Highlights
- •
Circumferential defects resulting from surgery of head and neck cancers are a reconstructive challenge for surgeons.
- •
The jejunal free flap requires a single surgical session for harvesting and reconstruction, with a quick return of swallow.
- •
Jejunal free flap has superior outcomes for fistula and stricture rates when compared to other forms of flap reconstruction.
- •
Jejunal free flap has high rates of return to normal diet and speech production, however the latter has its limitations.
Abstract
Pedicled, fasciocutaneous and visceral flaps are all widely adopted for reconstruction after ablative surgery for advanced laryngeal, hypopharyngeal and cervical oesophageal cancers. With multiple options available, the choice depends on type and extent of the defect, patient’s general conditions and institution expertise or preference.
Since its first description in 1959, the use of jejunal free flap (JFF) has been refined thanks to the introduction of microvascular anastomoses, progressively allowing to achieve low mortality and morbidity rates. Both swallowing and speech outcomes are also positively reported across studies.
A systematic review of English literature on JFF in H&N cancer reconstruction published after 2000 was carried out on Medline and Embase. Thirty-six studies were included in the analysis with a total of 3191 JFF reconstructions. Primary outcomes were surgical complications and functional outcomes (quality of speech and oral alimentation). A cumulative review was created pooling complication rates reported in single studies, and overall rates were obtained for fistulas (11.39%), strictures (14.17%), total and partial flap failure (4.79 and 6.15% respectively) and perioperative mortality (3.1%). Functional outcomes were variably reported, with different qualitative and quantitative assessment methods showing overall positive results. When reported, we’ve included impact of adjuvant radiotherapy and the ability of JFF to tolerate it has been widely confirmed. Above results have also been compared with same outcomes registered for different flaps.
Overall, studies over the past 20 years demonstrate good clinical and functional outcomes, proving JFF to be a reliable and safe method for reconstructing circumferential pharyngoesophageal defects.
Introduction
The management of advanced laryngeal, hypopharyngeal and cervical oesophageal cancers, often requires multimodal approach with surgery being either primary treatment or intervening as a salvage. Extensive resections are required to obtain negative margins, resulting in large circumferential defects. Reconstruction aims at maintaining a conduit for food passage as well as providing acceptable speech and swallow functions.
Over the years different reconstruction methods have been developed using various types of flaps. Two types of flaps are generally used, namely pedicled or free flaps. The choice depends on type and extent of the defect, patient’s general conditions, previous treatments to the neck and institution expertise or preference.
Pectoralis major (PM) is the most commonly used pedicled flap for hypopharyngeal defect reconstructions; it is a versatile and reliable flap, easy to harvest and generally gives low donor site morbidity. It can however be too bulky and cause strictures.
Among free flaps, fasciocutaneous free flaps (FCFF) like radial forearm free flap (RFFF) and anterolateral thigh (ALT) are commonly used in reconstructing upper aerodigestive tract (UADT) defects. They are pliable, amenable to shaping and, particularly ALT, is suitable for reconstructing large defects. An issue commonly reported with free flaps is a higher fistula rate, likely related to the multiple suture lines.
Among visceral free flaps both jejunal free flap (JFF) and gastric pullup (GPU) can be used to reconstruct large circumferential pharyngo-esophageal defects. GPU has historically been associated with high mortality and morbidity .
The use of the JFF for reconstruction of the UADT was first described in 1959 by Seidenberg et al. who published their results of an experimental study where they used JFF following a pharyngolaryngectomy . In 1961, Roberts et al. published the first successful case report of this type of reconstruction, where the patient was reported to survive the procedure and regain swallowing function.
Since then, the technique has been progressively refined and higher success rates have been achieved thanks to the introduction and advancement of microvascular procedures . Currently JFF are being used with reasonable outcomes and relatively low mortality and morbidity.
Good functional outcomes both in terms of swallowing and speech are reported for JFF. Advantages in swallowing outcomes are likely related to its intrinsic similarity to pharyngo-oesophageal structures, being jejunum a lubricated, mucosa-lined, tubular structure with peristaltic activity.
In terms of speech rehabilitation, it is generally believed that FCFF provide better voice quality compared to “wet voice” of JFF. However, highly functional tracheo-oesophageal voices following JFF reconstructions, non-inferior to that obtained with FCFF, have been described .
According to recent multidisciplinary guidelines on head and neck (H&N) cancers management, a jejunal flap would be indicated for a circumferential defect with less than 3.5 cm of residual pharyngeal mucosa and when the inferior anastomosis is above the clavicle .
The aim of this systematic review was to compile, evaluate and present surgical complications and provide an accurate representation of oncological and functional outcomes following pharyngoesophageal defects reconstruction with JFF.
Methodology
Search strategy
A systematic review of published literature on JFF in H&N cancer reconstruction was carried out in compliance with the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) guidelines. Medline and Embase were searched with no search filters applied. Combinations of the following free terms and MeSH terms were used: “Jejunum”[Mesh], “Free Tissue Flaps”[Mesh], “Laryngeal Neoplasms”[Mesh], “Esophageal Neoplasms”[Mesh], jejun* free flap, pharyn* cancer*, laryn* cancer*, hypopharyn* cancer*, cervical esophag* cancer*, pharyngoesophageal defect*, laryn* defect*, circumferential defect*, laryngopharyngeal cancer*, laryngopharyngeal defect*. Truncation was used to ensure inclusion of most relevant studies. Duplicate articles were eliminated. Studies which reported at least one of the primary outcomes (defined below), and used JFF for circumferential defects, were included in our analysis. Animal studies, non-English articles, small case series (less than 10 subjects) and case reports, studies where the data of the target patient population could not be separated from other cohorts, review articles, articles with patients with partial or near circumferential pharyngoesophageal defects, patients with circumferential defects not related to H&N cancers (e.g. due to corrosive injuries), patients undergoing JFF where further reconstruction was done; and studies published before the year 2000, were all excluded from this review. In studies with overlapping patient populations, the most recent study was included. Relevant data was collected; data was excluded if not clear for our population of interest or not separated from other patient populations in the study.
Primary outcomes
- •
Surgical complications, recorded as number of events:
- o
Fistula and anastomotic leak rate
- o
Stricture rate
- o
Flap failure; reported cases of total flap loss and flap necrosis were counted under flap failure. Cases where patients were taken to theatre for exploration and review of the microvascular anastomosis, or where a partial flap loss was reported, were counted under partial flap failure
- o
Perioperative mortality; defined as 30 days peri -operatively or during hospital admission following reconstruction
- o
Peri-operative reoperation; defined as 30 days peri -operatively or during hospital admission following reconstruction
- o
- •
Functional outcomes, described in quantitative or qualitative measures:
- o
Quality of speech
- o
Oral alimentation
- o
Secondary outcomes
- •
Donor site morbidity
- •
Other complications
Complication rates recorded in each study were pooled to create a cumulative review.
Results
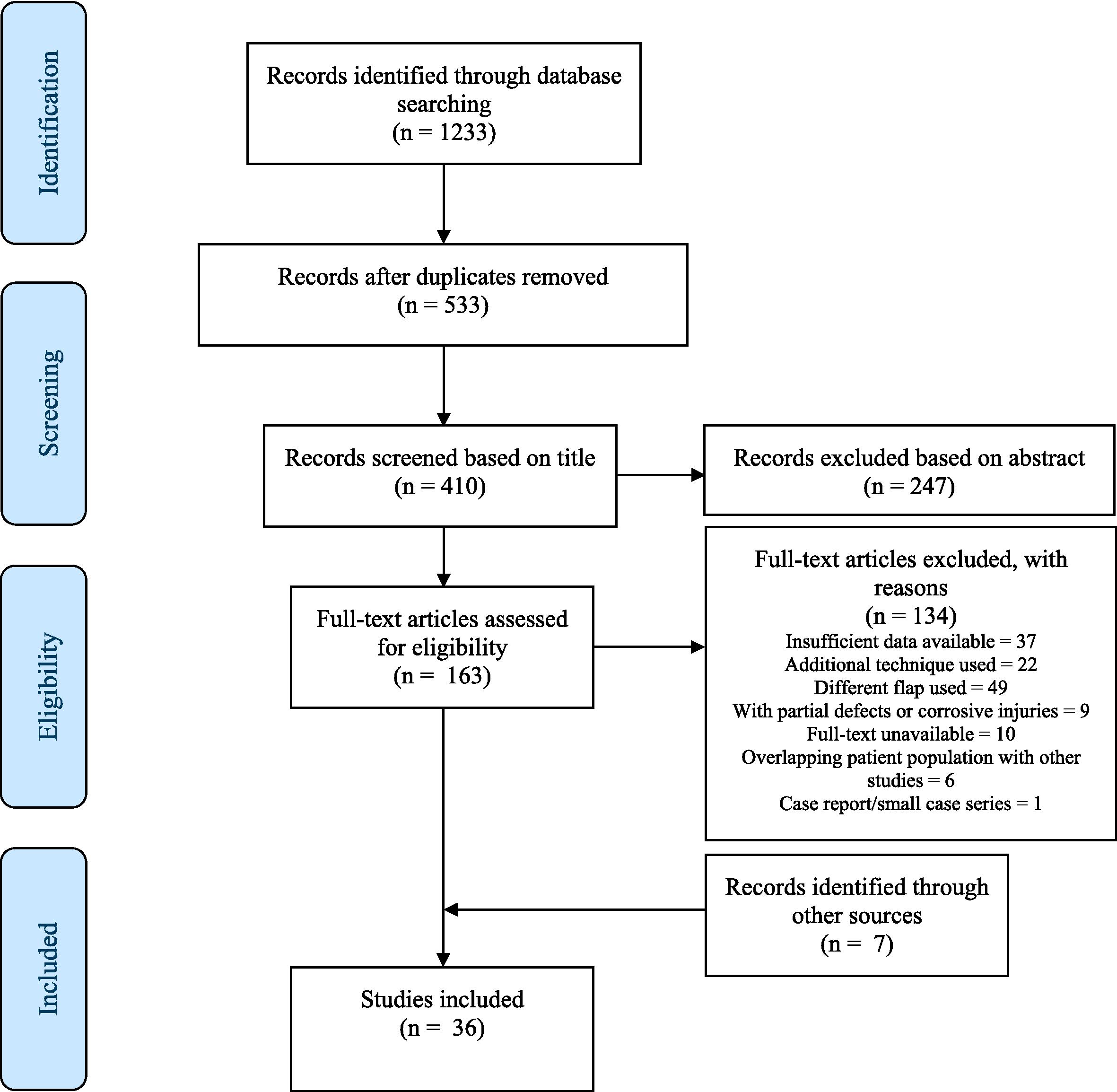
The initial search yielded 1233 articles. After elimination of duplicate results, 533 studies remained for further screening. A further 123 articles were excluded based on title alone, leaving 410 studies to undergo abstract screening to determine eligibility for inclusion. Of these, 163 articles were determined eligible for full text screening, of which 29 articles met the inclusion criteria (reasons for exclusion listed in Figure 1 ). Furthermore, 7 articles that met our inclusion criteria were identified through references of articles and were included in the analysis.
Patient demographics
A total of 3191 reconstructions were analysed, with a male predominance (992 males, 349 females) and a mean patient age of 62.5 years (range 25–93). Primary site of cancer was reported in 17 studies; the most common indication was hypopharyngeal cancer, reported as an indication in 597 patients, with oesophageal (263 patients) and laryngeal (66 patients) cancers ranking as second and third most common indications for reconstruction, respectively. Other indications for reconstruction included thyroid, advanced oropharyngeal and tracheal cancers. Mean hospital stay and follow-up were reported in 11 and 6 studies respectively; patients were hospitalized for a mean of 25.6 days (range 6–350), and followed for a mean of 30 months (range 0.1–162).
Clinical outcomes
All studies reported at least one of the primary clinical outcomes.
Fistula and anastomotic leak ( Table 1 ):
| Reference | Patient No. | No. included | Leak/fistula | Percentage |
|---|---|---|---|---|
| Daiko et al. | 50 | 50 | 2 | 4.00 % |
| Elfeky et al. | 37 | 37 | 3 | 8.11 % |
| Ikeguchi et al. | 22 | 22 | 2 | 9.09 % |
| Lee et al. | 32 | 32 | 1 | 3.13 % |
| Miyata et al. | 58 | 58 | 10 | 17.24 % |
| Ferahkose et al. | 14 | 14 | 0 | 0.00 % |
| Ott et al. | 109 | 109 | 29 | 26.61 % |
| Numajiri et al. | 10 | 10 | 0 | 0.00 % |
| Ida et al. | 14 | 14 | 1 | 7.14 % |
| Laing et al. | 31 | 31 | 3 | 9.68 % |
| Yu et al. | 31 | 31 | 1 | 3.23 % |
| Chang et al. | 168 | 168 | 23 | 13.69 % |
| Triboulet et al. | 77 | 77 | 25 | 32.47 % |
| Chan et al. | 89 | 86 1 | 4 | 4.65 % |
| Chen et al. | 12 | 12 | 0 | 0.00 % |
| Hanson et al. | 23 | 23 | 0 | 0.00 % |
| Hong et al. | 18 | 18 | 1 | 5.56 % |
| Hsieh et al. | 16 | 16 | 5 | 31.25 % |
| Lewin et al. | 31 | 31 | 1 | 3.23 % |
| Nyquist et al. | 24 | 19 2 | 4 | 21.05 % |
| Perez- Smith et al. | 368 | 368 | 30 | 8.15 % |
| Sharp et al. | 19 | 19 | 2 | 10.53 % |
| Walker et al. | 104 | 104 | 11 | 10.58 % |
| Omura et al. | 10 | 10 | 0 | 0.00 % |
| Park et al. | 61 | 61 | 18 | 29.51 % |
| Tan et al. | 10 | 10 | 3 | 30.00 % |
| Mehrara etl al. | 105 | 105 | 8 | 7.62 % |
| Miyamoto et al. | 274 | 274 | 7 | 2.55 % |
| Denewer et al. | 28 | 25 1 | 2 | 8.00 % |
| Sugiyama et al. | 773 | 757 3 | 87 | 11.49 % |
| Keereweer et al. | 51 | 51 | 18 | 35.29 % |
| Total | 2669 | 2642 | 301 | 11.39 % |
| Reference | No. | Salvage cases | Fistula/leak total | Fistula/leak in salvage cases | RR | P-Value |
|---|---|---|---|---|---|---|
| Hsieh et al. | 16 | 5 | 5 | 2 | ||
| Laing et al. | 31 | 11 | 3 | 3 | ||
| Miyamoto et al. | 274 | 79 | 7 | 4 | ||
| Chang et al. | 168 | 80 | 23 | 13 | ||
| Total | 489 | 175 | 38 | 22 | 2.46 | 0.004 |
1 Some patients excluded from further analysis due to flap failure.
2 Some patients excluded from further analysis due to mortality or flap failure.
3 Some patients excluded from further analysis as no information recorded about fistula.
Fistula and anastomotic leak were combined as a single outcome, and were collectively reported in 31 studies. A total of 301/2642 (11.39 %) patients developed fistulas, ranging between 0–35.29 %. Table 1 shows the relationship between developing fistula/anastomotic leak and previous RT (salvage cases); out of 175 salvage cases, 22 patients developed fistula (RR = 2.46, p = 0.004).
Stricture/stenosis ( Table 2 ):
| Reference | Patient No. | No. included | Stricture | Percentage |
|---|---|---|---|---|
| Chan et al. | 89 | 86 1 | 2 | 2.33 % |
| Chen et al. | 12 | 12 | 0 | 0.00 % |
| Hanson et al. | 23 | 23 | 7 | 30.43 % |
| Hong et al. | 18 | 18 | 6 | 33.33 % |
| Hsieh et al. a | 16 | 16 | 1 | 6.25 % |
| Ikeguchi et al. | 22 | 22 | 3 | 13.64 % |
| Laing et al. | 31 | 31 | 3 | 9.68 % |
| Lee et al. b | 32 | 32 | 3 | 9.38 % |
| Lewin et al. | 31 | 31 | 6 | 19.35 % |
| Ni et al. | 18 | 18 | 3 | 16.67 % |
| Nyquist et al. c | 24 | 19 2 | 5 | 26.32 % |
| Perez- Smith et al. | 368 | 368 | 40 | 10.87 % |
| Sharp et al. | 19 | 19 | 6 | 31.58 % |
| Yu et al. | 31 | 31 | 6 | 19.35 % |
| Ferahkose et al. | 14 | 14 | 1 | 7.14 % |
| Ott et al. | 109 | 109 | 27 | 24.77 % |
| Park et al. | 61 | 61 | 19 | 31.15 % |
| Sarukawa et al. | 183 | 183 | 25 | 13.66 % |
| Tan et al. b | 10 | 10 | 0 | 0.00 % |
| Denewer et al. | 28 | 25 1 | 1 | 4.00 % |
| Triboulet et al. | 77 | 77 | 9 | 11.69 % |
| Keereweer et al. | 51 | 51 | 5 | 9.80 % |
| Total | 1267 | 1256 | 178 | 14.17 % |
| Reference | Patient No. | Adjuvant RT | Stricture total | Stricture with RT | RR | P Value |
|---|---|---|---|---|---|---|
| Chen et al. | 12 | 12 | 0 | 0 | ||
| Hanson et al. | 23 | 11 | 7 | 6 | ||
| Laing et al. | 31 | 17 | 3 | 3 | ||
| Nyquist et al. | 24 | 14 | 5 | 5 | ||
| Yu et al. | 31 | 13 | 6 | 4 | ||
| Total | 121 | 67 | 21 | 18 | 4.83 | 0.0082 |
1 Some patients excluded from further analysis due to flap failure.
2 Some patients excluded from further analysis due to mortality or flap failure.
c Distal anastomosis, with tracheoesophageal puncture (TEP).
This complication was reported in 22 studies and was the most commonly reported primary outcome, occurring in 178/1256 patients (14.17 %; ranging from 0–33.3 % among studies). Five studies reported data on 67 patients who underwent adjuvant RT; 18 of these patients developed stricture, with a calculated relative risk (RR) of 4.83 (p = 0.0082) . One study reported the rate of stricture in salvage cases (described in text as pre-operative RT), with stricture developing in 9/86 salvage cases (RR = 0.63, p = 0.24).
Flap failure ( Table 3 ):
| Reference | Patient No. | Failure | Percentage | Partial failure | Percentage |
|---|---|---|---|---|---|
| Chan et al. | 89 | 3 | 3.37 % | ||
| Chen et al. | 12 | 0 | 0.00 % | 0 | 0.00 % |
| Daiko et al. | 50 | 3 | 6.00 % | ||
| Elfeky et al. | 37 | 2 | 5.41 % | ||
| Hanson et al. | 23 | 2 | 8.70 % | 4 | 17.39 % |
| Hong et al. | 18 | 3 | 16.67 % | ||
| Hsieh et al. | 16 | 2 | 12.50 % | ||
| Ikeguchi et al. | 22 | 1 | 4.55 % | ||
| Laing et al. | 31 | 0 | 0.00 % | ||
| Lee et al. a | 32 | 3 | 9.38 % | ||
| Lewin et al. | 31 | 2 | 6.45 % | 1 | 3.23 % |
| Miyata et al. | 58 | 3 | 5.17 % | ||
| Nouarei et al. | 123 | 3 | 2.44 % | ||
| Nyquist et al. | 24 | 2 | 8.33 % | ||
| Perez- Smith et al. | 368 | 11 | 2.99 % | ||
| Walker et al. | 104 | 3 | 2.88 % | 11 | 10.58 % |
| Yu et al. | 31 | 2 | 6.45 % | ||
| Ferahkose et al. | 14 | 1 | 7.14 % | ||
| Mura et al. | 58 | 4 | 6.90 % | ||
| Ott et al. | 109 | 12 | 11.01 % | 10 | 9.17 % |
| Park et al. | 61 | 5 | 8.20 % | ||
| Tan et al. | 10 | 0 | 0.00 % | ||
| Numajiri et al. | 10 | 0 | 0.00 % | ||
| Mehrara et al. | 105 | 3 | 2.86 % | ||
| Miyamoto et al. | 274 | 6 | 2.19 % | 8 | 2.92 % |
| Ida et al. | 14 | 1 | 7.14 % | ||
| Denewer et al. | 28 | 3 | 10.71 % | ||
| Triboulet et al. | 77 | 5 | 6.49 % | ||
| Keereweer et al. | 51 | 5 | 9.80 % | ||
| Total | 1880 | 90 | 4.79 % | 34 | 6.15 % |
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree