Abstract
Prostate cancer (PCa) screening has evolved beyond PSA and digital rectal exam to include multiparametric prostate MRI (mpMRI). Incorporating this advanced imaging tool has further limited the well-established problem of overdiagnosis, aiding in the identification of higher grade, clinically significant cancers. For this reason, mpMRI has become an important part of the diagnostic pathway and is recommended across guidelines in biopsy naïve patients or for patients with prior negative biopsy. This contemporary review evaluates the most recent literature on the role of mpMRI in the screening and diagnosis of prostate cancer. Barriers to utilization of mpMRI still exist including variable access, high cost, and requisite expertise, encouraging evaluation of novel techniques such as biparametric MRI. Future screening and diagnostic practice patterns will undoubtedly evolve as our understanding of novel biomarkers and artificial intelligence improves.
Introduction
Prostate cancer (PCa) remains the second most common malignancy worldwide [ ]. Screening tools have traditionally included serum PSA levels and digital rectal examination, followed by transrectal ultrasound-guided (TRUS) biopsy of the prostate when there is sufficient concern for clinically significant PCa. However, widespread use of PSA screening has led to overdiagnosis of low risk, clinically localized disease. PSA screening has been a contentious topic with studies yielding conflicting results regarding its clinical utility [ , ]. Furthermore, there are well-established significant downsides to PSA screening including false-positive results, complications of prostate biopsy [ ] and overtreatment with negative effects on urinary, bowel, and sexual function [ ]. Better screening tools are needed.
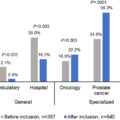
Multiparametric prostate MRI (mpMRI) has emerged as a valuable screening tool in the management of prostate cancer, improving the sensitivity and specificity for detecting clinically significant cancer while avoiding detection of indolent disease [ ]. Review of Medicare SEER data from 2008 to 2015 found that the percentage of men undergoing MRI prior to biopsy skyrocketed from 0.5% to nearly 10% [ ]. More contemporary data from a single, high volume center showed rates of prebiopsy mpMRI increasing from 56% in 2018 to 89% in 2021 suggesting utilization continues to soar [ ]. In 2023 the American Urological Association (AUA) published updated guidelines for the Early Detection of Prostate Cancer which note that MRI may be used prior to initial biopsy for improved detection of Grade Group (GG) 2 and above cancers which aligns with the European Association of Urology Guidelines recommendations [ , ]. Additionally, these guidelines recommend mpMRI for patients with prior negative biopsy who have not yet had a prostate MRI. Furthermore, National Comprehensive Cancer Network (NCCN) guidelines strongly recommend mpMRI as an intermediate step between elevated PSA and prostate biopsy as well as for patients with prior negative biopsy who have not yet obtained an MRI [ ]. Herein, we review the available literature regarding the role of mpMRI in the detection of prostate cancer with an emphasis on the technical details of mpMRI, the role of mpMRI in the biopsy naive and prior negative biopsy settings, biopsy technique, limitations of mpMRI and future directions.
Technical details of prostate MRI
Advances in imaging, namely utilization of multiple functional and anatomic MRI sequences, have allowed for the detection of important prostate cancers while limiting detection of insignificant cancers. Early on prostate MRI focused on T1- and T2-weighted sequences, with the later addition of diffusion-weighted imaging (DWI) allowing for enhanced diagnostic ability [ ]. Prostate MRI first gained traction in the 1980s with a focus on disease staging and initial reports highlighted the challenges in differentiating benign from malignant tissue – a challenge that persists to some degree even today [ , ]. Over the past decade, mpMRI has proved to be an important screening and diagnostic adjunct, contributing additional information regarding the volume and location of suspicious lesions, while helping inform the decision regarding who to biopsy [ ].
To briefly review the role of each imaging phase:
T1-weighted sequence: This fat-enhancing sequence provides high resolution morphologic detail and is typically most useful for evaluating pelvic lymph nodes and bony structures. The T1 sequence is also useful in differentiating postbiopsy hemorrhage from tumor, as postbiopsy hemorrhage is more pronounced on T2 sequences than on T1 [ ].
T2-weighted sequence: T2-weighted imaging sequences provide high resolution morphologic detail through enhanced signals from water and are a cornerstone of mpMRI. PCa appears hypointense on T2 due to its relatively higher cellularity and lower water content; the degree of hypodensity has been shown to be associated with Gleason grade [ , ]. T2-weighted sequences are less effective in the transition zone which also has relatively high cellularity [ ].
Diffusion Weighted Imaging (DWI) sequence : This functional sequence quantifies the amount of water molecule movement within a tissue; the high cellularity of PCa has a lower amount of random water molecule movement as compared to normal prostate tissue [ ]. Given this, DWI sequences are useful especially in the transition zone. One meta-analysis found that combining DWI with T2-weighted imaging sequences allows for increased specificity and relatively lower sensitivity as compared to T2-weighted sequences alone [ ].
Dynamic contrast-enhanced (DCE) imaging sequence: This functional sequence uses gadolinium contrast to show differentiation in rates of uptake in malignant prostatic cells vs. benign cells, although certain benign prostatic processes such as prostatitis may also cause increased contrast uptake [ ].
Additional techniques have also shown utility for prostate cancer diagnosis, such as utilization of an endorectal coil and spectroscopy imaging. The use of an endorectal coil improves image quality and in meta-analysis has been shown to increase sensitivity but confers additional cost and patient discomfort [ ]. Magnetic resonance spectroscopy imaging (MRSI) requires an endorectal coil and allows for visualization of the relative rates of change of prostatic metabolites such as citrate and choline, although the main use of MRSI remains academic due to cost and availability limitations [ ].
The Prostate Imaging Reporting and Data System (PI-RADS) reporting system was developed to decrease variability in radiologist reports (originally a Likert scale for subjective radiologist suspicion was used in reporting) via a standardized scoring criteria, and the first version was published in 2012 [ , ]. PI-RADS version 2 represented a streamlined version, published in 2015, with changes including omitting MRSI, simplifying sequence interpretation, and defining key sequences specific to each prostatic zone [ ]. Compared to the first version, PI-RADS v2 demonstrated increased sensitivity and similar specificity [ ]. Notably, while PI-RADS evaluates the cancerous risk of a prostatic lesion, it does not report on additional information that may be gleaned from mpMRI such as seminal vesicle involvement, lymph node involvement, and bony pelvic metastases. The most updated version, PIRADS 2.1, was published in 2019 with the goal of facilitating improved detection, localization, and risk stratification among patients with suspected prostate cancer.[ ] This latest scoring system has contributed to increased utilization of mpMRI and further streamlined reporting, although still requires a well-experienced radiologist for optimal interpretation [ ].
More recently, biparametric MRI (bpMRI) has garnered interest due to several advantages including avoidance of contrast (and thus the cost and potential adverse reactions), shorter time in the MRI scanner, and broader patient access [ ]. This protocol avoids need for contrast by utilizing only T2-weighted and DWI sequences and available data indicate comparative accuracy to mpMRI [ , ]. While still investigational, this limited protocol has appeal and more data will help elucidate which patients and clinical scenarios bpMRI may be most appropriate.
Prostate MRI as a prebiopsy step in the diagnostic pathway
Multiparametric prostate MRI provides actionable information for clinicians and patients considering whether to pursue prostate biopsy. While patients with significantly elevated PSA certainly warrant biopsy, strong evidence demonstrates the utility of mpMRI as a prebiopsy tool to limit detection of indolent disease, improve detection of significant disease, and potentially allow for a more limited biopsy or avoid systematic biopsy altogether in some patients.
The PROMIS trial was a multicenter paired cohort confirmatory study, where 576 patients underwent mpMRI, followed by both standard TRUS biopsy for comparison and a transperineal template-mapped biopsy to achieve a saturation reference. The authors found that mpMRI was more sensitive and less specific than standard TRUS biopsy and suggested that mpMRI alone would allow 27% of patients to avoid a primary biopsy and diagnose 5% fewer clinically insignificant cancers [ ]. The PRECISION trial involved 500 biopsy naïve men randomized to either mpMRI plus mpMRI-targeted biopsy or standard TRUS biopsy. Notably, in this study, 28% of men in the mpMRI-targeted biopsy arm had mpMRI results that were not suggestive of PCa, and so they did not undergo biopsy. The authors found that the mpMRI + targeted biopsy arm detected clinically significant PCa in 38% of men vs. 26% of men who underwent standard TRUS only [ ]. The authors additionally found 13% fewer clinically insignificant cancer detected in the mpMRI + targeted biopsy arm as compared to the standard TRUS arm [ ]. Similarly, a 2019 meta-analysis of 18 studies found that, compared to upfront systematic biopsy, mpMRI followed by mpMRI-guided biopsy for only suspicious lesions (nonsuspicious lesions were not biopsied) increased the rate of detection of clinically significant PCa while decreasing the rate of clinically insignificant PCa [ ]. A real-world study of 2,900 men found that mpMRI use led to biopsy avoidance in 31% of men [ ].
Indeed, the negative predictive value (NPV) is paramount in the mpMRI role as triage test. The PROMIS trial showed an NPV of 76% for mpMRI, compared to NPV of 63% for TRUS biopsy [ ]. A 2015 meta-analysis of 12 articles in 2015 found an NPV ranging from 63% to 98% [ ]. A larger meta-analysis of 48 studies found a median NPV of 82% for any PCa and 88% for clinically significant PCa; interestingly, the NPV estimates decreased when overall PCa prevalence within the study populations increased [ ]. These results suggest that NPV ranges are highly dependent on the underlying prevalence of PCa within the population, and that mpMRI may be most useful as a triage test when the underlying prevalence of PCa is low. The false positive rate of mpMRI has been found to range from 42% to 92% and occurs due to benign lesions such as prostatitis and benign hypertrophic nodules, while also highlighting the importance of a well-trained radiologist [ ].
The MRI-FIRST was a multicenter, prospective trial which found that adding MRI with subsequent targeted biopsy maximized detection of clinically significant cancer when combined with systematic biopsy among biopsy naïve patients regardless of biopsy technique employed [ ]. All patients underwent MRI followed by 12-core systematic biopsy by operator blinded to MRI results and finally, targeted biopsy by another operator if an MRI region of interest was identified. Detection of clinically significant cancer was higher with targeted biopsy (7.6% vs. 5.6%) with fewer low grade cancers found (5.5% vs. 22.3%), although detection of GG2 and above was highest when both systematic and targeted were utilized.
Nomograms and risk calculators using patient variables such as age, PSA, digital rectal exam, and prior biopsy results have long been incorporated into the management of elevated PSA to assess patient risk. Often these tools are part of the shared decision-making process prior to biopsy or repeat biopsy. More recently, MRI results have been incorporated into nomograms as a data point yielding superior accuracy for the detection of clinically significant cancer in both biopsy naïve and prior negative biopsy patients [ , ].
The role of mpMRI in setting of prior negative biopsy
mpMRI may also informs the decision to biopsy in men who have had prior negative biopsy. In 2016, an expert panel collaborative initiative was undertaken by AUA and the Society of Abdominal Radiology (SAR) to address role of mpMRI and targeted biopsy in patients with history of prior negative prostate biopsy. The panel concluded, based on available data, that mpMRI with targeted biopsy should be performed prior to repeat biopsy [ ]. Today, this practice is recommended by guidelines for such patients when there is ongoing concern for clinically significant prostate cancer [ ].
Patients with prior negative biopsy may have suspicious MRI lesions for targeting on subsequent biopsy which diagnoses clinically significant cancers missed on earlier systematic only biopsy. In one case series including 105 patients with prior negative biopsy and persistently elevated PSA, mpMRI followed by fusion biopsy (targeted and systematic) demonstrated improved detection with diagnosis of clinically significant disease (GG2 and above) in 91% of targeted biopsies compared to 54% of systematic biopsies [ ]. Another study evaluated 195 men with prior negative biopsies who subsequently underwent mpMRI; men with suspicious mpMRI underwent both standard TRUS biopsy and mpMRI-targeted biopsy. Thirty-seven percent of patients were found to have PCa on repeat biopsy, with 55% of those men found to have high grade cancer detected only on the mpMRI-targeted biopsy, not on the standard TRUS biopsy [ ]. Additionally, 39% of the men found to have PCa were pathologically upgraded on mpMRI-targeted biopsy as compared to standard TRUS, emphasizing both the diagnostic and prognostic value of mpMRI [ ]. In a multi-institutional analysis of 779 men with prior negative biopsies who subsequently underwent repeat mpMRI-targeted biopsy plus standard TRUS biopsy, a similar result of improved detection with mpMRI-targeted biopsy as compared to standard TRUS biopsy was found [ ]. Interestingly, on multivariate analysis, the number of prior negative standard biopsies was a negative predictor for PCa diagnosis on repeat standard TRUS biopsy, but not associated with PCa diagnosis on mpMRI-targeted biopsy [ ].
The PICTURE study utilized a paired-cohort confirmatory design, where 249 men with prior negative biopsies underwent mpMRI and transperineal template prostate mapping biopsies as a saturation reference. Using a Likert score of ≥3 as a cutoff value for mpMRI suspicion, the authors found a sensitivity of 94% and NPV of 69% for detecting high risk diseasex [ ].
mpMRI-guided biopsy improves detection of clinically significant PCa
As highlighted above, mpMRI impacts decision-making in men being screened for prostate cancer while further aiding in the diagnosis of important cancers through targeted sampling. While standard systematic biopsy remains a mainstay in PCa diagnosis in the US, the mpMRI-guided, or mpMRI targeted biopsy is increasing in popularity.
A prospective cohort study of 1,003 men who underwent both mpMRI-targeted and standard TRUS biopsy found that mpMRI-targeted biopsy diagnosed 30% more high risk cancers vs. standard biopsy and 17% fewer low risk cancers [ ]. Another randomized clinical trial of 212 biopsy naïve patients found that detection of any PCa and clinically significant PCa were higher in patients who underwent mpMRI-targeted biopsy plus standard TRUS biopsy as compared to patients who underwent standard TRUS biopsy alone [ ]. Again, this was shown in the MRI-FIRST prospective study where the combination of standard TRUS + mpMRI-targeted biopsy showed added value compared to standard TRUS alone or targeted biopsy alone for finding >GG1 disease, but systematic biopsies added significantly more indolent cancer diagnoses [ ]. This also highlights the challenges in interpreting data regarding the role of mpMRI include the evolution of radiologist reporting, as well as the variety of reference techniques used (i.e. targeted biopsy, saturation biopsy, etc.).
Some studies have used prostatectomy specimens as references for which to assess MRI-guided biopsy accuracy. One study enrolled 246 consecutive patients who underwent robot-assisted radical prostatectomy following diagnosis of PCa via either standard TRUS biopsy alone or mpMRI-targeted biopsy alone; mpMRI-targeted biopsy correctly classified the Gleason score in 53% of patients who underwent standard TRUS biopsy as compared to 91% of patients who underwent mpMRI-targeted biopsy [ ].
Avoidance of systemic biopsy completely in favor of mpMRI-targeted biopsy alone has been shown to decrease the rate of overdiagnosis of low-grade PCa. The Goteborg-2 Trial Investigators screened nearly 18,000 men with PSA and MRI followed by randomization to systematic and targeted biopsy (reference group) or MRI-targeted biopsy only (experimental group) [ ]. Only 66 participants (0.6%) in experimental group were diagnosed with clinically insignificant cancer compared to 72 (1.2%) in the reference group, demonstrating an overdiagnosis reduction of half, at the expense of 10 patients being diagnosed with GG 2 disease. Interestingly, however, there is some question regarding the true real-world behavior of “clinically significant” PCa identified on mpMRI-targeted biopsy alone. A retrospective study of 999 men w negative standard TRUS biopsy + positive mpMRI-targeted biopsy as compared to 3,056 men followed for 11 years after the ERSPC trial found that while mpMRI-targeted biopsy detected a large amount of high risk cancer, those patients with PCa solely identified on mpMRI-targeted biopsy had lower rates of PCa mortality than would be expected [ ]. Ultimately, it remains a balancing act where avoiding systematic biopsy results in missed high grade cancers, while performing systematic biopsy unavoidably diagnoses low grade cancers.
Importantly, evidence supporting the superiority of biopsies with MRI targeting is built on biopsy pathology which is not always reflective of final pathology after radical prostatectomy. One method of assessing the significance of tumors detected by MRI targeting has been to examine the concordance between biopsy grade and pathologic grade following surgery. A systematic review and meta-analysis found that both MRI-targeted biopsies alone and combined targeted and systematic biopsies decrease rates of upgraded pathology and increase rates of pathologic concordance with RP as compared with systematic biopsies [ ]. However, combined biopsies were also found to have higher odds of downgraded final pathology which raises a concern for targeted biopsies to have a potential net harm as significant downgrading suggests unnecessary or overtreatment.
Biopsy technique
In 2024, there are many ways to approach prostate biopsy given recent advancements in imaging and technology. These include cognitive fusion and software-assisted fusion MRI-targeted biopsies, which may be performed via a transrectal (TR) or transperineal (TP) approach and prostate biopsies that be conducted in-bore. Cognitive registration requires the operator to recall the MRI lesions for targeting on live ultrasound imaging while software-assisted platforms overlay segmented MRI images atop the real-time ultrasound. In-bore biopsies are performed in the MRI suite which has been to be resource intensive and expensive. It remains that obtaining adequate tissue impacts management and is paramount for best care.
There are several studies comparing targeted biopsy techniques. In the PROFUS Trial, Wysock et al.[ ] compared cognitive and computer software-assisted targeting in 125 consecutive patients with MRI lesions who underwent both targeting approaches (and systematic biopsy) in the same setting transrectally . There was no difference in cancer detection rates, although software-assisted fusion was more accurate for detecting cancer in smaller regions of interest. Hamid et al.[ ] conducted a prospective, within-person randomized trial, SmartTarget, comparing accuracy of cognitive fusion and software-assisted fusion TP biopsy for risk stratification . One hundred and forty-one men with prior TR biopsy and ≥PIRADS 3 or greater MRI lesion underwent fusion TP biopsy with both cognitive and software fusion and detection rates of clinically significant cancers were compared, targeting lesions only. Findings indicate that combined biopsy – cognitive and software fusion – yielded the highest cancer detection rates over either form of targeting individually. A 2023 systematic review and meta-analysis found no difference in the detection of clinically significant cancers across 8 comparative studies with authors concluding that choice of approach is at the clinician’s discretion and should be based on experience [ ].
The FUTURE Trial was a multicenter randomized control trial comparing overall and clinically significant cancer detection rates among nearly 700 patients undergoing cognitive registration, software-assisted, and in bore MRI biopsies following prior negative biopsy [ ]. The in-bore and cognitive fusion biopsies were obtained via a transrectal approach while the software-assisted fusion biopsies were transperineal. There were no significant differences in detection rates overall or for clinically significant disease. An earlier systematic review and meta-analysis evaluated these same 3 techniques and found greater overall cancer detection with in-bore biopsies when compared to cognitive fusion and similar detection to software-assisted fusion biosy [ ]. Overall, available evidence suggests no one technique is superior to the other when it comes to targeting of MRI lesions.
Studies Evaluating Impact of Biopsy Technique on Cancer Detection.
| PROFUS Trial | Wysock, J. S. et al. A prospective, blinded comparison of magnetic resonance (MR) imaging-ultrasound fusion and visual estimation in the performance of MR-targeted prostate biopsy: the PROFUS trial. Eur Urol 66 , 343–351,2014. |
| SmartTarget Trial | Hamid, S. et al. The SmartTarget Biopsy Trial: A Prospective, Within-person Randomised, Blinded Trial Comparing the Accuracy of Visual-registration and Magnetic Resonance Imaging/Ultrasound Image-fusion Targeted Biopsies for Prostate Cancer Risk Stratification. Eur Urol 75 , 733–740,2019. |
| FUTURE Trial | The FUTURE Trial: A Multicenter Randomised Controlled Trial on Target Biopsy Techniques Based on Magnetic Resonance Imaging in the Diagnosis of Prostate Cancer in Patients with Prior Negative Biopsies. Eur Urol 75 , 582–590, 2019. |
| Systematic Reviews and Meta-analyses | Pirola, G. M. et al. Transperineal US-MRI Fusion-Guided Biopsy for the Detection of Clinical Significant Prostate Cancer: A Systematic Review and Meta-Analysis Comparing Cognitive and Software-Assisted Technique. Cancers (Basel) 15, 2023. Wegelin, O. et al. Comparing Three Different Techniques for Magnetic Resonance Imaging-targeted Prostate Biopsies: A Systematic Review of In-bore versus Magnetic Resonance Imaging-transrectal Ultrasound fusion versus Cognitive Registration. Is There a Preferred Technique? Eur Urol 71 , 517–531, 2017. |
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree