Highlights
- •
Our study explores the efficacy of prostate ablation, both whole-gland and partial-gland ablation, as an emerging treatment for localized prostate cancer, emphasizing its potential in reducing quality of life burdens compared to traditional radical treatments.
- •
The choice of prostate ablation modality as well as the choice between whole and partial gland ablation should be tailored based on the patient’s and tumor’s characteristics.
- •
The study reports promising short- to mid-term outcomes for prostate ablation with good genitourinary and oncological outcomes- pathological failure rates of 6.1% for whole-gland ablation and 16.8% for partial-gland ablation.
- •
Approximately one-third of patients experienced minor complications (Clavien-Dindo 1-2) within 30 days, highlighting the safety of these ablation techniques.
Abstract
Purpose
To evaluate the oncological and genitourinary outcomes of various forms of prostate ablation for localized prostate cancer.
Methods
A prospectively managed database included men with localized prostate cancer who underwent prostate ablation during January 2018-August 2023. Patients received either whole or partial-gland ablation using 1 of 3 energy modalities: cryotherapy, High Intensity Focused Ultrasound (HIFU), or Irreversible electroporation (IRE).
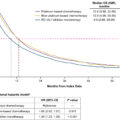
The primary endpoints included biochemical recurrence (BCR), imaging failure (IF) and pathological failure (PF). The secondary endpoints included complication rate at 30 days and genitourinary function.
Results
150 consecutive patients were included, of them 49 (32.7%) underwent whole-gland therapy and 101 (67.3%) underwent partial-gland therapy. The whole-gland therapy subgroup included cryoablation (39, 79.6%) and HIFU (10, 20.4%) and the partial-gland therapy subgroup included cryoablation (50, 49.5%), HIFU (30, 29.7%) and IRE (21, 20.8%). The median follow-up time was 32.6 months (IQR, 19.2–47.0) and 14.8 months (IQR, 9.5–31.9) in the whole-gland and partial-gland therapy subgroups, respectively. The rate of PF was 6.1% and 16.8% in the whole and partial gland groups, respectively. Whole-gland cryoablation had the most prominent positive impact on AUA-SS score and negative impact on SHIM score. Among patients undergoing partial gland ablation there was no significant impact on urination and erections at 12 months and 90% of potent men retained their potency. Approximately one-third of the patients experienced minor postoperative complications within 30 days.
Conclusion
Our findings conclude that ablation is a safe treatment option for localized prostate cancer, with satisfactory oncological outcomes and minimal short-intermediate-term morbidity.
Patient Summary
In this study we looked at whole- and partial-gland ablation therapies for localized prostate cancer and found satisfactory oncological outcomes and minimal impact on urinary and sexual function with short-intermediate-term follow-up.
1
Introduction
Traditional radical treatments for prostate cancer (PCa) result in a high burden on the patient’s quality of life (QoL) [ , ]. As the use of multi-parametric MRI (mpMRI) and other diagnostic tools continues to evolve to localize better and risk-stratify the disease, the demand for innovative therapeutic treatments continues to grow [ ].
Prostate ablation (PA) has emerged as 1 such novel treatment and represents a significant advancement in the management of PCa. PA includes a variety of energy modalities including but not limited to cryotherapy, high intensity focused ultrasound (HIFU), and irreversible electro-corporation (IRE) [ , ]. Whole-gland ablation (WGA), destroys the prostate gland in its entirety, while partial-gland ablation (focal therapy- FT) treats a region of interest and has demonstrated efficacy with reduced impact on QoL [ ].
As momentum builds for a more expansive application of FT, discerning whether it or WGA is more appropriate will be of paramount clinical importance. Determining the ideal use case for each relies heavily on clinician experience, as strong, evidence-based guidelines do not yet exist for FT [ ]. The same challenge exists when choosing the type of energy modality. Thus, despite the growing evidence that PA in its various forms provides optimal oncologic control in the context of reduced side effects [ ], the need for additional longitudinal data remains high. Our work seeks to shrink this knowledge gap.
2
Materials and methods
2.1
Study population
From January 2018 to August 2023, 223 men with PCa underwent PA for the management of localized PCa at the University of Cincinnati Medical Center and Cincinnati Veteran Affairs Medical Center. Demographic, clinical, pathologic, and imaging data were available on 150 consecutive men, through an IRB-approved prospective registry and database. Patients in our study received either WGA or FT guided by MRI-US fusion biopsy using 1 of the 3 energy modalities: cryotherapy (Cryocare® System, Endocare Inc., Austin, TX), HIFU (Sonablate® system, Sonacare Medical, Charlotte, NC), or IRE (NanoKnife® System, AngioDynamics, Latham, NY).
2.2
Selection and administration of appropriate therapy
PA as a treatment option was primarily offered to patients with National Comprehensive Cancer Network (NCCN) intermediate risk category patients: grade group (GG) 2 or 3 with PSA below 20ng/ml. Patients with unifocal, unilateral, or anterior-only clinically significant (CS) disease (defined as GG2 or higher) corresponding to mpMRI visible lesion(s) were offered FT. Generally, for FT, we utilized IRE for unifocal anterior tumors, cryotherapy for larger anterior tumors or hemi-ablations (when multiple lesions were present on the same side of the prostate), and HIFU primarily for posterior lesions. However, these guidelines were flexible, and we adjusted our treatment plan based on patient preferences, functional status, and insurance coverage. The majority of our focal procedures were performed using mpMRI fusion system. We have previously published our technique of mpMRI-Ultrasound fusion-guided focal cryoablation utilizing the ARTEMIS™ platform (Eigen Inc., Grass Valley, CA) [ ]. The patient’s annotated mpMRI was used for 3D reconstruction and image fusion during a live trans rectal ultrasound (TRUS). Needle probes were placed, and cryoablation of the lesion was performed for 2 freeze-thaw cycles, creating a circumferential 1 cm treatment margin. A similar technique was used for focal IRE cases. In select cases, template ablation was performed when systematic cores around the MRI visible lesions were noted to be positive for cancer. Template ablations were performed under ultrasound guidance alone. WGA for unilateral or bilateral CS disease was offered only when patients were ineligible or poor candidates for “standard of care” surgery or radiation therapy options or adamantly declined these. Patients with high-risk prostate cancer were only offered PA if they were at a significantly high risk of morbidity from surgery or radiation therapy.
2.3
Follow up
2.3.1
Partial-gland
Patients were scheduled for postoperative follow-up appointments every 3 months during the first year and every 6 months thereafter. During these appointments, patients completed 2 questionnaires – the American Urological Association Symptom Score (AUA-SS) and the Sexual Health Inventory for Men (SHIM), in addition to prostate-specific antigen (PSA) testing. Patients additionally were asked about their ability to maintain erections sufficient for penetrative sex, medication use for ED, and urinary incontinence. At the 6 to 9 months postoperative window, patients underwent a prostate mpMRI followed by ‘protocol’ transrectal (TR) or transperineal (TP) prostate biopsy. The biopsy technique consisted of obtaining 2 to 4 targeted cores from the ablated zone(s) and any new lesion(s) seen on mpMRI, followed by a random 12-core systematic prostate biopsy. For patients with negative ‘protocol’ biopsy, further mpMRI were obtained at 24 months post-treatment, followed by every 2 years. Further biopsies were performed only on a “for cause” basis, triggered by abnormal mpMRI or abnormal trend in PSA. Patients with GG1 on ‘protocol’ biopsy were assigned to active surveillance.
2.3.2
Whole -gland
Patients receiving WGA therapy underwent a similar follow-up regimen in terms of PSA and QOL questionnaires. However, prostate imaging and biopsy were done only when a patient experienced biochemical recurrence (BCR).
2.4
Primary and secondary outcomes
We defined 3 primary oncological outcomes: BCR, imaging failure (IF), and pathological failure (PF). BCR was defined as an increase in PSA level greater than 2 ng/mL above the nadir (Phoenix criteria) following PA confirmed by a repeat check. The use of the Phoenix criteria to define BCR has been reported as a useful tool following both WGA and FT [ , ]. IF was defined as identifying any new lesion with PI-RADS score of 4 or higher in the non-ablated zone as well as the presence of residual disease in the ablated zone on postoperative prostate mpMRI. IF was counted as such even if PF was not confirmed on protocol biopsy. PF was defined as a positive prostate biopsy detecting CS disease on a follow-up biopsy. In-field and out-of-field recurrence were defined as a positive biopsy with CS disease in the ablated and non-ablated zones, respectively.
The secondary outcomes included complication rate in 30 days post treatment and genitourinary function. Severe postoperative complications were defined as Clavien-Dindo grade 3 or higher. Continence was described as being pad-free. Loss of potency was defined as the patient’s self-reported inability to achieve erections suitable for sexual intercourse with or without oral medications.
2.5
Statistical analysis
Descriptive statistics consisted of medians and interquartile ranges (IQR) for continuous variables and proportions for categorical variables. Variation over time of continuous variables was represented by box and whisker and spaghetti plots. To assess the time following treatment to BCR, IF, and PF, nonparametric Kaplan-Meier (KM) curves were used to estimate the survival probability of these failures. A 2-sample median test was performed to compare the SHIM medians, and a 2-proportion Z test was used to compare the postoperative complication rate. All statistical analyses were performed using SAS software (V9.4, SAS Institute Inc., Cary, NC).
3
Results
3.1
Baseline and pre-operative characteristics
150 patients were included in the analysis. 49 patients underwent WGA, 39 of which received cryotherapy (w-cryo) and 10 received HIFU (w-HIFU). 101 patients underwent FT, 50 of which received cryotherapy (p-cryo), 30 received HIFU (p-HIFU), and 21 received IRE (p-IRE). A total of 19 patients (12.67%) underwent salvage ablation following radiation therapy. The remaining patients received primary ablation treatment without any prior interventions ( Table 1 ). In the FT group, 69 (68.3%) patients were treated for a single index lesion, while 27 (26.7%) received templated hemi-ablations ( Supplementary table 1 ). Median follow-up time was 32.6 months (IQR, 22.7–50.2) and 14.8 (IQR, 9.5–31.9) for WGA and FT, respectively. The median (IQR) SHIM score was considerably higher in patients undergoing FT compared to WGA (16 (7–21) vs. 6.5 (1–14), P = 0.0019). Additional baselines characteristics are detailed in Table 2 . Majority of patients had intermediate-risk PCa with 42 (85.7%) and 96 (95%) patients in WGA and FT groups, respectively ( Table 3 ).
| Whole Gland | Partial Gland | Total | |
|---|---|---|---|
| Cryoablation | 39 (26.00) | 50 (33.33) | 89 (59.33) |
| HIFU | 10 (6.67) | 30 (20.00) | 40 (26.67) |
| Irreversible Electroporation | 0 (0.00) | 21 (14.00) | 21 (14.00) |
| Total | 49 (32.67) | 101 (67.33) | 150 (100.0) |
| Salvage (post radiation) | 9 (6.00) | 10 (6.67) | 19 (12.67) |
| Non-salvage | 40 (26.67) | 91 (60.67) | 131 (87.30) |
| Total | 49 (32.67) | 101 (67.33) | 150 (100.0) |
| Whole Gland (n=49) | Partial Gland (n=101) | Total (n=150) | ||||||
|---|---|---|---|---|---|---|---|---|
| Cryoablation (n=39) | HIFU (n=10) | Sub-total | Cryoablation (n=50) | HIFU (n=30) | IRE (n=21) | Sub-total | ||
| Follow-up time, months (IQR) | 35.8 (22.7-50.2) | 25.5 (16.3-42.0) | 32.6 (19.2-47.0) | 25.1 (10.3-36.7) | 18.4 (11.2-30.5) | 9.8 (5.0-13.0) | 14.8 (9.5-31.9) | 23.6 (10.8-36.5) |
| Median age, years (IQR) | 69 (65.0-74.0) | 68 (65.0-72.0) | 69 (65.0-73.0) | 65 (59.0-71.0) | 66.5 (64.0-70.0) | 71 (66.0-74.0) | 67 (62.0-72.0) | 68 (63.0-72.0) |
| Race, n (%) | ||||||||
| Caucasian | 21 (53.8) | 9 (90.0) | 30 (61.3) | 35 (70.0) | 25 (83.3) | 19 (90.5) | 79 (78.2) | 109 (72.7) |
| African American | 16 (41.0) | 1 (10.0) | 17 (34.7) | 13 (26.0) | 4 (13.3) | 2 (9.5) | 19 (18.8) | 36 (24.0) |
| Asian | 1 (2.6) | 0 (0.0) | 1 (2.0) | 1 (2.0) | 1 (3.3) | 0 (0.0) | 2 (2.0) | 3 (2.0) |
| Other | 1 (2.6) | 0 (0.0) | 1 (2.0) | 1 (2.0) | 0 (0.0) | 0 (0.0) | 1 (1.0) | 2 (1.3) |
| Median PSA, ng/mL (IQR) | 7.83 (4.9-11.85) | 6.87 (5.2-8.15) | 7.59 (5.05-10.2) | 5.87 (3.64-9.2) | 5.83 (4.6-9.26) | 6.62 (5.1-9.04) | 5.98 (4.42-9.2) | 6.6 (4.47-9.4) |
| Median mpMRI prostate volume, mL (IQR) | 35.65 (25.5-45.3) | 33.3 (20-45.38) | 34.05 (23.21-45.34) | 41.3 (27.6-53.1) | 31.0 (26.3-39.0) | 35.1 (31.0-43.0) | 35.5 (27.6-48.3) | 35.3 (26.6-46.5) |
| Highest PI-RADS score, n (%) | ||||||||
| 3 | 1 (2.6) | 2 (20.0) | 3 (6.1) | 4 (8.0) | 2 (6.7) | 3 (14.3) | 9 (8.9) | 12 (8.0) |
| 4 | 11 (28.2) | 2 (20.0) | 13 (26.6) | 17 (34.0) | 10 (33.3) | 2 (9.5) | 29 (28.7) | 42 (28.0) |
| 5 | 16 (41.0) | 2 (20.0) | 18 (36.7) | 18 (36.0) | 3 (10.0) | 10 (47.6) | 31 (30.7) | 49 (32.7) |
| Unassigned/Missing | 11 (28.2) | 4 (40.0) | 15 (30.6) | 11 (22.0) | 15 (50.0) | 6 (28.6) | 32 (31.7) | 47 (31.3) |
| Median SHIM (IQR) | 5 (1-12) | 15.5 (10-19) | 6.5 (1-14) | 11.5 (4.5-18.5) | 19 (14-24) | 18 (5-21) | 16 (7-21) | 13 (5-19) |
| Median AUA-SS (IQR) | 12 (6-17.5) | 5.5 (3-8) | 9.5 (3-15) | 9 (4-14) | 6.5 (2.5-11) | 10 (7-21) | 9 (4-13) | 9 (4-14) |
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree