Fig. 19.1
In the presented case, the patient had a solitary, thinly encapsulated 3 cm nodule in her thyroid lobe (a, gross photograph). On low power, there is a vague, linear disruption within the tumor (asterisks) along with some cellularity within the tumor capsule (oval) (b, hematoxylin and eosin, ×40). Within the capsule, there were irregular nests of tumor embedded in fibrous stroma (c, hematoxylin and eosin, ×400). Within the linear area of tumor disruption, there is evidence of trauma including stromal fibrosis, hemorrhage, and hemosiderin (d, hematoxylin and eosin, ×400). In all, the findings are consistent with a benign follicular adenoma with worrisome histologic alterations following fine-needle aspiration of the thyroid gland
Assessment and Literature Review
This case highlights the important differences between the diagnoses of follicular adenoma and follicular carcinoma and the diagnostic difficulties that can arise in making the distinction.
General Considerations
A follicular adenoma is defined as an encapsulated neoplasm of thyroid follicular epithelial differentiation that lacks evidence of invasive growth and does not exhibit the nuclear features of papillary carcinoma [1]. Its malignant counterpart, follicular carcinoma, is actually a diagnosis of exclusion, defined as “a malignant epithelial tumor showing evidence of follicular cell differentiation and not belonging to any other distinctive types of thyroid malignancy” [2]. Follicular carcinoma is subdivided into two general categories: widely invasive tumors that usually lack a capsule and exhibit extensive, clear-cut invasion of surrounding stroma and minimally invasive tumors that invade only into a surrounding capsule. Widely invasive follicular carcinoma is not easily confused with follicular adenoma; as a result, the remainder of this chapter will deal with the differential diagnosis between follicular adenoma and minimally invasive follicular carcinoma.
Clinical Presentation
Both follicular adenomas and minimally invasive follicular carcinomas tend to present similarly as a solitary thyroid nodule, though follicular carcinomas tend to be larger overall. Patients with large tumors may complain of compressive symptoms like dyspnea, coughing, or hoarseness. Almost all patients with these tumors are euthyroid. Because the defining feature of minimally invasive follicular carcinoma is an architectural one (details below), a definitive diagnosis cannot be made by fine-needle aspiration. Both follicular adenoma and follicular carcinoma are likely to be diagnosed as “suspicious for a follicular neoplasm” or “atypical cells of undetermined significance” by fine-needle aspiration [3].
Treatment
Surgical intervention—at minimum, a thyroid lobectomy—is required to make the diagnosis of follicular adenoma or minimally invasive follicular carcinoma. A patient receiving the diagnosis of follicular adenoma requires no additional therapy. In contrast, the treatment of minimally invasive follicular carcinoma is somewhat controversial. Many experts advocate for completion thyroidectomy with subsequent radioactive iodine, although others have argued that a lobectomy alone may be sufficient, particularly in tumors that exhibit only capsular invasion [4]. Because follicular carcinoma only rarely metastasizes to lymph nodes, a prophylactic lymph node dissection is not recommended [4].
Surgical Pathology
Grossly, follicular adenomas and minimally invasive follicular carcinomas have an appearance that is essentially identical: a solitary, well-circumscribed nodule with a well-developed capsule (Fig. 19.2a). At the microscopic level, follicular carcinomas generally tend to be larger; exhibit more hypercellular growth with microfollicular, trabecular, and solid growth patterns; and possess thicker tumor capsules when compared to follicular adenomas. However, the sole histologic feature that distinguishes follicular adenoma from minimally invasive follicular carcinoma is the presence of invasive growth. Specifically, a follicular carcinoma must exhibit capsular and/or vascular invasion. While this may sound relatively straightforward on its face, any practicing pathologist knows that determining the presence of invasive growth in a follicular neoplasm can be very challenging and is fraught with pitfalls.
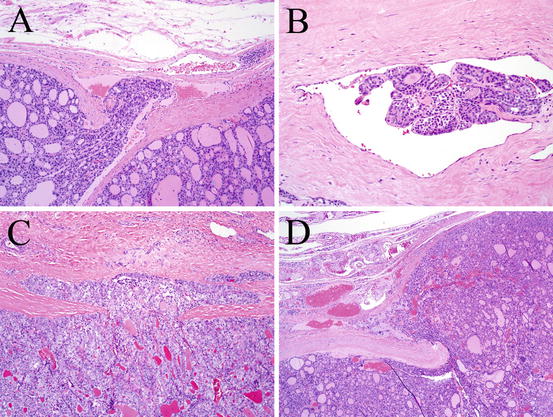
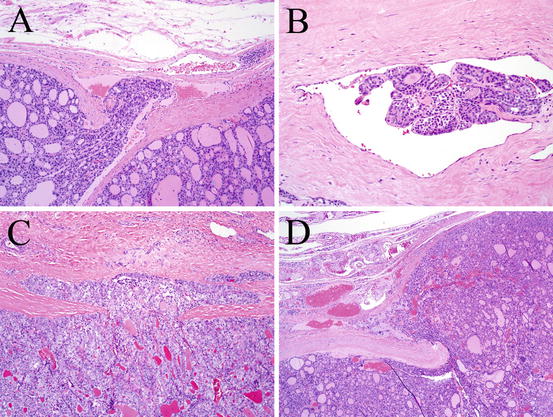
Fig. 19.2
To be regarded as true vascular invasion in an encapsulated follicular carcinoma, the vessel in question must be located within or immediately beyond the tumor capsule (a, hematoxylin and eosin, ×40). In addition, the tumor thrombus must extend into the vessel and is usually covered by a layer of endothelial cells (b, hematoxylin and eosin, ×200). Foci of capsular invasion in a minimally invasive follicular carcinoma often take the shape of a mushroom cloud (c, hematoxylin and eosin, ×100) or a fishhook (d, hematoxylin and eosin, ×20)
Vascular invasion is generally regarded as more reliable than capsular invasion for the diagnosis of minimally invasive follicular carcinoma, and the criteria are strict [2]. To qualify as vascular invasion, the vessel in question needs to be either within the capsule or immediately outside of it; vessels inside the tumor itself should not be considered (Fig. 19.2a). The vessel wall must have a clear-cut endothelial lining and a muscle wall. In addition, the focus of tumor must be attached to the vessel wall with protrusion into the lumen (Fig. 19.2b). Tumor that is “free-floating” within a vessel may represent artifactual detachment from surgery or from the grossing station and therefore does not qualify. Similarly, tumor simply “bulging” into a vessel should not be regarded as truly invasive growth. Ideally, the tumor thrombus should be lined by an endothelial layer, though not all authorities agree on the importance of this finding [2, 5]. In addition, some investigators regard the presence of fibrin thrombi as helpful evidence of true vascular invasion [5].
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree





