Fig. 39.1
Microscopic high power of the medullary thyroid cancer. Tumor is composed of solid nests of variable size, separated by the presence of areas with collagen connective tracts and foci of amyloid deposits from calcitonin. The cells are usually round and fusiform, with poorly defined and finely granular eosinophilic cytoplasm, uniform nuclei, and punctate chromatin
Table 39.1
Classification and treatment of the drug-related diarrhea according to common terminology criteria for adverse events (CTCAE) v4.0
Diarrhea | Treatment | |
|---|---|---|
Grade 1 | Increased of <4 stools per day over baseline, mild increase in ostomy output compared with baseline | No change in treatment Medical intervention not indicated |
Grade 2 | Increased of 4–6 stools per day over baseline, moderate increase in ostomy output compared with baseline | No change in treatment Initiating supportive care |
Grade 3 | Increased of ≥7 stools per day over baseline, incontinence, hospitalization indicated, severe increase in ostomy output compared with baseline. Limiting self-care ADL | Discontinue treatment until recover to grade ≤2 Hospitalization is required for intensive supportive care |
Grade 4 | Life-threatening consequence | Discontinue treatment until recovery to grade ≤2 and reintroduce with dose reduction Hospitalization is required for urgent treatment |
Grade 5 | Death |
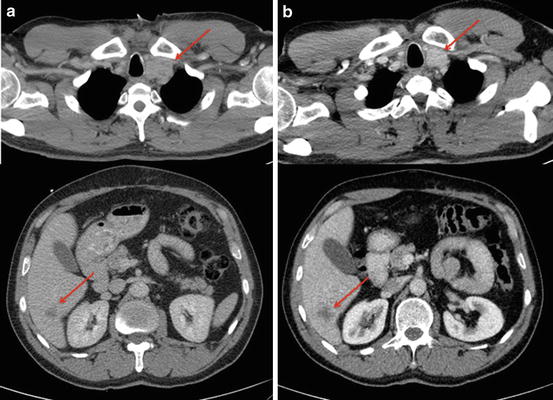
Fig. 39.2
Radiographic assessment conducted in February 2012 (a) and September 2012 (b) during treatment with vandetanib. Stable disease was achieved on the left supraclavicular lymph node (arrow) and the right liver lobe lesion (segment VI) according to RECIST criteria v1.1
Literature Review
The appearance of diarrhea has been described in approximately 30 % of patients with MTC and has been suggested to precede the identification of the thyroid mass in some cases [3]. Calcitonin plays a key role in this disturbance and it seems to be related to an alteration in water and electrolyte movement from absorption to secretion in the intestinal tract [4]. However, intestinal motor dysfunction has been suggested as the main mechanism for diarrhea related to hypercalcitoninemia [5]. Adequate symptomatic control will improve the quality of life of these patients.
Definition
MTC derives from the thyroid parafollicular C cells that are able to produce and secrete calcitonin. This thyroid cancer subtype occurs as a sporadic tumor or as part of a hereditary syndrome (multiple endocrine neoplasia (MEN), 2A and 2B, or familial MTC). Sporadic MTC accounts for 75 % of all cases (Table 39.2). Median age at diagnosis occurs during fifth or sixth decade of life and remains slightly more frequent in women [6]. In 35–50 % of patients, lymph node metastases are observed at diagnosis. When MTC metastasizes, the most common distant sites are the liver, lung, bones, and, with less frequency, brain and skin [7].
Their neural crest origin is responsible for the ability of C cells to take up amine precursors as well as the secretion of neuroactive peptides that include calcitonin, CEA, serotonin, ACTH, chromogranin A, somatostatin, neurotensin, pro-opiomelanocortin, prostaglandins, kinins, histaminase, and vasoactive intestinal peptide (VIP) [8]. Serum calcitonin or CEA elevations are almost universal and are key in MTC diagnosis, monitoring the clinical course of disease, and evaluating the response to therapy.
Symptoms Related to MTC
Typically, patients present with a palpable asymptomatic neck mass. However, with the appearance of a thyroid nodule, clinicians should be aware of the presence of an MTC if patients suffer from symptoms such as diarrhea, flushes, weight loss, and, more rarely, Cushing’s syndrome or if it is associated with a familial history of MTC, pheochromocytoma, and hyperparathyroidism. The systemic symptoms may occur due to hormonal excess or to distant metastatic disease.
In case of a large palpable thyroid nodule, local compressive symptoms, such as dysphagia or a choking sensation, may occur. Rarely, the mass can infiltrate the recurrent nerve and cause hoarseness [9].
Diarrhea in MTC
When faced with a patient with chronic diarrhea, neuroendocrine tumors should always be considered in the differential diagnosis. Clues should be sought in the clinical history, physical examination, complementary studies, and laboratory tests. They can help rule out more common causes of chronic diarrhea such as infections, drug use, chronic inflammatory diseases, cathartic agent use, and diabetic diarrhea.
Diarrhea in MTC is caused by two main pathophysiological mechanisms: the most important one suggests a motor dysfunction diarrhea leading to decreased transit time due to hyperactivity of small intestinal and colonic tone, leading to insufficient absorption. It has been reported in 28–39 % of cases [10]. The second possible mechanism is a secretory impairment as the origin of the diarrhea caused by substances other than calcitonin. This postulated mechanism is based on an increase in fluid and electrolyte secretion induced by prostaglandins (E2 or F2α), serotonin, or substance P that worsens the absorptive dysfunction in the intestinal tract caused by increased colonic tone and decreased transit time [11]. Circulating agents enter the intestinal epithelial cells (located in the jejunum and ileum) and reverse the absorption of water and electrolytes into a secretory process. The rapid emptying of the proximal colon may contribute to the increase stool weight in these patients. While sodium plays a key role in the absorption of water and electrolytes, chloride is the most important electrolyte involved in the secretion of ions. Several intracellular pathways result in the output of chloride ions from the intestinal epithelial cells via a specific chloride channel in the luminal membrane. The process can start on the luminal side, as occurs in infections, or on the serosal side, for example, when related to circulating agents such as serotonin or VIP. Thus, elevated circulating concentrations of hormones such as gastrin, somatostatin, and VIP can alter both gastrointestinal motor function and intestinal secretion and contribute to the diarrhea associated with MTC [12].
This phenomenon usually occurs in advanced disease, so patients can suffer from a syndrome similar to the carcinoid syndrome with flushing and/or diarrhea. Because the increased levels of circulating calcitonin or other peptides stimulate secretion by the small intestine mucosa, the diarrhea can be severe with a large volume of watery stools, often exceeding 1 L per day, without any specific treatment [11].
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree





