Introduction 173
Glycaemic control 174
Dyslipidaemia 177
Hypertension 183
Non-pharmacological means of reducing blood pressure 186
Pharmacological treatment of cardiovascular disease 187
Obesity 188
Conclusion 189
References 189
Diabetes is now one of the most common non-communicable diseases and poses one of the most challenging health problems worldwide. Modernisation and Westernisation of lifestyles are the underlying cultural processes driving the escalating diabetes epidemic. In 2000 the estimated worldwide prevalence of type 2 diabetes was 151 million adults, compared to 135 million in 1995 and 30 million in 1985 (Harris et al 1998). It is estimated that this prevalence will increase to 300 million people worldwide in 2025, with the steepest increases in rates of diabetes being in developing countries due to their rapidly changing economies and lifestyles (King et al 1998).
The burden of macrovascular disease in people with diabetes has been recognised for many years. It is well established that people with type 1 and type 2 diabetes have an increased risk of atherosclerotic cardiovascular disease (CVD). People with diabetes have a higher incidence of morbidity and mortality from coronary heart disease (CHD), and there is also evidence suggesting an increased risk of stroke and peripheral vascular disease in these people.
Epidemiological studies from around the world have confirmed the excessive cardiovascular morbidity and mortality in people with diabetes compared to non-diabetic subjects in the same geographical area over the same time period. Data from the Framingham cohort, in the USA (Kannel & McGee 1979), which first examined this issue, demonstrated an increase in CVD in people with diabetes compared to people who did not have diabetes in the study population. There were higher rates of CHD, congestive cardiac failure, stroke, peripheral vascular disease and cardiovascular death within the subgroup of people with diabetes. Although this group was small, and there might have been discrepancies in the diagnostic criteria for diabetes, several other larger studies have mirrored these findings.
Another study from the USA (Wingard et al 1993) demonstrated the increased prevalence of coronary heart disease in different age groups. The rate of CHD was increased 14-fold in the 18–44-years age group, threefold in the 45–64-years age group and doubled in those people over the age of 65 years. Two further studies have also shown that whereas the absolute rates of CVD are higher in men with diabetes, the relative risk of CVD is higher in women with diabetes (Jousilahti et al 1999, Manson et al 1990), so it is sometimes stated that ‘women with diabetes lose the protection of their gender’.
The age-adjusted mortality has also been shown to be greater in diabetic populations. A meta-analysis of ten observational studies (Lee et al 2000) revealed a relative risk of death of 1.9 for men and 2.6 for women, when compared with their non-diabetic counterparts.
The South Tees Mortality Study (Roper et al 2002) looked at death rates in a cohort of 4842 people with type 2 diabetes and found that one-quarter was dead within 6 years, the majority from cardiovascular causes. Cardiovascular mortality was significantly increased in both sexes and all age groups, but it was particularly evident in middle-aged women with diabetes. Relative death rates for age band 40 to 59 years were 5.47 and 5.60 for men and women, respectively.
Despite the accumulation of this evidence over the past three decades, reducing the risk of cardiovascular disease in the person with diabetes remains a major challenge. This chapter examines a multifactorial approach to reducing cardiovascular morbidity and mortality in the person with diabetes and includes detailed examination of several recent studies that have helped provide evidence for this approach.
GLYCAEMIC CONTROL
Controversy remains regarding the extent to which hyperglycaemia contributes to the high prevalence of CVD in people with type 1 and type 2 diabetes and there is relatively little convincing evidence to suggest that aggressively managing hyperglycaemia reduces cardiovascular risk in people with diabetes mellitus. One study in 1971 even suggested that, far from being protective, lowering plasma glucose using the sulphonylurea, tolbutamide, had toxic effects on the myocardium (University Group Diabetes Program 1970). Although this study has subsequently been criticised for poor study design and the results of other studies have contradicted this evidence, other controversial issues arose in this field in the 1980s. The association between elevated plasma insulin levels and coronary heart disease in insulin-resistant people, for example, led some investigators to suggest that insulin itself might be atherogenic, given that insulin stimulates both smooth muscle proliferation and lipid synthesis. Over the past decade, however, more evidence has been published that has further increased our understanding about the relationship between CVD and glycaemic control.
UNITED KINGDOM PROSPECTIVE DIABETES STUDY
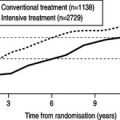
The long-awaited results from the United Kingdom Prospective Diabetes Study (UKPDS) were published in 1998 (UKPDS Study Group 1998a, 1998b, 1998c, 1998d). This randomised, controlled trial of people newly diagnosed with type 2 diabetes refuted the suggestion that treatment with either sulphonylureas or insulin therapy was associated with increased cardiovascular risk (UKPDS Study Group 1998a). Subjects in the main study were randomised either to conventional treatment with diet or to intensive treatment with either sulphonylurea or insulin therapy. There was a significant reduction in HbA1c in the intensive treatment group and a 25% risk reduction in microvascular endpoints (neuropathy, nephropathy and retinopathy and need for laser treatment). However, despite small reductions in macrovascular endpoints, such as myocardial infarction (MI), these results did not reach statistical significance. These people have been followed for a few years since the end of the UKPDS and the reduction in MI with intensive treatment based on sulphonylureas or insulin therapy is now statistically significant.
Interestingly, a substudy from the UKPDS group in overweight individuals indicated that treatment with metformin led to a reduction in cardiovascular events, including MIs and diabetes-related deaths (UKPDS Study Group 1998b). Because MI was such a common cause of death in these individuals, the reduction in MIs was also mirrored by a reduction in total mortality. This unexpected finding was not fully anticipated by the UKPDS investigators and the results remain difficult to explain. The number of people receiving metformin was small (n = 342) and this might have exaggerated the degree of benefit. The reductions in events could not be explained on the basis of reductions in HbA1c, suggesting that metformin might have extended benefits that were not directly related to glucose-lowering effects of the drug. Metformin has a relatively minor effect in reducing insulin resistance at the level of the liver, and this is one possible explanation.
DIABETES CONTROL AND COMPLICATIONS TRIAL
The results of the Diabetes Control and Complications Trial (DCCT), a multicentre trial, which randomised 1141 people with type 1 diabetes to usual care or intensive insulin therapy, mirrored to some extent the findings from the UKPDS Study. There was a significant reduction in microvascular endpoints in the intensive treatment group compared to the conventionally treated group (DCCT Research Group 1995). Although there was a trend towards a reduction in cardiovascular disease in the intensive treated group, again this did not reach statistical significance. This might be due to the small number of events that actually occurred throughout the period of follow-up (40 in the control group; 23 in the treatment group), which is attributable to the young age of the population studied (13–39 years). A subsequent meta-analysis, including data from DCCT and several smaller studies, demonstrated a significant reduction in the number of macrovascular events, but no significant effect on the number of people developing macrovascular disease, or on macrovascular mortality (Lawson et al 1999).
Therefore, although the results from the UKPDS and DCCT trials were beneficial in so much as they proved that treatment with insulin or sulphonylureas reduced microvascular events and did not lead to an increase in cardiovascular disease, to date, no study has demonstrated that intensive management of hyperglycaemia reduces the risk of CHD. However, in addition to the evidence that metformin might reduce the incidence of macrovascular complications, the thiazolidinediones, a new group of oral agents, have also been shown to have extended benefits beyond glucose lowering, including favourable affects on blood pressure, lipids and microalbuminuria, as well as reductions in novel cardiovascular risk markers such as C-reactive protein (CRP) (Haffner et al 2002). Whether this translates into clinical benefit in terms of a reduction in cardiovascular events is currently being tested in large studies with rosiglitazone and pioglitazone, respectively.
Based on the results of the UKPDS, Alan should initially be treated with lifestyle measures. If, as is likely, he is unable to reach the target HbA1c with lifestyle measures alone, then metformin would be the drug of first choice. It would be helpful, however, to have an echocardiogram to be certain that he does not have cardiac failure, as this would be a contraindication to the use of metformin. An echocardiogram would also establish the best secondary preventive therapies. If significant left ventricular dysfunction is present, a thiazolidinedione is also contraindicated because of the side effect of fluid retention, so a sulphonylurea would be indicated.
DYSLIPIDAEMIA
Hyperlipidaemia is also a risk factor for atherosclerotic cardiovascular disease. In the general population, the Multiple Risk Factor Intervention Trial (MRFIT) demonstrated that the incidence of ischaemic events increases proportionally with elevations in serum low-density lipoprotein (LDL) cholesterol, and conversely with reductions in serum high-density lipoprotein (HDL) cholesterol concentrations (Stamler et al 1993). This study also showed that the absolute increase in risk of a cardiovascular event per unit rise in serum cholesterol was steeper in people with diabetes than in those without.
Well-controlled type 1 diabetes is associated with serum lipids similar to that of the general population. Poor glycaemic control, increasing age, obesity and the presence of nephropathy all lead to an increase in serum triglyceride and very low-density lipoprotein (VLDL) concentrations in type 1 diabetes. Type 2 diabetes is also associated with an unfavourable lipid profile; although the level of total and LDL cholesterol might be within normal limits, the HDL concentration tends to be low with elevated triglycerides. In addition, the distribution of LDL subfractions is altered so that small, dense LDL particles predominate and these are thought to be more atherogenic. This pattern of dyslipidaemia is also seen in those people without frank diabetes who have the ‘metabolic syndrome’ and who also have an increased risk of cardiovascular disease (see Chapter 4).
It is interesting to remember that as recently as 10 years ago lipid-lowering agents were thought to have few beneficial effects on cardiovascular mortality in the general population and the data from one meta-analysis even suggested that there was an increased risk of suicide and accidental death in people who were receiving lipid-lowering agents (Davey Smith & Pekkanen 1992). The advent of the HMG CoA reductase inhibitors (statins) revolutionised lipid-lowering therapy and the evidence that has emerged over the past decade for reducing serum total and LDL cholesterol is compelling and has dramatically changed clinical practice. This has included subgroup analysis of large studies containing many people with diabetes and, more recently, studies performed exclusively in people with diabetes.
Three major studies published in the 1990s, in which more than 15 000 people participated, looked at the issue of secondary prevention of atherosclerotic CVD using statin therapy: the Scandinavian Simvastatin Survival Study (4S) (Scandinavian Simvastatin Survival Study Group 1994), the Cholesterol and Recurrent Events (CARE) Trial (Sacks et al 1996) and the Long-term Intervention with Pravastatin in Ischaemic Disease (LIPID) Study (LIPID Study Group 1998).
Data from the 4S and CARE, which were conducted in the US and Canada, and from the LIPID Study, which was carried out in Australia and New Zealand, were consistent. Reducing LDL and total cholesterol is associated with reductions in all-cause mortality, CHD-related deaths and major coronary events (first MI, unstable angina). As a result, statin therapy in people with a history of coronary heart disease is normal practice.
PRIMARY PREVENTION STUDIES
Also in the 1990s, two large studies also examined the issue of the role of statins in the primary prevention of coronary heart disease. Data from the West of Scotland Coronary Prevention Study (WOSCOPS) and the Airforce/Texas Coronary Atherosclerosis Prevention Study (AFCAPS/TexCAPS) suggested that statin therapy was also of benefit in people with no history of CVD (Shepherd et al 1995, Downs et al 1998). People with a wide range of cardiovascular risk were included in these studies and all people appeared to benefit. Few people with diabetes were included in these studies so no meaningful analysis could be made of the data from these small subgroups.
However, despite the large numbers of people in these five studies, relatively few individuals with diabetes were included. A total of 2000 people with diabetes were included in these five cohorts and, until recently, clinical practice was based on data from these small diabetic subgroups. Over the last few years, however, further studies have been published that have greatly enhanced our knowledge of the effects of lipid-lowering in the population of people with diabetes.
The Heart Protection Study
The Heart Protection Study (HPS) was a large randomised study designed to address the question of whether lowering LDL cholesterol below previously accepted thresholds in people at high risk of cardiovascular disease would confer added benefit (Heart Protection Society Collaborative Group 2002). In particular, its aim was to study the effects of lipid lowering within subgroups for which there was limited existing evidence including people with diabetes, women, the elderly and those with non-coronary occlusive arterial disease.
There were 5963 people with diabetes within the study group and 90% of these were classified as having type 2 diabetes. There were highly significant reductions in serum total LDL cholesterol concentrations and a corresponding 22% reduction in first major vascular event in the simvastatin-treated group when compared to the placebo group. These figures are similar to the reductions seen with simvastatin in the non-diabetic, high-risk people studied.
An even greater reduction was seen in the group with diabetes but without previous coronary or occlusive vascular disease. A total of 2912 diabetic people had no cardiovascular disease and simvastatin reduced the primary endpoint of first major vascular event from 13.5% to 9.3%, and of first major coronary event from 6.5% to 3.7%. This effect was still seen regardless of age, sex, blood pressure, body mass index (BMI), HBA1c and, most importantly, initial LDL cholesterol, with similar levels of relative risk reduction in those with high serum cholesterol levels compared to those individuals with ‘normal’ cholesterol levels (Collins et al 2003).
ALLHAT-LLA and ASCOT-LLA
The Antihypertensive and Lipid-Lowering treatment to prevent Heart Attack Trial–Lipid Lowering Arm (ALLHAT-LLA) was a non-blinded, randomised study with one arm examining the benefits of cholesterol lowering with 40 mg of pravastatin in modestly hypertensive people with one or more coronary heart disease risk factors. The other arm of the study compared the effects of two different antihypertensive regimes (The ALLHAT Officers and Coordinators for the ALLHAT Collaborative Research Group 2002a).
In this trial, the primary endpoint of all-cause mortality was not altered significantly by treatment with pravastatin, unlike other primary prevention trials. There was a non-statistically significant reduction in rates of CHD and stroke. These rather disappointing results were thought to be due to a lower than average compliance rate in the treatment group (70–75%) and high use of open-label statins in the placebo group, leading to a smaller reduction in both total and LDL cholesterol than observed in the other large intervention trials. In total, 3638 people with type 2 diabetes took part in the study (35% of the cohort) and there were no differences in the rates of the primary or secondary endpoints in this subgroup.
Published shortly after ALLHAT in 2003, the Anglo-Scandinavian Cardiac Outcomes Trial – Lipid Lowering Arm (ASCOT-LLA) was a similarly designed study, again with one arm, looking at cholesterol lowering, this time with 10 mg of atorvastatin in people with hypertension and who were at high risk, but had no previous history of CHD (Sever et al 2003). The results of this study revealed a 36% reduction in non-fatal MI and fatal CHD in the active treatment group. However, treatment with atorvastatin in the subgroup with diabetes (25% of the total cohort) did not lead to a statistically significant reduction in primary endpoint. This might have been due to the higher use of open-label statins within the placebo group with diabetes than among the group who did not have diabetes.
Collaborative Atorvastatin Diabetes Study (CARDS)
Until very recently, no study had shown the benefits of cholesterol lowering in a cohort containing only individuals with diabetes. This evidence has now been provided by the Collaborative Atorvastatin Diabetes Study (CARDS), a multicentre, double-blind trial that examined the effects of cholesterol lowering in 2838 people with type 2 diabetes and low LDL-cholesterol (median 3.1 mmol/L) randomised to atorvastatin 10 mg/day or placebo (Colhoun et al 2004).
CARDS also reinforces the long-term safety profile of statins. The study showed no significant differences in treatment-related events or liver enzyme abnormalities and no cases of muscle symptoms or rhabdomyolysis. Discontinuation rates associated with treatment-related events were low in both groups.
SHOULD EVERYONE WITH DIABETES RECEIVE A STATIN?
These more recent studies add weight to the argument for treating people with diabetes with statins to reduce cardiovascular risk. Before the availability of these data, it was necessary to extrapolate data from the older studies to the population of people with diabetes in order that they could enjoy the benefits of lipid-lowering therapy. However, the issue of whether or not all people with diabetes should receive statin therapy remains controversial.
Some believe that everyone with type 2 diabetes should be treated as if they had pre-existing CHD, and one large study based on data from Finland suggested that a person with diabetes was at greater risk of suffering from a coronary event than a person without diabetes who has previously had a similar event (Haffner et al 1998). A similar study carried out in Tayside, however, has suggested that, while certainly at higher risk of CHD than the general population, people with diabetes without known cardiovascular disease are not more likely to suffer an event than a person who has pre-existing cardiovascular disease (Evans et al 2002). Several recent guidelines suggest that all people with diabetes are treated as a CHD equivalent, and so should be given a statin. Although all people with diabetes would gain from the widespread use of statins, the issues of cost and compliance need to be considered carefully before adopting such a ‘blanket’ prescribing policy.
A further issue that remains unresolved is the use of statins in people with type 1 diabetes. This group has a much higher incidence of CHD than their counterparts who do not have diabetes. Despite this, however, diabetes is usually diagnosed at a young age when the absolute incidence of CHD is negligible. The benefit of statin therapy in type 1 diabetes has not been proven given the very small numbers of these people included in statin trials. The timing of initiation of therapy also remains unresolved in people with type 1 diabetes, and there is still a need for further information regarding the benefits of statins in people with diabetes but who do not have CHD, particularly people with type 1 diabetes and younger people with type 2 diabetes.
A further cloudy issue in the management of dyslipidaemia is how far cholesterol should be lowered. Although the Heart Protection Study provided some indication as to target levels of cholesterol it was not specifically designed to identify this. A recent novel analysis of the reduction of CHD events with all forms of lipid-lowering therapy (Brady & Betteridge 2003) has shown that the lower the cholesterol the greater the reduction in CHD events, and the same is true for an analysis of the reduction of CHD events in people with diabetes. The Pravastatin or Atorvastatin Evaluation and Infection Therapy (PROVE-IT) Study (Cannon et al 2004) has demonstrated that high-dose atorvastatin is better than a less efficacious dose of pravastatin in reducing major cardiovascular events or death in patients with acute coronary syndromes; 18% of the cohort had diabetes but the reduction in diabetic subjects did not reach statistical significance.
OTHER DRUGS
Fibrates are also available as lipid-lowering therapy. They cause a reduction in serum triglycerides and elevations in HDL cholesterol with little impact on LDL cholesterol. Given that the major lipid abnormalities seen in people with diabetes are a reduction in HDL cholesterol and elevated serum triglycerides, it would seem likely that fibrates would be a more reasonable choice of lipid-lowering therapy in the person with diabetes. A randomised double-blind placebo-controlled trial has studied the effect of fibrates on progression of coronary artery disease in people with type 2 diabetes (Diabetes Atherosclerosis Intervention Study Investigators 2001) and demonstrated a 28% reduction in triglycerides and 6% increase in HDL cholesterol, with no significant change in LDL cholesterol. There was a significant reduction in coronary artery plaque progression in the fenofibrate-treated group compared to the placebo group. There was also a reduction in clinical endpoints in the treated group, although the study did not have statistical power to analyse these data. This is currently being examined in a larger randomised, prospective study of fenofibrate in people with diabetes examining harder cardiovascular end points.
The Veterans Affairs High-density lipoprotein cholesterol Intervention Trial (VA-HIT) Study Group carried out a randomised double-blind placebo controlled trial looking at the effect of treatment with gemfibrozil in 2500 men with established CHD and reduced HDL cholesterol and normal levels of LDL cholesterol (Rubins et al 1999). This cohort had a large diabetes subgroup. The study demonstrated that HDL cholesterol increased and triglycerides were significantly reduced in the gemfibrozil treated group. There was also a 22% relative risk reduction in primary endpoints in the treatment group and a 41% relative risk reduction in CHD related death in the subgroup of people with diabetes.
Although these studies look promising, larger studies looking at the effects of fibrates on clinical endpoints are necessary. No large study has looked at the combined effect of a fibrate and a statin and, although this might seem like the ideal combination in the person with diabetes, given the typical lipid profile, there are concerns regarding the safety of these agents in combination in terms of rhabdomyolysis.
Ezetimibe is a novel lipid-lowering agent that acts by selectively inhibiting cholesterol absorption without disrupting the absorption of fat soluble vitamins. It reduces LDL cholesterol by 15–20% and is mainly used in people who are intolerant of statins (especially at higher doses), or as combination therapy in people who are failing to reach target serum cholesterol levels despite high dose statins.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree