This article discusses the growth and infrastructure of a clinical trials program in a large community hospital. An association between increased patient accrual and establishment of site-specific tumor boards and patient care navigators is also discussed. Strong hospital administrative support and clinical research staff are crucial for success.
This article (1) reviews the experience of a clinical trials program at a large community hospital; (2) presents the growth of our trials program along with the increasing number of site-specific tumor boards; and (3) also examines the role of clinical care coordinators, often referred to as patient care navigators. By coordinating and directing patients along a path of optimal multidisciplinary evaluation including presentation at appropriate tumor boards, the authors believe there has been increased participation in clinical trials. They also believe these 2 modalities go hand-in-hand in providing an infrastructure needed to maintain and grow an active community hospital clinical trials program.
Development of clinical trials programs
Clinical trials hold the key to treatment decisions in medicine by bringing basic science research and clinical advances to the mainstream of clinical practice. They have provided a means of translating what we learn in the laboratory into the clinic and build an ever-expanding knowledge base and experience. The role of clinical trials is particularly unique in oncology clinical research. The authors often explain to the residents that to know and understand the early advances in breast cancer treatment, one could study the progression and outcomes of the National Surgical Adjuvant Breast Project clinical trials starting from the 1970s. These trials were somewhat unique in that they included both drug protocols and surgical procedures. The application of these trials, along with others such as from the Milan National Cancer Institute (NCI) by Dr Veronesi has been critical in advancing cancer treatment. In more recent years, the American College of Surgeons Oncology Group (ACOSOG) has also become active in bringing more surgery-related studies to the participating community surgeon as well.
Up to 30 years ago, 80% of clinical trials were done in the academic setting in spite of 80% to 85% of cancer patients being under the care of community oncologists. In 1983, the NCI started the Community Clinical Oncology Program (CCOP) in which community and private physician participation was encouraged. By 1994, Fleming reported that the number of clinical trials done in the community had increased to 60%, with 40% in academic or dedicated cancer centers. In that same year, Cobau reported almost one-third of all patients on clinical trials were accrued via the CCOP program. Though there were initial quality concerns, there proved to be no difference in patient evaluability, eligibility, morbidity, or mortality These concerns were also examined more recently by Wilke and colleagues when looking at National Quality Forum performance measures for breast cancer treatment in the ACOSOG Z0010 breast trial. Data were reviewed from teaching affiliated, academic, and community hospitals. This multiinstitutional trial found excellent compliance with the quality standards regardless of practice environment. This finding was also supported by Lamont and colleagues. They reviewed outcomes from phase III Cancer and Leukemia Group B (CALGB) lung cancer trials at 272 different treatment sites, including academic centers, community hospitals, and Veteran Hospital Administration affiliates. There was no difference in patient survival that could be related to the enrollment setting. They also found that patients enrolled in the community setting provided an important heterogeneity, thus making such studies more relevant to general practice.
Clinical trial participation has been encouraged by many organizations including the American Society of Clinical Oncology (ASCO), the Society of Surgical Oncology, and the National Comprehensive Cancer Network. When following National Comprehensive Cancer Network (NCCN) guidelines, a statement is made for each tumor site: “the NCCN believes the best management of any cancer patient is in a clinical trial. Participation in clinical trials is especially encouraged.” An editorial by Burstein when discussing the comprehensive nature of the NCCN guidelines states that “this thoroughness creates somewhat of an illusion, however, that NCCN guidelines panel members always know the right thing to do next, that little uncertainty exists, or that things couldn’t be done better. This is rarely the case in oncology, of course, which is why clinical trials are needed.”
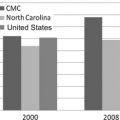
Participation in clinical trials is considered a measure of a cancer program’s success. Clinical trial accrual is an important eligibility criterion for participation and accreditation with the American College of Surgeons Commission on Cancer. A Comprehensive Community Hospital Cancer Program designation requires 2% of annual newly diagnosed cancer patients to be accrued. This percentage of cancer patients increases to 4% for a Teaching Hospital Program and 6% for Network Cancer Program designation.
In spite of all of the encouragement and organization support, barriers remain to clinical trial enrollment. These include lack of interest by oncologists and patients, limited access to trials, excessive bureaucratic demands, inadequate financial support, and the difficulty to take the time to do the hard work that is necessary. Though direct revenue is generally considered inadequate, indirect revenue may increase by reducing patient outmigration from the hospital and physician practice, increasing referrals from community physicians and clinics and spin-off laboratory and imaging revenues.
Funding
An ASCO survey by Baer and colleagues indicated a trend toward decreasing participation in NCI-supported clinical trials and an increase in industry-sponsored trials. One of the factors cited was that the NCI reimbursed less than 50% of actual costs incurred, a problem that continues in our current program. Booth and colleagues reported a significant increase in for-profit or mixed sponsorship clinical trials. They reviewed 321 randomized clinical trials covering breast, colorectal, and non–small cell lung cancer published from 1975 to 2004. There was a significant increase from 4% to 57% of for-profit or mixed sponsorship studies over that time. During that same period, government funded randomized clinical trials decreased from 60% (28 of 47) to 31% (51 of 167).
More recent randomized clinical trials also seem to be larger and include more trial centers. Peppercorn and colleagues examined breast cancer trials published in 1993, 1998, and 2003. The authors found the pharmaceutical trials to be more directed to advanced stage or likely to report a single-arm nonrandomized design. These pharmaceutical trials were also not likely to do as many head-to-head drug studies and more likely to report positive results.
Reimbursement from industry-sponsored trials is significantly better than that from cooperative groups. This allows physician and hospital trial programs to perhaps be at least budget neutral. But this is an area of potential conflict of interest, however, and has many implications in the conduct and success of clinical trials and research in general. It has been addressed in a series of articles published in the New England Journal of Medicine from 2000 through 2009. The impact of academic and industry relationship on clinical trials is an interesting issue that will not be further addressed in this article. In spite of these changes and pressures, the percentage of clinical trials at Florida Hospital Cancer Institute (FHCI) sponsored by industry has remained approximately 33% since 1995. The clinical trials available to us are constantly reviewed, and we are currently pursuing development and participation in the Community Clinical Oncology Program. To do so certainly requires a strong commitment by the medical staff and significant administrative support, given the reimbursement issues in today’s financial climate.
Florida Hospital Cancer Institute
The Florida Hospital in Orlando was founded in 1908 and has grown into a 1000-bed facility today. The most significant growth has been within the last 10 to 15 years when there has been increase in bed capacity and expansion of multiple programs. Six other hospitals have been incorporated into a system covering 3 counties. The original facility functions as the main or tertiary center for the system.
The FHCI was initiated in 1985, and the oncology clinical research program was started in 1989. From 1989 to 1991, there was only one nurse covering 11 medical oncologists and support staff varied between 1 and 2 people. Since then the number of staff has increased dramatically. This has been a function of sheer patient volume and clinical trial requirements for data collection for the life of the patient. Increasing patient survival has thus resulted in increasing staffing needs. There are now 16 nurses, 3 regulatory staff, 3 data managers, 1 office manager, and more than 28 physicians involved in the clinical trials program. This research team works with the participating physicians and provides staff and family education, implements protocols, organizes the consenting process, helps monitor test results, and collects and organizes data.
The original and continued structure of the program is as a hospital-based program with a centralized staff performing eligibility evaluation, trial oversight, and data management. All trial reimbursement comes to the central clinical trials office and helps to offset the costs of the clinical trials nurses and support staff. None of the reimbursement goes to the participating physicians. As previously noted, the actual costs of the trials can be substantially greater than the sponsor reimbursement, particularly from the NCI. This strongly suggests how critical it is to have FHCI administrative support, understanding the importance of the trials program in spite of its financial costs.
As this program began, we became affiliated with the Duke Oncology Consortium through which we could participate in cooperative trials. Over the years we have continued to expand our affiliations to include the Sarah Cannon Group in Nashville, the Texas Offender Reentry Initiative (TORI) program from University of California, LA, and the International Bone Marrow Transplant Registry.
Having a broad base of clinical trials available allows potential inclusion of many more patients. As the volume of patients has increased so has the number of nurses required to do these initial consults and evaluations. We now have 16 nurses who are responsible for these evaluations that take place at multiple sites in our system.
Though the number of trials offered per year has remained relatively stable, the number of consults per year has grown dramatically. This increase is also reflected in the number of patients enrolled on clinical trials per year. Table 1 shows the number of trials available, consults, and clinical trial enrollment over intervals of 5 years from 1993 through 1997 and 1998 through 2002. Table 1 also reflects the most recent data collected over a 7-year period from 2003 through 2009. The number of consults and subsequent patients enrolled had a dramatic increase as of approximately 1998, and this increase has been maintained.