Highlights
- •
Lymph node metastasis with extranodal extension was the most important prognostic factor.
- •
Postoperative radiotherapy was associated with a lower risk of recurrence and a good prognosis.
- •
Adenoid cystic carcinoma was associated with a good prognosis.
Abstract
Objectives
Salivary gland cancer is a rare disease composed of more than 20 histological types with different grades of malignancy. The aim of this multicenter, retrospective study was to identify the most important predictors affecting recurrence and survival after surgery.
Material and Methods
A total of 543 patients with salivary gland cancers that underwent curative surgery between 2012 and 2022 in 13 institutions in northern Japan were evaluated in this study. Predictors affecting recurrence and survival were identified by univariate and multivariate Cox regression analyses. Age, sex, primary site, histological type, pathological T status, surgical margin, lymph node metastasis, extranodal extension, and postoperative radiotherapy were the variables evaluated.
Results
Multivariate Cox regression analysis showed that increasing age, submandibular cancer, pathological T status 3 or 4, positive surgical margin, and lymph node metastasis, especially with extranodal extension, were independent risk factors for both recurrence and survival. Sublingual cancer was an independent risk factor for recurrence. Postoperative radiotherapy was associated with a lower risk of recurrence and a good prognosis, and adenoid cystic carcinoma was associated with a good prognosis.
Conclusion
Lymph node metastasis with extranodal extension was the most important prognostic factor affecting both recurrence and survival after surgery, adenoid cystic carcinoma was associated with a good prognosis, and postoperative radiotherapy was associated with a lower risk of recurrence and a good prognosis.
Introduction
Major salivary gland cancer is a rare malignancy that accounts for 5 % of head and neck cancers, with an annual incidence of 0.5–16 per 1,000,000 population . According to the 5th WHO classification, there are more than 20 histological types of salivary gland cancers, including mucoepidermoid carcinoma (MEC), adenoid cystic carcinoma (AdCC), acinic cell carcinoma (ACC), salivary duct carcinoma (SDC), carcinoma ex pleomorphic adenoma (CXPA), squamous cell carcinoma (SCC), and adenocarcinoma not otherwise specified (NOS), which have different clinical behaviors and different prognoses . Although there are exceptions, most MEC, ACC, and CXPA (intracapsular/minimally invasive type) tumors are classified as low-grade malignancies, AdCC (cribriform/tubular types) as intermediate-grade malignancies, and AdCC (solid type), CXPA (invasive type), SDC, and SCC as high-grade malignancies . According to the ESMO clinical practice guideline for salivary gland cancer, surgery is the standard treatment for resectable salivary gland cancer . Previous studies have shown that older age, high-grade histology, higher T classification, positive surgical margin, perineural invasion, and positive lymph node (LN) metastasis are risk factors for recurrence and a poor prognosis . Postoperative radiotherapy (PORT) reduces the risk of recurrence and improves the prognosis in patients with high to intermediate risk characteristics for recurrence . Although there have been many reports of the predictors of recurrence and survival after surgery, they often involved relatively small cohorts with a variety of histological types. To clarify the most important predictive factors for recurrence and survival in a large number of patients, a multicenter, retrospective study that included more than 500 patients who underwent surgery for salivary gland cancers was performed. All 13 university hospitals and cancer centers in the northern area of Japan with a population of 14 million people participated in this study, and factors affecting recurrence and survival were analyzed statistically.
Materials and methods
Patients
This multicenter, retrospective study was conducted from January 2012 through December 2022, and involved patients who underwent surgery for salivary gland cancer for curative intent at the 13 participating hospitals. Patients who underwent surgery for recurrence or who had distant metastases were excluded.
Institutions
This study was conducted at 13 hospitals. All university hospitals and cancer centers in the northern area of Japan, with a population of 14 million people, participated in this study.
Ethics
This study was performed in accordance with the Declaration of Helsinki. The institutional review board approved the study protocol (2023–1-1093) and waived the requirement for informed consent because all data were analyzed anonymously.
Study design
Information about age, sex, primary site of tumor, clinical T and N status based on UICC 8th edition, histology of the tumor, pathological T and N status based on UICC 8th edition, surgical margin, LN metastasis, extranodal extension (ENE), PORT, and information about recurrence or death after surgery was obtained from the medical records. As potential predictors of recurrence and survival, age, sex, primary site of tumor, histology of tumor, pathological T status, surgical margin, LN metastasis, ENE, and PORT were included in the statistical analysis.
Histological diagnosis
Histological diagnosis was performed at each individual institution according to the criteria applicable at the time of treatment. Pathological diagnoses were not reviewed in this study. The diagnosis of SCC was made by excluding other histological types, such as high-grade MEC, and by ruling out metastatic SCC originating from other sites, including the oral cavity, pharynx, larynx, nasal sinuses, skin, and external auditory canal. In this study, CXPA included all cases, not limited to invasive types, and ENE included any type of ENE, not limited to macroscopic ENE.
Statistical analysis
The Kaplan-Meier method was used to estimate disease-free survival (DFS) and overall survival (OS). The log-rank test was used to test significant differences. A Cox proportional hazards model was used for multivariate analysis. Values of p < 0.05 were considered significant. Variables included in the analysis are shown in Supplemental Table 1 . All statistical analyses were performed using R for Mac version 3.5.0 software (R Foundation for Statistical Computing, Vienna, Austria). All statistical calculations were reviewed and validated by specialists in statistics.
Results
A total of 543 patients with salivary gland cancer underwent surgery for curative intent at the 13 participating hospitals from January 2012 to December 2022. The clinical characteristics of the patients are shown in Table 1 . The most common histological type was SDC, followed by AdCC, MEC, CXPA, SCC, adenocarcinoma NOS, and ACC.
| Number of patients | 543 | |
|---|---|---|
| Age (y, median) | 10–91 (65) | |
| Sex (M/F) | 311 / 232 | |
| Primary site | Parotid | 394 |
| Submandibular | 132 | |
| Sublingual | 17 | |
| Clinical stage | I | 70 |
| II | 160 | |
| III | 119 | |
| IVA | 187 | |
| IVB | 7 | |
| Clinical T status | 1 | 86 |
| 2 | 199 | |
| 3 | 141 | |
| 4 | 117 | |
| Clinical N status | 0 | 385 |
| 1 | 39 | |
| 2 | 113 | |
| 3 | 6 | |
| Histology | Salivary duct carcinoma | 116 |
| Adenoid cystic carcinoma | 96 | |
| Mucoepidermoid carcinoma | 77 | |
| Carcinoma ex pleomorphic adenoma | 66 | |
| Squamous cell carcinoma | 34 | |
| Adenocarcinoma NOS | 33 | |
| Acinic cell carcinoma | 30 | |
| Others | 91 |
The postoperative characteristics are shown in Table 2 . There were 165 (31.2 %) patients with positive surgical margins, and 185 (34.1 %) patients with LN metastasis, including 59 (10.8 %) patients with ENE. During a median follow-up period of 39 months, 190 (34.9 %) patients had recurrence of local, LN, or distant metastases.
| Number of patients | 543 | |
|---|---|---|
| Pathological stage | I | 59 |
| II | 116 | |
| III | 129 | |
| IVA | 169 | |
| IVB | 38 | |
| Pathological T status | 1 | 72 |
| 2 | 149 | |
| 3 | 165 | |
| 4 | 125 | |
| Pathological N status | 0 | 358 |
| 1 | 56 | |
| 2 | 92 | |
| 3 | 37 | |
| Surgical margin | Positive | 165 |
| Negative | 363 | |
| Lymph node metastasis | Negative | 358 |
| Positive (ENE-) | 126 | |
| Positive (ENE + ) | 59 | |
| Postoperative radiotherapy | Yes | 297 |
| No | 242 | |
| Recurrence | None | 353 |
| Local | 55 | |
| Lymph node | 57 | |
| Distant | 124 | |
| Follow-up period (months, median) | 1–134 (39) |
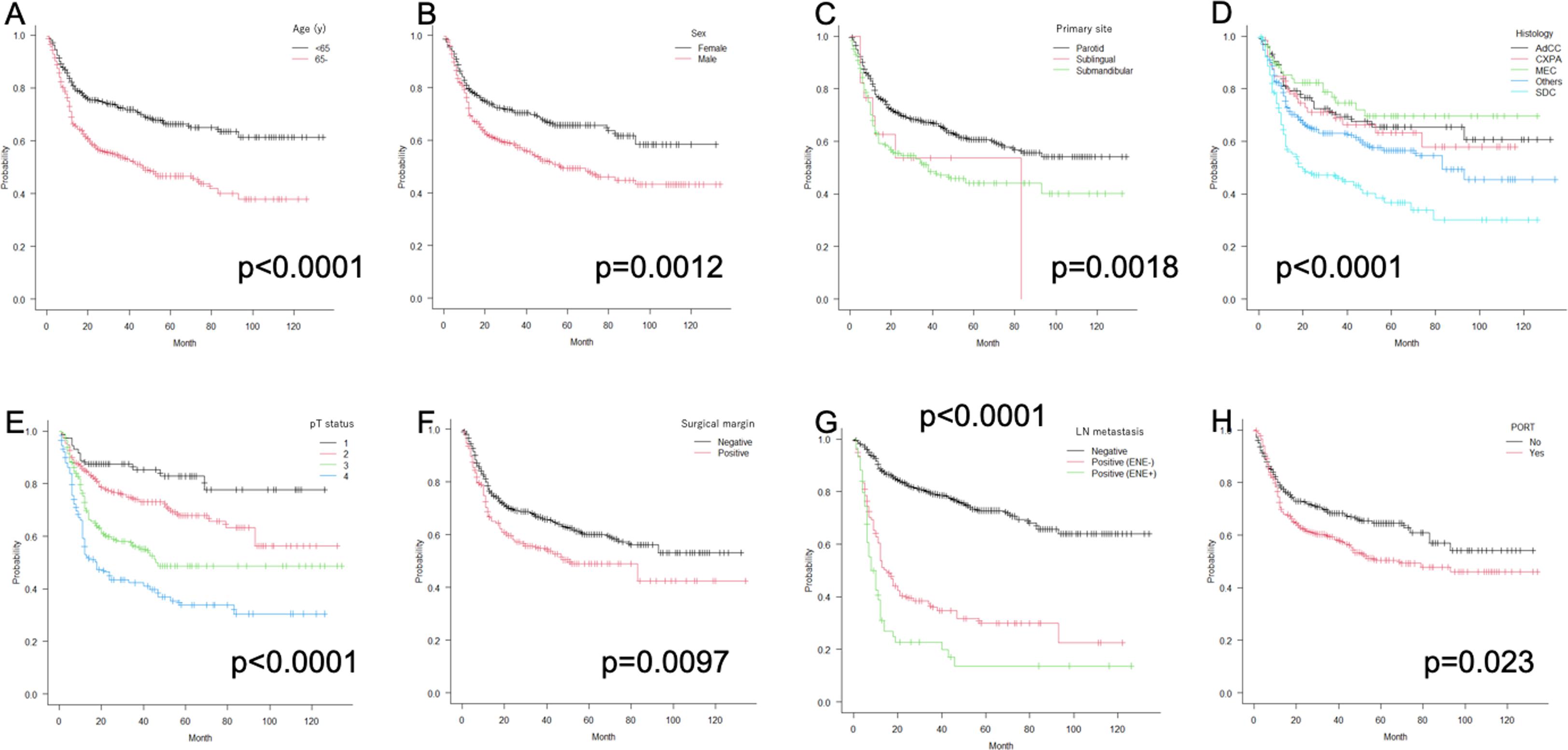
The Kaplan-Meier curves for DFS are shown in Fig. 1 , and 3 to 5-year DFS is summarized in Supplemental Table 2 . Patients over 65 years of age had significantly poorer DFS than the others (p < 0.0001, Fig. 1 A). Male patients had significantly poorer DFS than female patients (p < 0.0012, Fig. 1 B). Patients with submandibular cancer had significantly poorer DFS than those with parotid cancer (p = 0.0018, Fig. 1 C). There were significant differences in DFS among histological types (p < 0.0001, Fig. 1 D) and depending on pathological T status (p < 0.0001, Fig. 1 E). Patients with positive surgical margins had significantly poorer DFS than those with negative margins (p = 0.0097, Fig. 1 F). There was a significant difference in DFS depending on LN metastasis and ENE (p < 0.0001, Fig. 1 G). Patients who received PORT had significantly poorer DFS than those who did not (p = 0.023, Fig. 1 H).

Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree