Case 39
Presentation
A 59-year-old man presents with a 4-month history of intermittent bright red bleeding per rectum treated as hemorrhoidal disease. For the last 2 months, he complained of pain with defecation, incontinence, and weight loss.
He was diagnosed 10 years ago with human immunodeficiency virus (HIV) and hepatitis C and had hemorrhoid banding 5 years ago. He has no allergies. Current medications include stavudine (Zerit), lamivudine (Epivir), nelfinavir (Viracept), and an antidepressant. He is homeless and is enrolled in a detox program for alcohol, cocaine, and tobacco (40-pack-year) addiction. There is no known family history of cancer.
He is alert with normal vital signs, is thin but not cachetic, and sits with some discomfort. He has moist mucous membranes with no icterus, pallor, or generalized lymphadenopathy. He has a palpable liver 3 cm below the costal margin.
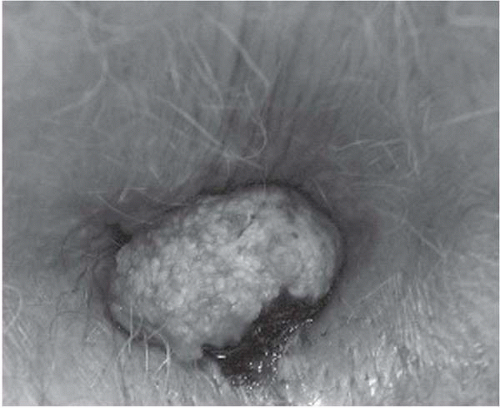
▪ Clinical Photograph
Physical Examination Report
Rectal examination shows a 2-cm exophytic mass at the right lateral anal margin with a 5 × 3-cm firm, tender, lobulated, and fixed intra-anal mass. The surrounding skin is erythematous due to pruritus. No enlarged inguinal lymph nodes are palpated.
Differential Diagnosis
Given the appearance and intra-anal component, a neoplastic growth would be on top of the list, most commonly epidermoid carcinoma, anal adenocarcinoma, or amelanotic melanoma. The external component could be mistaken for thrombosed fibrotic hemorrhoids, or hypertrophied and prolapsing anal papilla.
Discussion
The anal canal is defined as extending from the anorectal ring to the intersphincteric groove corresponding to the length of the internal sphincter. The anal verge is the junction of the keratinized hair-bearing squamous epithelium and the anoderm. The mucosa of the anal canal varies from rectal columnar to the anal transitional zone (extending variably above the dentate line, usually 5 to 10 mm) to squamous nonkeratinized anoderm without hair or other skin appendages. The anal transitional zone has the most varied epithelium including basal, columnar, cuboidal, and squamous cells in four to nine layers. In addition, this zone may have endocrine cells and melanocytes. It is this layer that is most susceptible to human papilloma virus (HPV) infection and is where most anal canal cancers arise.
Anal canal squamous cell carcinoma is defined as a tumor between the intersphincteric groove and the anorectal ring. It accounts for about 1.5% of all
gastrointestinal tract tumors; however, it has been rising in incidence over the past 25 years, especially in HIV-positive male homosexuals.
gastrointestinal tract tumors; however, it has been rising in incidence over the past 25 years, especially in HIV-positive male homosexuals.
Current major known etiological factors are HPV infection and smoking. Smoking increases the risk (relative risk 7 to 9) of anal cancer, and patients with anal cancer have a higher risk of cervical, vulvar, and other smoking-related cancers (i.e., oral cavity, larynx, lung, bladder, and breast cancers). HPV is important in the etiology of anal cancer. There is a strong association among genital warts known to be caused by HPV, low-grade and high-grade squamous intraepithelial lesions and anal cancer, and sexual promiscuity and anal-receptive intercourse. Patients with HIV disease, especially those with CD4 counts less than 200/mm3, have a higher incidence of HPV infection that is more likely to be persistent compared with patients who do not have HIV disease. HIV infection may also predispose to a greater progression of low-grade to high-grade dysplasia. The incidence of anal cancer has increased in both men and women, but especially in HIV-positive male homosexuals. The relative risk in patients with acquired immunodeficiency syndrome (AIDS) may be as high as 84 for homosexual patients compared with 37 for nonhomosexual patients. Transplant patients have been shown to have a tenfold to 100-fold increased risk of HPV infection, anal intraepithelial neoplasia (AIN 1-3), and anogenital cancer. Benign anal disease (e.g., fistulas) is more often a complication of the neoplasm rather than the cause, though very rarely a long-standing fistula in ano can develop adenocarcinoma.
Recommendation
Perform examination under anesthesia, and obtain biopsy to establish tissue diagnosis.
Case Continued
Routine laboratory results show a hemoglobin level of 11.7 g/dL, down from 15 g/dL 6 months ago. Serum chemistry, liver function tests, and chest roentgenogram are normal. His CD4 count is 764 and HIV viral load is less than 50 copies/mL.
The patient undergoes examination under anesthesia, proctoscopy, transrectal ultrasound, and biopsy of the mass.
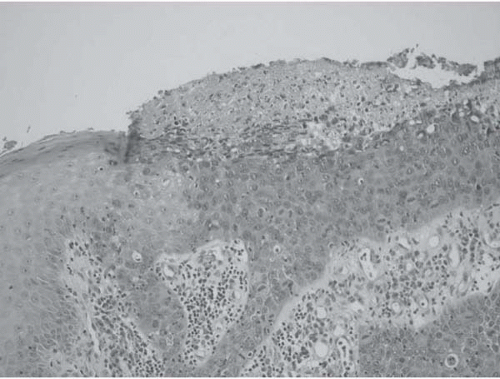
▪ Histopathology Slide
Histopathology Report
Photomicrograph showing junction of normal skin and invasive squamous cell carcinoma. The pathologic diagnosis is moderately differentiated squamous cell carcinoma, clinical stage T2 N0 M0. Higher power reveals HPV cytopathologic changes with crumpled crenated nuclei and perinuclear clearing.
Diagnosis and Recommendation
Squamous cell cancer of the anal canal. Computed tomography (CT) scans of the abdomen and pelvis are obtained to exclude abdominal lymph node and liver metastasis. Local tumor staging is best performed with an examination under anesthesia and with endoanal ultrasound. This approach is especially useful because anal canal cancers are often too painful to allow a satisfactory examination in the clinic. Suspicious groin lymph nodes should be evaluated with fine-needle aspiration cytology at the same time.
Discussion
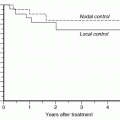
Size, location of the anal cancer, depth of penetration, and lymph node involvement are important prognostic factors. In a study comparing endoanal ultrasound (EAUS) with clinical staging in 50 patients, two thirds of patients with clinical stage 1 and 2 had evidence of muscle penetration ultrasound T staging (UT) 3-4. Overall, there was good correlation among tumor size, depth of penetration, and tumor volume. Depth of penetration has not been incorporated in
the recent tumor, node, metastasis (TNM) staging system. In a multicenter study, EAUS staging of anal cancer was more accurate in predicting tumor recurrence and survival after treatment than traditional clinical staging using tumor height. The ultrasonic T stage was the only significant factor in survival using multivariate analysis. In the presence of nodal metastasis, invasion and grade do not influence survival. Staging the tumor has no therapeutic value because most patients are treated with chemoradiation irrespective of stage. Chemoradiation successfully treats 90% of groin disease; therefore, inguinal node staging is more useful for prognosis rather than for change in therapy.
the recent tumor, node, metastasis (TNM) staging system. In a multicenter study, EAUS staging of anal cancer was more accurate in predicting tumor recurrence and survival after treatment than traditional clinical staging using tumor height. The ultrasonic T stage was the only significant factor in survival using multivariate analysis. In the presence of nodal metastasis, invasion and grade do not influence survival. Staging the tumor has no therapeutic value because most patients are treated with chemoradiation irrespective of stage. Chemoradiation successfully treats 90% of groin disease; therefore, inguinal node staging is more useful for prognosis rather than for change in therapy.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree