Highlights
- •
pTA-treated mRCC patients were compared to patients who underwent NLT and CN.
- •
pTA was associated with significantly lower mortality compared to NLT.
- •
OM between pTA and CN mRCC patients did not exhibit significant differences.
- •
pTA may provide a comparable survival benefit to CN in highly selected mRCC patients.
Abstract
Background
The role of primary tumor ablation (pTA) in metastatic renal cell carcinoma (mRCC) is unknown. We compared pTA-treated mRCC patients to patients who underwent no local treatment (NLT), as well as patients who underwent cytoreductive nephrectomy (CN).
Methods
Within the Surveillance, Epidemiology, and End Results database (SEER, 2004–2020), we identified mRCC patients who underwent either pTA, NLT or CN. Endpoints consisted of overall survival (OM) and other-cause mortality (OCM). Propensity score 1:1 matching (PSM), multivariable cox regression models (OM), as well as, multivariable competing risk regressions (CRR) models (OCM) were used.
Results
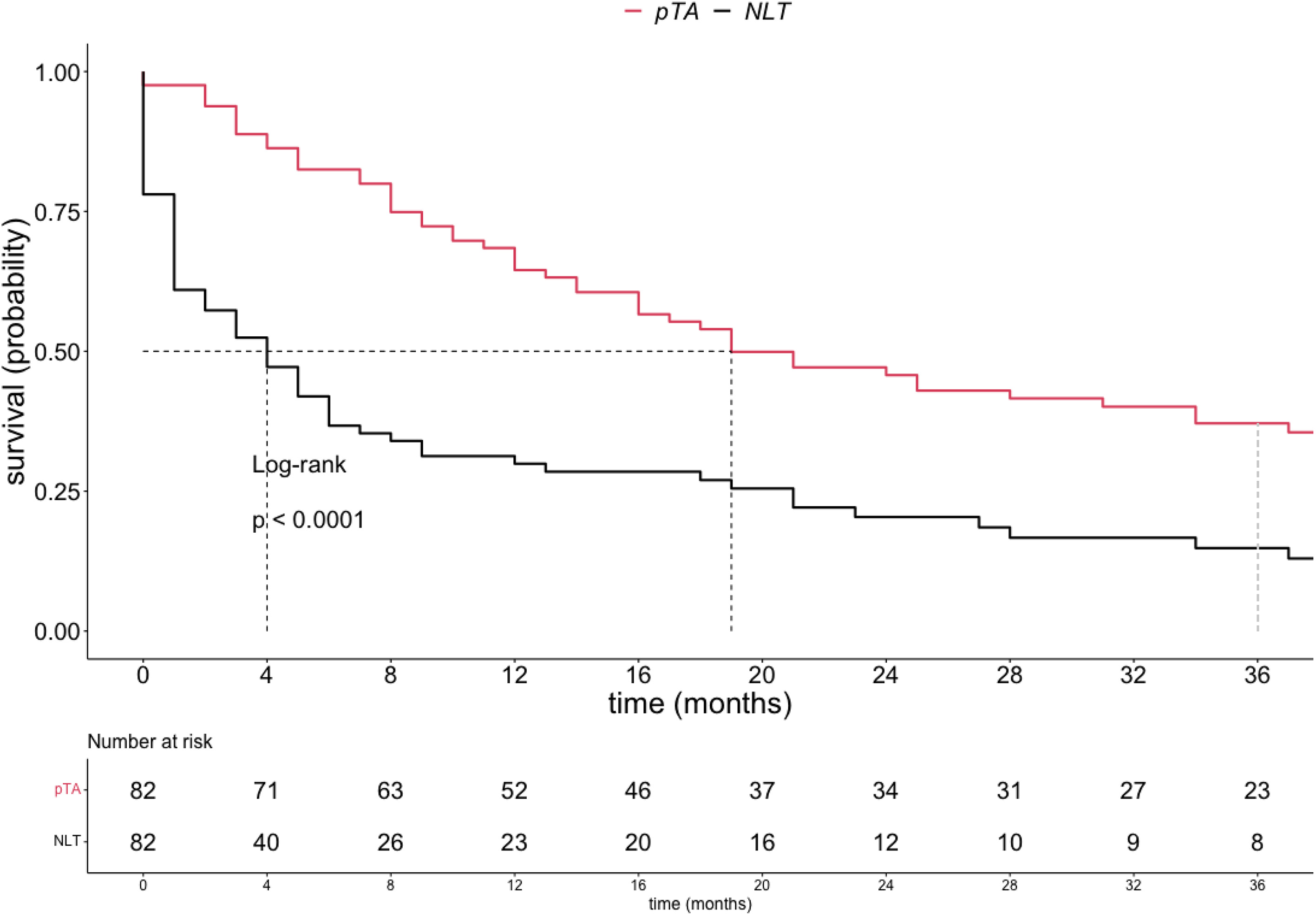
We identified 27,087 mRCC patients, of whom 82 (0.3%) underwent pTA, 17,266 (64%) NLT and 9,739 (36%) CN. In comparisons of pTA vs. NLT mRCC patients addressing OM, after 1:1 PSM, median survival was 19 months for pTA vs. 4 months for NLT patients (multivariable HR 0.3, 95% CI 0.22–0.47, P < 0.001). No statistically significant OCM differences were recorded in multivariable CRR (HR 1.13 95%, CI 0.52–2.44, P = 0.8). In comparisons of pTA vs. CN, after 1:1 PSM, no statistically significant differences in OM (HR 1.22, 95% CI 0.81–1.83, P = 0.32), as well as OCM (HR 1.4, 95% CI 0.56–3.48, P = 0.5) were recorded.
Conclusion
In mRCC patients, pTA is associated with significantly lower mortality compared to NLT. Interestingly, OM rates between pTA and CN mRCC patients do not exhibit statistically significant differences. This preliminary report may suggest that pTA may provide a comparable survival benefit to CN in highly selected mRCC patients.
1
Introduction
In the context of localized renal cell carcinoma, primary tumor ablation (pTA) has demonstrated comparable outcomes to surgical resection [ ]. As a result, pTA is currently recommended as an alternative treatment approach in patients with small renal masses [ , ]. In the metastatic setting, cytoreductive nephrectomy (CN) represents the gold standard in patients with favorable prognosis [ ]. However, there is a lack of viable alternatives for patients who are deemed unfit for surgery. The use of minimally invasive techniques in the treatment of metastatic cancer is gaining attention, offering potential alternatives where traditional surgical options may not be feasible [ ]. To date, primary tumor ablation (pTA) has only received limited attention as an alternative treatment modality in metastatic renal cell carcinoma (mRCC). To the best of our knowledge, only 3 studies have addressed pTA in the context of mRCC so far [ ]. The complexity of treating metastatic disease, where systemic therapy is often prioritized, as well as the lack of robust clinical data supporting its efficacy in this setting, have likely contributed to the limited exploration of pTA as a viable option in mRCC treatment. In consequence, the effect of primary tumor ablation (pTA) on overall survival (OS) in metastatic renal cell carcinoma (mRCC) is unknown. We postulated, that pTA may be associated with a benefit in overall survival compared to no local treatment (NLT). Moreover, we also hypothesized, that pTA may exhibit a comparable association with mortality relative to cytoreductive nephrectomy (CN). We tested both hypotheses within the Surveillance, Epidemiology, and End Results (SEER) database (2004–2020).
2
Methods
2.1
Study population
Within the SEER database (2004–2020), we identified patients ≥ 18 years old, with histologically confirmed metastatic RCC (International Classification of Disease for Oncology site code C64.9) [ ]. Autopsy or death certificate only cases were excluded, in order to avoid underestimation of survival [ ]. Primary tumor ablation was defined as either cryoablation (codes 13 and 23) or heat-based thermal ablation (code 15), in accordance with established methodology [ , ]. Death was defined according to the SEER mortality code as overall mortality (OM) [ ]. Additionally, other-cause mortality status (OCM; death unrelated to mRCC) was also recorded for each patient [ ]. Owing to the anonymously coded design of the SEER database, study-specific ethics approval was waived by the institutional review board [ ].
2.2
Variables of interest
Demographic covariates consisted of age at diagnosis (years, continuously coded) and sex. Tumor characteristics consisted of primary tumor size (<3.0 cm vs. ≥3.0 cm & <6.0 cm vs. ≥6.0cm vs. unknown), primary tumor extent (organ-confined vs. non-organ-confined vs. unknown), N-stage (N0 vs. N1 vs. NX), histological subtype (clear-cell vs. others) and systemic therapy (received vs. not received) [ ].
2.3
Statistical analyses
First, baseline characteristics of the cohort were analyzed. Descriptive statistics included frequencies and proportions for categorical variables. Medians and interquartile ranges (IQR) were reported for continuously coded variables. Second, to optimize the comparisons between pTA vs. NLT patients, as well as pTA vs. CN patients, we relied on 1:1 propensity-score matching (PSM), according to the nearest neighbor. Specifically, in comparisons between pTA vs. NLT, PSM was applied for age, sex, primary tumor size, primary tumor extent, histological subtype and systemic therapy exposure. In comparisons between pTA vs. CN, PSM was applied for age, sex, primary tumor size, N-stage, histological subtype and systemic therapy exposure. For all propensity-score matched variables, a threshold of <0.1 in standardized mean difference (SMD) was used. The latter is indicative of clinically insignificant differences [ ]. Third, Kaplan-Meier curves were used to depict OM between pTA and NLT patients, as well as pTA and CN patients. Additionally, multivariable Cox-regression models, adjusting for age, sex, primary tumor size, primary tumor extent, N-stage, histological subtype, systemic therapy exposure and year of diagnosis, were fitted to test for differences between pTA and NLT, as well as for differences in pTA and CN mRCC patients. Furthermore, we relied on cumulative incidence plots, as well as multivariable competing risks regression (CRR) models to test for differences in OCM between the groups [ ]. All tests were 2 sided, with a level of significance set at P < 0.05. R software environment for statistical computing and graphics (version 4.1.1; R Foundation for Statistical Computing, Vienna, Austria) was used for all analyses [ ].
3
Results
3.1
Overall population
The overall population consisted of 27,097 mRCC patients. Of those, 82 (0.3%) underwent pTA, 17,266 (64%) underwent no local treatment (NLT) and 9,739 (36%) underwent CN. Compared to the NLT and CN patients, pTA-treated patients were older (70 vs. 66 vs. 61 years), more often female (45 vs. 32 vs. 29%) and were less likely to undergo systemic therapy (21 vs. 39 vs. 44%). Differences in tumor characteristics existed for primary tumor size (≥ 6.0 cm: pTA 16% vs. NLT 56% vs. CN 79%), primary tumor extent (non-organ-confined: pTA 21% vs. NLT 34% vs. CN 75%), N-stage (N1: pTA 20% vs. NLT 32% vs. CN 40%) and histological subtype (clear-cell: pTA 44% vs. NLT 29% vs. CN 62%; Table 1 ).
| Characteristic | N | Overall, N = 27,087 a | pTA, N = 82 (0.3%) a | NLT, N = 17266 (64%) a | CN, N = 9739 (36%) a | p-value b |
|---|---|---|---|---|---|---|
| Age | 27,087 | 64 (57, 73) | 70 (60, 78) | 66 (58, 75) | 61 (54, 69) | <0.001 |
| Sex | 27,087 | <0.001 | ||||
| Female | 8,398 (31%) | 37 (45%) | 5,518 (32%) | 2,843 (29%) | ||
| Primary tumor size | 27,087 | |||||
| <3 | 1,144 (4.2%) | 26 (32%) | 827 (4.8%) | 291 (3.0%) | ||
| ≥3 & <6 | 4,461 (16%) | 35 (43%) | 3,025 (18%) | 1,401 (14%) | ||
| ≥6 | 17,317 (64%) | 13 (16%) | 9,633 (56%) | 7,671 (79%) | ||
| Unknown | 4,165 (15%) | 8 (9.8%) | 3,781 (22%) | 376 (3.9%) | ||
| Primary tumor extent | 27,087 | <0.001 | ||||
| T1-T2 | 8,303 (31%) | 53 (65%) | 6,221 (36%) | 2,029 (21%) | ||
| T3-T4 | 13,159 (49%) | 17 (21%) | 5,873 (34%) | 7,269 (75%) | ||
| TX | 5,625 (21%) | 12 (15%) | 5,172 (30%) | 441 (4.5%) | ||
| Histological subtype | 27,087 | <0.001 | ||||
| clear-cell | 11,043 (41%) | 36 (44%) | 4,929 (29%) | 6,078 (62%) | ||
| other | 16,044 (59%) | 46 (56%) | 12,337 (71%) | 3,661 (38%) | ||
| N- stage | 27,087 | <0.001 | ||||
| N0 | 15,114 (56%) | 57 (70%) | 9,585 (56%) | 5,472 (56%) | ||
| N1 | 9,349 (35%) | 16 (20%) | 5,439 (32%) | 3,894 (40%) | ||
| NX | 2,624 (9.7%) | 9 (11%) | 2,242 (13%) | 373 (3.8%) | ||
| Systemic therapy | 27,087 | <0.001 | ||||
| received | 11,120 (41%) | 17 (21%) | 6,772 (39%) | 4,331 (44%) |
3.2
Primary tumor ablation vs. no local treatment
After 1:1 PSM, 82 pTA vs. 82 NLT mRCC patients remained. Based on SMD criteria of <0.1, no clinically meaningful differences remained between pTA and NLT patients after PSM.
3.2.1
Overall mortality
In Kaplan-Meier analyses, median survival in pTA patients was 19 months vs. 4 months in NLT patients (hazard ratio [HR] 0.39, P < 0.0001; Fig. 1 ). In multivariable Cox regression analyses, pTA independently predicted lower OM (HR 0.32, P < 0.001; Table 3 ).