The prevalence and impact of incontinence
Up to 1 in 5 women and around 1 in 10 men over the age of 65 suffer from incontinence. The prevalence increases with increasing age and co-morbidity. Two-thirds of care home residents are incontinent of urine. However, with variations in definitions and under-reporting due to embarrassment, the prevalence of incontinence is probably an underestimate.
Incontinence can significantly affect a person’s wellbeing. People with incontinence restrict their social activities. Carer strain is common and incontinence is second only to dementia as an initiating factor in admission to a care home. Soiled clothing, bed linen and soft furnishings have to be laundered and replaced frequently, resulting in an increased financial burden. Incontinence overall costs the NHS over £ 420 million per year (approximately 1% of the total NHS budget).
Box 9.1 Changes in the urinary tract with ageing
- Shortening of the urethra
- Post-menopausal atrophy of the urothelium
- Reduced bladder sensation
- Reduced detrusor muscle function
- Increased residual bladder volume
- Less effective urethral closure
Box 9.2 Drugs that can worsen or precipitate incontinence
- Diuretics
- Sedatives
- Alpha blockers
- Any drug with cholinergic properties
Co-morbidities and incontinence
Diseases that are prevalent in older age can affect continence. Any disability affecting vision, mobility, dexterity or cognition may have an adverse effect on continence, especially if an individual has a problem with urgency of micturition.
Treatments for diseases may also have the unintended effect of precipitating incontinence. Some examples are given in Box 9.2. Patients with dementia may have incontinence because of either the disease process itself or its treatment, for example with cholinergic drugs, which can worsen an overactive bladder.
Patients with poorly controlled diabetes may have polyuria. Less commonly, patients with hypercalcaemia, hypokalaemia or diseases of the pituitary gland may present with urinary frequency or incontinence. There is also an association between incontinence and falls.
Assessment
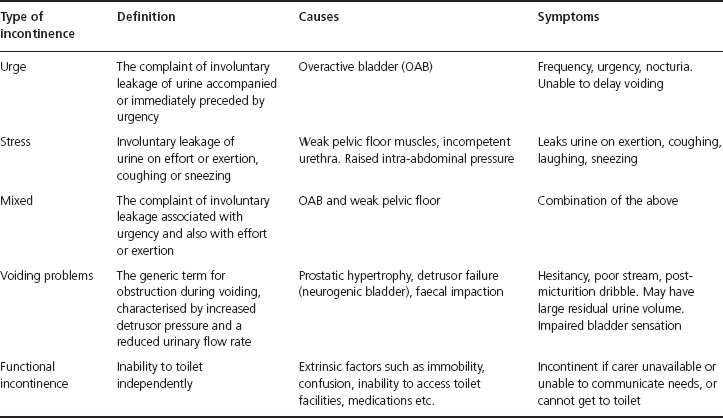
There are different types of urinary incontinence and symptoms vary in nature and severity (see Table 9.1). Each type is treated differently, so it is important to assess which type of incontinence a person has. This is based on the history and examination – urodynamics (specialised tests) are rarely needed.
Table 9.1 Types of urinary incontinence in older people.
Box 9.3 Key components of a continence assessment
- History of onset and duration of problems
- Symptom sorter (see Box 9.4)
- Previous medical, surgical and obstetric history
- Medications
- Assessment of functional abilities
- Examination of the abdomen, rectum (and perineum/vagina in women)
- Urinalysis
- Urea and electrolytes, glucose, calcium (and prostate-specific antigen in men)
In addition, patients are asked to keep a ’bladder diary’. It is also very important to ask about bowel problems, as constipation leading to faecal loading can cause urinary problems.
In a continence clinic, further assessments are typically undertaken, which include:
- post-micturition bladder scan (to look for evidence of voiding problems)
- measurement of urine flow (using a special commode)
- quality of life score
- measurement of body mass index.
There are five main types of urinary incontinence in older people:
- urge incontinence (or over-active/unstable bladder)
- stress incontinence
- mixed incontinence (both urge and stress)
- voiding problems (due to obstruction or a neurogenic bladder)
- functional incontinence (due to an inability to get to the toilet, or confusion).
All older people presenting with urinary incontinence should be offered an assessment. Box 9.3 shows the key components of this. Any member of the healthcare team can initiate it and there are useful diagnostic tools available to facilitate this.
As well as the assessment outlined in Box 9.3, a simple ’symptom sorter’ is useful in determining the type of incontinence (Box 9.4). A bladder diary, detailing volumes of urine voided, wet episodes, type and amount of fluids taken is also useful – for example, caffeine and citrus drinks can exacerbate bladder instability. A physiotherapist or occupational therapist can help if patients have mobility problems or difficulty accessing toilet facilities in their own home.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree