Early-Stage Colorectal Cancer
Northwestern University Feinberg School of Medicine, Chicago, IL, USA
Multiple Choice and Discussion Questions
Stage II Colon Cancer
1. Which of the following tumor features would you consider for recurrence risk stratification of a patient with stage II colon cancer to determine potential benefit from adjuvant chemotherapy?
- Lymphatic or vascular invasion
- Deficient mismatch repair (dMMR)
- KRAS mutation status
- Oncotype DX
Stage II colon carcinoma is a biologically heterogeneous entity with a wide range of 5-year disease-free survival (DFS) between 45.7% and 66.7%. Treatment choices as per current National Comprehensive Cancer Network (NCCN) Clinical Practice Guidelines in Oncology for stage II colon cancer include enrollment on a clinical trial, observation, or systemic chemotherapy (5-fluorouracil–leucovorin (5FU–LV) or capecitabine with or without the addition of oxaliplatin (CapeOx)) depending on the risk stratification. Traditional risk factors for recurrence include poorly differentiated histology, T4 disease, lymphatic or vascular invasion, bowel obstruction, less than 12 nodes examined, perineural invasion, localized perforation, or close, indeterminate, or positive margins. While these clinicopathologic risk features offer some overall guidance, they are inadequate in terms of the biologic behavior and risk of recurrence for an individual. Microsatellite instability high (MSI-H) phenotype, defined as instability in two or more nucleotide markers within the five microsatellite loci or ≥30% if a larger panel is used, through either germline mutation or epigenetic silencing, has both predictive and prognostic implications for adjuvant therapy. A retrospective stratification analysis using mismatch repair (MMR) status of 1027 previously randomized patients with stage II and III colon adenocarcinoma to either 5FU with levamisole or leucovorin, or observation, was reported by Sargent et al. (2009, 2010). They showed that patients with defective mismatch repair (dMMR) have a 5-year DFS of 80% compared with 56% for those with proficient MMR or microsatellite stable (MSS) (HR: 0.51; 95% CI: 0.29–0.89; P = .009). In patients with stage II colon cancer with dMMR or MSI-H who were treated with adjuvant 5FU chemotherapy, there was a statistically decreased overall survival (OS) compared to the surgery alone arm (HR: 2.95; 95% CI: 1.02–8.54; P = .04). The stage III MSI-H patients did not appear to benefit from 5FU (DFS, HR: 1.01; 95% CI: 0.41–2.51; P = .98) and only the MSS stage III patients obtained any survival advantage from adjuvant 5FU (DFS, HR: 0.64; 95% CI: 0.48–0.84; P = .001).
Emerging tools include gene expression assays, such as Oncotype DX and ColoPrint. Oncotype DX includes seven recurrence risk genes and five reference genes, and it calculates a recurrence score (low, intermediate, or high) predictive of the risk of recurrence of stage II colon cancer at 3 years. Validation studies have shown significant correlation between the risk of recurrence and the recurrence score. ColoPrint probes 18 genes and results in a risk index score independent of the clinical risk factors and MSI status, similar to Oncotype Dx, but the recurrence score has been independently validated with significantly associated relapse-free and distant metastasis–free survival. These gene signatures serve as important prognostication tools, but do not yet predict response to adjuvant chemotherapy, thus limiting their use to determine the role of adjuvant therapy. Several other potential molecular markers such as oncogenic KRAS and BRAF mutations, loss of heterozygosity at chromosome 18q, overexpression and mutations of TP53, expression of thymidylate synthase, or DNA ploidy are being currently analyzed for their prognostic and predictive capability, with insufficient evidence to recommend routine clinical use at this time for stage II colon cancer patients.
2. Which of the following management options would you consider for a patient with R0 resected stage II or node-negative colon adenocarcinoma with high-risk features?
- 5FU or capecitabine alone
- 5FU–oxaliplatin or FOLFOX
- Capecitabine–oxaliplatin or CapeOx
- Observation
- All of the above
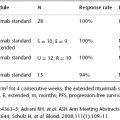
Although it is universally accepted that most stage III patients should receive adjuvant chemotherapy, there is uncertainty regarding whether stage II patients would derive sufficient benefit. The initial evidence to support the role of adjuvant chemotherapy came from the INT-0035 trial that randomized 325 patients with resected stage II colon cancer to either 5FU–levamisole for 1 year or observation. At a median follow-up of 7 years, 5FU–levamisole yielded a trend toward superior recurrence-free survival (HR: 0.69; 95% CI: 0.44–1.08; P = .10) over observation. However, there was no improvement noted in OS (72% in each arm; P = .83). The QUASAR trial also showed benefit in risk of recurrence at 2 years for 2146 patients with resected stage II colon cancer who were treated with 5FU–LV compared to patients who received no adjuvant therapy (HR: 0.71; 95% CI: 0.54–0.92; P = .01), with a trend toward better OS (HR: 0.86; 95% CI: 0.66–1.12). Furthermore, a large pooled analysis of seven randomized controlled trials (NCCTG, ECOG-NCCTG-INT, SWOG-INT0035, Siena, NCIC-CTG, FFCD, and GIVIO) with 1440 patients with node-negative disease revealed a 4% absolute benefit in 5-year DFS (76% versus 72%; P = .49), although there was no benefit in OS (81% versus 80%; P = .11). In contrast, the ACCENT data set, which included 6896 patients with resected stage II disease from 18 phase III adjuvant trials, showed an absolute benefit of 5% in 8-year OS (72.2% versus 66.8%; P = .026). Although probably real, the survival benefit from adjuvant chemotherapy for an average patient with stage II cancer is small and may not justify the involved cost, toxicity, and inconvenience to the patient.
This has prompted researchers to identify high-risk features within stage II disease (as listed in Question 1) that adversely affect the disease-specific survival and predict benefit from adjuvant chemotherapy. However, only a few adjuvant clinical trials have stratified patients according to these risk factors, and even those did not include all of them. A meta-analysis of four sequential NSABP clinical trials that compared adjuvant 5FU based chemotherapy with each other or no treatment showed that patients with Dukes’ B colon cancer (n = 1565) who had average-risk features (absence of obstruction, localized bowel perforation, or extension of tumor into adjacent organs) had a 32% reduction in mortality (HR: 0.68; 95% CI: 0.50–0.92; P = .01), whereas those with high-risk features had a 20% reduction of mortality (HR: 0.80; 95% CI: 0.55–1.17; P = .26). This translated into 5% absolute improvement in mortality in each category, thus counteracting the argument that only patients with high-risk features would derive benefit from adjuvant chemotherapy. An NCCTG trial restricted eligibility to high-risk stage II (T4 disease, and bowel perforation or obstruction) and stage III patients, and randomly assigned 317 patients to either adjuvant 5FU–LV chemotherapy or observation. Overall, there was a clear benefit in OS (74% vs. 63%; P = .01) in the chemotherapy arm, with only a trend toward benefit for patients with stage II cancer (n = 57) on exploratory analysis (90% vs. 74%; P = .15). Also, a large pooled analysis of seven randomized controlled trials with 1440 patients with node-negative disease failed to show benefit of chemotherapy in T4 low-grade (69% versus 71%) or high-grade (57% versus 46%) colon cancer compared to surgery alone in an underpowered subset analysis. Despite the lack of data from randomized clinical trials, the NCCN Clinical Practice Guidelines recommend discussion of adjuvant chemotherapy with medically fit patients with stage II disease with clinicopathologic high-risk features. Furthermore, MSI-low, defined as instability in less than two nucleotide markers within the five microsatellite loci, or MSS stage II colon cancer patients with a clinicopathologic risk factor would be considered potential candidates for 5FU-based chemotherapy after detailed discussion with patients; however, the management of the subset of patients with MSI-H tumors with traditional risk factor(s) is not clear, and they should be enrolled on a clinical trial or observed without adjuvant chemotherapy.
Furthermore, there are minimal data to recommend use of oxaliplatin with 5FU-based therapy in this patient population. The MOSAIC trial randomized 2246 patients, including 899 with stage II disease, to infusion–bolus 5FU–LV versus FOLFOX4, and found no improvement in 5-year DFS or 6-year OS between the two arms (OS 86.9% vs. 86.8%; HR: 1.00; 95% CI: 0.70–1.41; P = .986). However, a nonsignificant trend toward improved 5-year DFS in high- versus average-risk patients was observed with the addition of oxaliplatin (HR: 0.84; 95% CI: 0.50–1.02) in an unplanned analysis. Therefore, the addition of oxaliplatin is considered an appropriate option for stage II patients with high-risk features, but not for those with average-risk features. Patients should be encouraged to enroll in clinical trials as efforts continue to link risk with benefit from adjuvant therapy.
3. Why are patients with microsatellite instability (MSI) considered to have a better prognosis than those with microsatellite stable (MSS) tumors?
Patients with MSI-H tumors have a prognostic advantage regardless of the tumor stage at diagnosis. MSI phenotype has a higher prevalence in stage II than stage III colon cancers and has been associated with less lymph node involvement and metastasis. The precise explanation is not clear, but some of the pathologic differences include significant correlation of MSI tumors with intratumoral activated cytotoxic T-lymphocytes, increased apoptotic to proliferative index, and decreased p53 expression or KRAS mutations.
Stage III Colon Cancer
4. Which of the following adjuvant chemotherapy regimens would you not consider for a patient with R0 resected stage III or node-positive colon adenocarcinoma?