Highlights
- •
We compared treatments in patients with cT1 renal masses undergoing immediate vs delayed intervention.
- •
Use of nephron sparing interventions were not compromised by a period of active surveillance.
- •
Surgical outcomes and perioperative morbidity were similar in patients undergoing immediate vs delayed intervention.
Abstract
Introduction and Objective
It remains unknown whether the use of nephron sparing intervention (NSI) is impacted with delayed intervention after a period of active surveillance (AS) compared with immediate intervention for patients with clinically localized renal masses ≤7cm (cT1RMs). We hypothesized that the proportion of patients undergoing NSI is similar among patients undergoing immediate and delayed intervention for cT1RMs.
Methods
We retrospective reviewed the prospectively maintained Michigan Urological Surgery Improvement Collaborative (MUSIC) registry for patients undergoing intervention for cT1RMs from 05/2017 to 09/2023. The primary outcome was type of treatment received: radical nephrectomy (RN) or NSI (partial nephrectomy, ablation, or stereotactic body radiation therapy). The main independent variable was timing of treatment: immediate (treatment within 90 days) vs. delayed intervention (>90 days). We fit a mixed-effects multivariable logistic regression model to assess for the adjusted association of immediate vs delayed intervention with the receipt of NSI and estimate an adjusted probability of NSI.
Results
We identified 2,156 patients, of whom 93% underwent immediate intervention and 7% underwent a period of AS prior to delayed intervention. Median time from initial visit to intervention was 1.4 (IQR 0.9–2.0) and 13 (IQR 7.7–21) months in the immediate vs delayed intervention groups, respectively. In the multivariable model, we did not appreciate a significant association between delayed intervention with receipt of NSI (OR 0.99, 95% CI 0.57–1.70, P >0.9). The adjusted proportion of NSI was 75% and 78% for patients in the immediate and delayed intervention cohorts, respectively.
Conclusion
Patients undergoing delayed intervention after AS had similar use of NSI compared with those undergoing immediate intervention. Active surveillance for patients with cT1RMs does not appear to compromise the ability to perform nephron sparing interventions.
1
Introduction
With the widespread use of cross-sectional abdominal imaging, the diagnosis of renal masses, in particular stage cT1 renal masses (cT1RM), has increased over the past few decades [ ]. Active surveillance (AS) with clinical and radiographic monitoring for patients with small RMs has gradually become an accepted management strategy, demonstrating excellent oncological safety and not compromising oncologic outcomes [ ].
Despite these encouraging data, approximately a third of patients with renal masses on AS receive delayed intervention, whether it is due to progression of the disease or anxiety from the possible diagnosis of renal cell carcinoma (RCC) [ ]. When feasible, NSIs are preferred over RN as they are associated with lower rates of surgically-induced chronic kidney disease (CKD), which is a risk factor for cardiovascular events [ , ]. Supporting the importance of nephron preservation, the proportion of patients undergoing PN, tumor ablation, and AS has steadily risen over the past decades; in fact, in a span of 10 years, the proportion of patients with cT1RM receiving RN has dropped over half, to around 20% of patients receiving definitive intervention [ ].
The Michigan Urologic Surgery Improvement Collaborative (MUSIC) is a community that partners to improve patients’ lives by inspiring high quality care through data-driven best practices, education, and innovation. MUSIC has prospectively maintained a registry of patients with localized renal masses ≤7cm in size since 2017, and has developed and implemented multiple quality improvement efforts aimed at encouraging the use of AS in appropriate patients [ ]. It remains unclear if the ability to perform NSI is negatively impacted for those undergoing delayed intervention after a period of AS. Herein, we examined the association of treatment timing (immediate intervention vs delayed intervention following AS) with the receipt of NSI for patients with cT1RM across the state of Michigan. Our hypothesis is that there will be no difference in the receipt of NSI among patients undergoing immediate vs delayed intervention for patients with cT1RMs.
2
Materials and methods
2.1
Study population
MUSIC-KIDNEY is a subset of the MUSIC collaborative, with over 100 providers from 20 practices contributing cases [ ]. Data abstractors reviewed the primary medical record and entered clinical, radiographic, treatment, and laboratory parameters at fix intervals into a web-based registry. We retrospectively reviewed all patients 18 years and older who underwent an intervention (radical nephrectomy (RN), partial nephrectomy (PN), tumor ablation (TA), or stereotactic body radiation therapy (SBRT)) for a cT1RM in MUSIC from 05/2017 to 09/2023. We defined NSI as any of the following: PN, TA, or SBRT. As the primary study objective was to assess the association of treatment delay while on AS with the use of NSI, patients were either classified as undergoing immediate intervention, defined as intervention within 90 days of the index encounter with their MUSIC urologist, or delayed intervention, defined as intervention after at least a 90-day period of active surveillance before transitioning to treatment. Patients that were listed as undergoing immediate intervention in the registry, but had surgery greater than 90 days after the index encounter were excluded from this analysis as they did not accurately reflect the clinical question of how active surveillance may influence future treatment decisions. AS for T1RM in the MUSIC KIDNEY registry was defined as the affirmative selection of active surveillance and the absence of treatment for at least 90 days.
Patients with radiographically benign lesions (Bosniak I, II, IIF cysts and angiomyolipomas) were excluded, such that only patients suspicious or indeterminate for RCC were included. Patients were also excluded if they had previous systemic therapy, nephroureterectomy, metastasis at the time of diagnosis, treatment of bilateral kidney masses, familial kidney cancer syndrome, kidney metastasis from another primary tumor, and/or solitary kidney, as these may influence the decision for RN vs NSI.
2.2
Study objectives
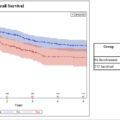
The primary objective was to test for the association of treatment type (RN vs. NSI) with timing of treatment (immediate vs. delayed intervention). The primary independent variable was timing of treatment and the main dependent variable was treatment type: RN vs. NSI. Secondary objectives were to assess for the association of treatment timing with measures of perioperative morbidity, oncological, and renal function outcomes. Perioperative and oncological outcomes were limited to patients undergoing surgery (open/robotic/laparoscopic RN/PN). Perioperative outcomes of interest included prolonged length of stay (LOS: defined as ≥3 days for laparoscopic/robotic surgery or ≥5 days for open surgery), estimated blood loss (EBL) >500 ml, warm ischemia time (WIT) >30 minutes, emergency room visit, and readmission. Oncologic outcomes of interest included surgical pathology (benign vs. malignant) and presence of positive surgical margin (PSM). Survival outcomes included metastasis-free survival, overall survival, and CKD stage G3b-free survival (eGFR <45 ml/min/1.73 m 2 ).
2.3
Statistical analysis
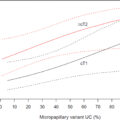
Patient clinical and demographic characteristics were summarized and compared between patients undergoing immediate vs. delayed intervention with the Chi-square test or Fisher’s exact test for categorical variables, and Wilcoxon rank sum test for continuous variables. For the primary objective, we fit a mixed-effects multivariable logistic regression model to assess for the adjusted association of immediate vs. delayed intervention with the receipt of NSI. A random intercept for surgeon nested within practice was included to account for intra-surgeon correlation. This model was then used to estimate the adjusted proportion of NSI among each group. The model was adjusted for age (continuous), body mass index (BMI, continuous per 5 unit change), sex (male/female), race (white /African American/other/unknown), family history of renal cancer (yes/no), Charlson Comorbidity Index (CCI, 0/1/≥2), preoperative glomerular filtration rate (GFR), insurance type (private/public/none or unknown), practice type (academic/hybrid/private), multiple lesions, radiographic tumor type (complex cyst/indeterminate/solid mass), tumor size (cm, per 0.5 cm change) and RENAL nephrometry score (low [4–6]/intermediate [7–9]/high complexity [10–12]). To test if the association of treatment timing (immediate vs. delayed intervention) and treatment type (RN vs. NSI) was different among patients with cT1a vs. cT1b renal masses, we fit a multivariable model with the same covariates described previously and included an interaction term between clinical stage and treatment timing.
For the secondary objectives, we compared the proportion of patients with the outcomes of interest stated above based on treatment timing and compared between groups with Chi-squared and Fisher’s exact tests. For all time to event analysis, the date of intervention was considered time zero. For overall survival, patients were censored at the date of their last follow-up, and for CKD stage G3b-free survival, patients were censored at their last GFR measurement. The Kaplan Meier estimator and log rank test was used to compare the time to event outcomes of overall survival (OS) and CKD stage G3b-free survival between immediate and delayed intervention cohorts. For time to the development of CKD stage G3b (eGFR <45), we included only patients with a baseline eGFR >45 prior to the date of intervention. Statistical analysis was performed with SAS v. 9.4 (SAS Institute Inc., Cary, NC, USA) with significance set at P <0.05. This study was deemed exempt from review by the Wayne State University IRB.
3
Results
A total of 2,156 patients with cT1RMs who underwent intervention were identified in the MUSIC-KIDNEY registry. 2,009 (93%) patients underwent immediate intervention, whereas 147 (7%) patients received delayed intervention. Patients in the immediate intervention group had a median time to treatment of 1.4 months (IQR0.9–2.0) compared with 13 months (IQR 7.7–21) for the patients in the delayed intervention group. The median follow up was 28 (0.9–50) and 32 (18–43) months for immediate and delayed intervention, respectively.
Baseline patient and tumor characteristics in both groups are displayed in Table 1 . Patients undergoing delayed intervention tended to be older (median: 67 vs. 62, P <0.001), had more comorbidities (CCI≥2 in 38% vs. 22%, P <0.001), and were more often treated in academic practices (31% vs. 25%, P = 0.048). Masses in the delayed intervention group were slightly smaller at diagnosis (median: 2.5 cm vs. 3.3 cm, <0.001). Among patients in the delayed intervention group, there was mild interval growth of lesions while on AS – the median renal mass diameter was 2.5cm (IQR:1.6–3.3 cm) at diagnosis and 2.8 cm (IQR: 2.0–3.5 cm) at the time of treatment. The median renal mass growth rate for the delayed intervention cohort was 0.34 cm/year (IQR: 0–0.73 cm/year).
| Variable | Immediate | Delayed | P-Value |
|---|---|---|---|
| No. of patients | 2009 | 147 | |
| Age, years (median, IQR) | 62 (53–70) | 67 (59–74) | <0.001 |
| BMI, units (median, IQR) | 30 (27–35) | 30 (27–33) | 0.8 |
| Female, n (%) | 768 (38%) | 59 (40%) | 0.6 |
| Race, n (%) | 0.053 | ||
| White | 1583 (79%) | 115 (78%) | |
| African American | 199 (9.9%) | 21 (14%) | |
| Asian | 21 (1.1%) | 2 (1.4%) | |
| Other | 40 (2.0%) | 3 (2.0%) | |
| Unknown | 155 (7.7%) | 4 (2.7%) | |
| Charlson Comorbidity Index | <0.001 | ||
| 0 | 1165 (58%) | 66 (45%) | |
| 1 | 374 (19%) | 25 (17%) | |
| ≥ 2 | 469 (23%) | 56 (38%) | |
| Family History of RCC, n (%) | 84 (5.4%) | 7 (6.0%) | 0.8 |
| Preoperative GFR, ml/min 1.73 m 2 (median, IQR) | 80 (64–94) | 78 (61–95) | 0.4 |
| Insurance | 0.5 | ||
| Private | 1171 (58%) | 82 (56%) | |
| Public | 816 (41%) | 62 (42%) | |
| None/Unknown | 22 (1.1%) | 3 (2.0%) | |
| Practice Type | 0.048 | ||
| Academic | 512 (25%) | 45 (31%) | |
| Hybrid | 1341 (67%) | 98 (67%) | |
| Private/Community | 156 (7.8%) | 4 (2.7%) | |
| Multiple Lesions, n (%) | 214 (11%) | 16 (11%) | 0.9 |
| Tumor Type | 0.002 | ||
| Complex Cyst | 91 (4.5%) | 16 (11%) | |
| Indeterminate | 163 (8.1%) | 13 (8.8%) | |
| Solid | 1755 (87%) | 118 (80%) | |
| Tumor Size at diagnosis, cm (median, IQR) | 3.3 (2.4–4.6) | 2.5 (1.7–3.3) | <0.001 |
| Tumor Size at treatment, cm (median, IQR) | 3.3 (2.4–4.6) | 2.8 (2.0–3.5) | <0.001 |
| Clinical T stage at diagnosis, n (%) | <0.001 | ||
| cT1a | 1315 (65%) | 126 (86%) | |
| cT1b | 694 (35%) | 21 (14%) | |
| Clinical T stage at treatment, n (%) | <0.001 | ||
| cT1a | 1310 (65%) | 120 (82%) | |
| cT1b | 699 (35%) | 27 (18%) | |
| RENAL Score, n (%) | 0.7 | ||
| Low (4–6) | 384 (19%) | 25 (17%) | |
| Intermediate (7–9) | 515 (26%) | 28 (19%) | |
| High (10–12) | 185 (9.2%) | 11 (7.5%) | |
| Unknown | 925 (46%) | 83 (56%) | |
| Renal Mass Biopsy (RMB) Performed | 417 (21%) | 31 (21%) | 0.92 |
| Biopsy Pathology | <0.001 | ||
| Benign/Favor Benign | 20 (1.0%) | 8 (5.4%) | |
| Favor Malignancy/Malignant | 385 (19%) | 21 (14%) | |
| Indeterminant | 12 (0.60%) | 2 (1.4%) | |
| Biopsy not performed | 1592 (79%) | 116 (79%) |
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree