5.8 months for placebo), 0.59 (0.45–0.76) and 18.3 months (vs. 3.6 months for placebo), 0.21 (0.14–0.31), respectively [3, 4]. These agents are very costly, and since these trials were crossover studies, it was not proved that they prolong overall survival of patients. Clinicians must therefore carefully weigh the advantages and disadvantages of using these agents for individual patients.
Prognosis of DTC Patients with RAI-Refractory Metastases
Not all RAI-refractory metastases are progressive or immediately life threatening. In our prior series, the 5- and 10-year carcinoma-related death rates of 74 DTC patients with RAI-refractory metastases (metastases without RAI uptake from the time of the initial treatment) were 5 % and 30 %, respectively [5]. Therefore, these data suggest that not all patients with RAI-refractory thyroid cancer require treatment with molecular-targeted agents. Without appropriate selection, many of these patients would likely suffer various adverse events without clear improvement in quality of life or survival.
We also demonstrated by a multivariate analysis that older age (≥60 years) was an independent prognostic factor for cause-specific survival (CSS) [6], indicating that RAI-refractory metastases are more progressive in elderly patients. Therefore, molecular-targeted agents are more likely to be administered to elderly patients. We have to be careful in this clinical context, because elderly patients more often have comorbidities such as hypertension, liver and renal dysfunctions, and diabetes mellitus, and they have lower immune resistance than younger patients.
Thyroglobulin-Doubling Time
The change in serum Tg levels is the most important prognostic factor for thyroglobulin antibody (TgAb)-negative patients who have undergone a total thyroidectomy for PTC. We reported that a short Tg-DT (<1 year) after total thyroidectomy strongly predicted a poor disease-free survival (DFS) and CSS (Table 15.1) and that the Tg-DT shorter than 1 year was a very strong predictor of disease recurrence and carcinoma-related death: HR with 95 % CIs for locoregional recurrence, distant recurrence, and carcinoma-related death were 2.38 (1.20–4.71), 4.20 (1.73–10.21), and 47.06 (5.47–405.13), respectively (superior to other conventional prognostic factors in a multivariate analysis) [7]. We also found that the incidence of persistent disease was significantly higher in young (<40 years) and old (≥60 years) patients than in middle-aged patients (40–59 years), whereas short Tg-DT was more frequently observed in old patients than others [8].
Table 15.1




Relationship between cause-specific survival (CSS), distant (DRS) and locoregional recurrence-free survival rate (RFS), and Tg-DT/(first four data)a,b
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree





