(1)
MedStar Washington Hospital Center, 110 Irvig St., NW, Washington, DC, 20010, USA
(2)
Georgetown University School of Medicine, Washington, DC, USA
Keywords
Thyroid cancerHürthle cell thyroid cancerFollicular thyroid cancerRASLymph nodesThyroidectomyRadioiodineRecombinant human thyrotropinTSHFDG-PETCase
A 67-year-old man was referred to our endocrine clinic by his primary care physician for the management of a 5.6 cm thyroid nodule in the left lobe with a recent fine-needle aspiration (FNA) cytology interpreted as an indeterminate diagnosis favoring a follicular neoplasm (Bethesda class IV). A repeat FNA was sent for mutational analysis and was positive for the RAS oncogene, and the patient was referred for thyroidectomy . Preoperative ultrasonography confirmed the left lobe nodule which was hypoechoic with irregular margins and lacked any calcification, and there was suspicion for involved lateral neck lymph nodes. Fine-needle aspiration of the suspicious lymph node confirmed thyroid cancer, and he underwent a total thyroidectomy and central and modified left neck dissection. The surgical pathology described a 6 cm poorly encapsulated tumor with both local invasiveness with extrathyroidal extension and vascular invasion at 8 identified sites. The predominant cell type was oncocytic or oxyphilic with microfollicle formation consistent with a Hürthle cell follicular carcinoma. Extrathyroidal extension was evident with several implants of tumor ranging from 2 to 11 mm in the lateral neck; 6/12 lymph nodes from Level VI and 12/31 lymph nodes from left Levels II and III were positive for metastatic tumor [Stage 4A (T3, N1B, MX)] (Fig. 24.1).
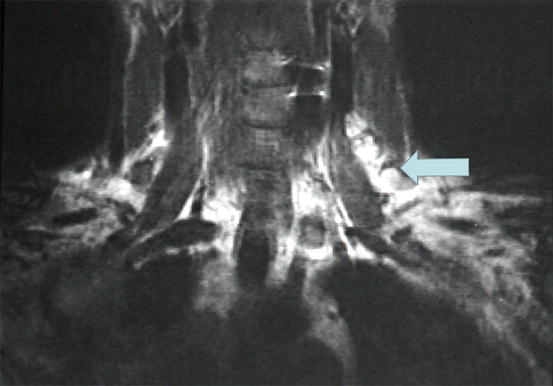
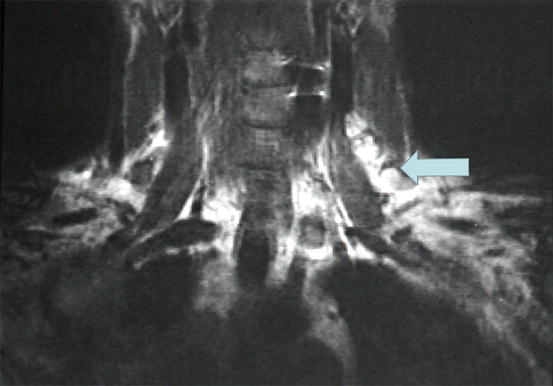
Fig. 24.1
Magnetic resonance imaging (MRI) of patient’s neck demonstrating lymph node metastases in left neck (arrow)
Hürthle Cell Carcinoma: Literature Review
Some thyroid tumors with predominant oncocytic cytology may be benign or so-called Hürthle cell adenomas [1]. Based upon postoperative surgical pathology, the risk of carcinoma in a nodule with FNA cytology read as Hürthle cell neoplasm ranges from 10 to 45 % in various series [2]. The likelihood that such a nodule is a carcinoma increases with nodule size [3] with approximately 50 % of tumors >4 cm and 100 % of tumors >6 cm being malignant [4]. In addition to tumor size, other factors associated with malignancy are male sex, age >65, and highly elevated serum levels of thyroglobulin (Tg ) [5], but cancer is still common but less frequent when Tg levels are <500 ng/mL [6].
In this patient, the finding of a RAS mutation on the fine-needle-aspirated material constituted an additional motivation for proceeding to total thyroidectomy [7]. Although a reading of follicular lesion of uncertain significance (FLUS) carries a low risk of malignancy of 5–20 %, in this patient the interpretation as follicular neoplasm (FN; Bethesda Class IV) carries a somewhat higher risk of 20–30 %, and the large size of the nodule implies an even higher risk [8]. In one study, 87/513 (17 %) of indeterminate nodules on FNA had a positive mutation, and 70 % of these were RAS point mutations as in our patient [9]. In contrast to our patient who had a Hürthle cell carcinoma, most RAS-positive thyroid cancers are papillary thyroid cancers and tend to have a good prognosis [10].
Sonography cannot reliably predict which nodules may be carcinoma as these lesions may present a wide variety of sonographic findings [11], but typically will lack calcification. Current guidelines of the American Thyroid Association [12] do not recommend screening thyroid nodules with FDG-PET scans, but thyroid nodules found incidentally to be positive on PET scan warrant FNA cytology to rule out malignancy. Because there is a correlation between PET positivity and clinical aggressiveness of tumors, Hürthle cell carcinoma is likely to be positive on FDG-PET [13] and was recently also found to be positive on an 18-F DOPA PET scan [14].
Hürthle cells are often present in Hashimoto’s thyroiditis , and the presence of a Hürthle cell lesion in a thyroid gland involved with Hashimoto’s thyroiditis can present a difficult challenge [15]. The Hürthle cell variant of follicular thyroid cancer was first described in 1928 on the basis of the distinctive cellular features of oxyphilic cells with abundant cytoplasm that lack any of the typical cytologic features of papillary thyroid carcinoma such as nuclear pseudoinclusions. Like classic follicular thyroid carcinoma, Hürthle cell cancers may be classified as either minimally invasive with less than four foci of capsular invasion or widely invasive [16]. In general, follicular thyroid cancer is more likely to metastasize to distant sites like lung and bone via vascular invasion and hematogenous spread and typically does not spread to local or regional lymph nodes as is typical of papillary thyroid cancer. Thus, it is less common for the Hürthle cell variant of follicular carcinoma to spread to lymph nodes as it did in this case, and the presence of involved lymph nodes is an independent predictor of reduced disease-free survival [17]. Bishop et al. [18] noted that locoregional soft tissue metastases may be more characteristic of this tumor than lymph node metastases. Whether the prognosis of fully encapsulated minimally invasive small Hürthle cell cancers may be excellent is controversial, with one recent study indicating significant risk of residual or recurrent disease [19]. However, the more invasive types such as the solid or trabecular subtypes are more aggressive, and their course is often marked by both locoregional and distant metastases [20–22]. Identification and classification of the degree of invasiveness is critical to the determination of how aggressively therapy is to be implemented. Unfortunately, a large proportion of Hürthle cell cancers do not trap radioiodine, and even those that may demonstrate 131-I uptake tend to be less radiosensitive than are papillary thyroid cancers. Nevertheless, in contrast to the general consensus and based on an analysis of clinical outcomes in 485 patients with follicular thyroid cancer and 73 patients with Hürthle cell cancer, Sugino et al. [23] concluded that the Hürthle cell patients fared no worse in regard to prognosis.
Management of the Patient
Postoperatively, the patient was started on levothyroxine 0.15 mg/day and placed on a low iodine diet in preparation for diagnostic radioiodine scanning and potential ablation . At 4 weeks postsurgery when his serum TSH level was 0.38, his serum Tg measured 1224 ng/mL, and after preparation with recombinant human thyrotropin (rhTSH ; Thyrogen®), an iodine-123 scan indicated moderate uptake in the right thyroid bed and faint uptake in 3 foci in the left lateral neck and one focus in the anterior mediastinum. The scan results prompted repeat ultrasonography of the neck which indicated either nodules or suspicious lymph nodes in the left neck. Magnetic resonance imaging (MRI) [24, 25] confirmed the lesions which appeared to correlate with the foci of radioiodine uptake on the isotopic scan, and the patient was referred back to his surgeon. A repeat left lateral neck compartmental node dissection was performed with removal of 18 additional lymph nodes, 9 of which were positive for metastatic tumor. At 3 months after his original surgery, his serum Tg was 88 ng/mL with a TSH of 0.03. He was again placed on a low iodine diet and after 2 weeks was treated with an activity of 175 mCi radioiodine facilitated by rhTSH preparation. His posttreatment total body scan revealed only modest uptake of iodine-131, and it is anticipated that he may need to be treated with external radiotherapy [26] or local interventional ablation [27, 28] should persistent locoregional disease be documented.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree





