Abstract
At the time of writing there are no vaccines or specific antiviral therapies for the SARS-CoV-2 virus with significant reductions in mortality. Lessons learned from the SARS outbreak have definitely helped us to understand many aspects of this emerging virus and the associated pathologies. But no effective therapies have been developed for SARS that could be leveraged for the COVID-19 outbreaks.
All who drink of this remedy recover in a short time, except those whom it does not help, who all die. Therefore it is obvious that it fails only in incurable cases.
At the time of writing there are no vaccines or specific antiviral therapies for the SARS-CoV-2 virus with significant reductions in mortality. Lessons learned from the SARS outbreak have definitely helped us to understand many aspects of this emerging virus and the associated pathologies. But no effective therapies have been developed for SARS that could be leveraged for the COVID-19 outbreaks.
In this chapter, I briefly discuss some of the ideas that have been suggested and are currently being tested. I start with a simple primer on how the virus is diagnosed and how infections are currently treated depending on the severity of the disease. I also discuss some of the therapeutic strategies that are currently being tried, including vaccines.
How Is the Virus Diagnosed?
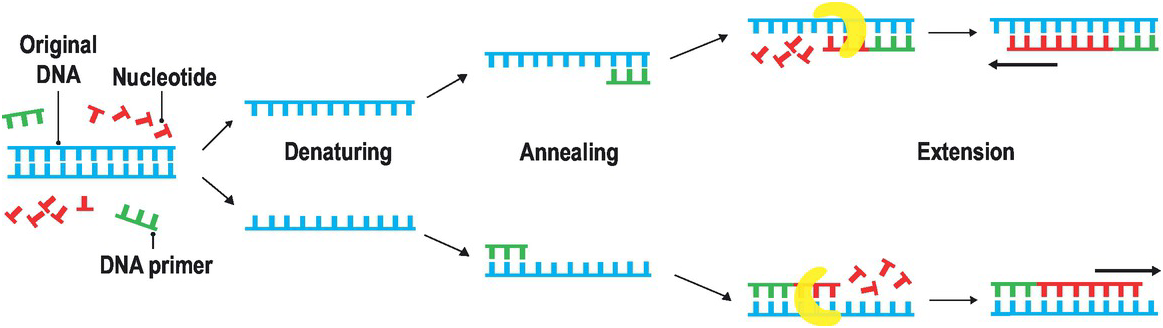
Testing is a highly efficient method to allocate healthcare resources to people who will be in need and to take measures to reduce the chance of infecting others. The virus was isolated from a sample from Wuhan on January 7, 2020, and the genomic sequences were shared with the international community on January 12. That allowed the rapid design of testing tools based on polymerase chain reaction, or PCR (Figure 8.1). This is a procedure for amplifying genomic material, in which specific pieces of genomic material are copied, the copies are copied again, and so on for several cycles, until the amount is large enough for identification. PCR tests measure directly the presence of the genomic material of the virus, but not the immune response to it. PCR tests require laboratory equipment and can take a few hours to generate results.
Figure 8.1 Polymerase chain reaction or PCR is a technique for exponentially amplifying the amount of genomic material. The process starts with two primers, design to complement the genomic region of interest. For instance, if we are interested in a particular gene, we will design the primers to be specific to the sequence of that gene. The sample DNA is heated so the two strands of DNA are separated. The primers will bind to the DNA of interest. A polymerase will extend the sections of the genome that bind to the specific primers, creating two copies per copy of DNA of the gene present. If the process is repeated through several cycles, the amount of DNA will amplify exponentially. Small amounts of genomic material can then rapidly expanded to large amounts.
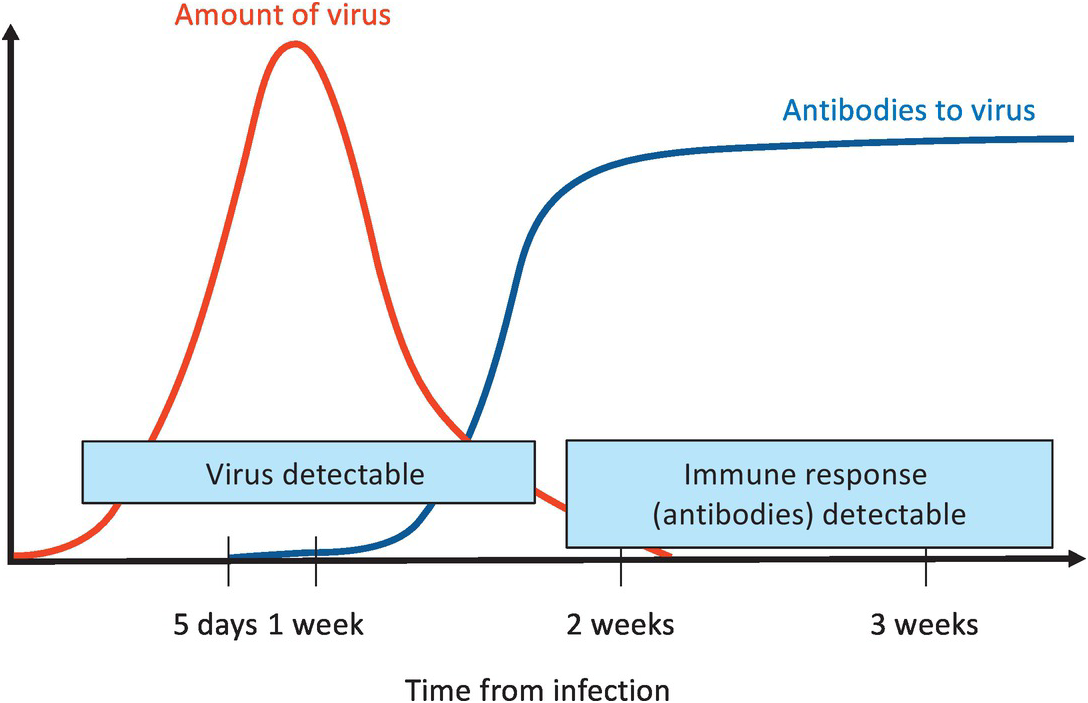
A couple of weeks after a person has been infected with SARS-CoV-2, the immune system develops antibodies – molecules that are able to recognize the virus very specifically. The identification of specific antibodies to the virus indicates that a person has been infected in the past and has been able to mount an effective immune response. Serology tests examine the blood for the presence of these antibodies. Because the generation of antibodies in an infected person takes a couple of weeks, antibody-based tests cannot provide a rapid assessment of the presence of an active virus. However, these tests are very useful to determine whether a person has been infected in the past, even if the virus is no longer there.
Serology tests are very useful for assessing how many people have been infected but not reported as such, due mostly to the mild or unobservable effects of the infection (Figure 8.2). Most of our estimates in the beginning of the pandemic were through mathematical modeling, with assumptions and large variance in estimates. Serology surveys could provide a more accurate assessment of true infection rates. They can also indicate that a person has been able to mount an effective response to the virus, and help determine whether the person can actively interact with more at-risk patients. Finally, they can help to estimate the rates of re-infection and the duration of the immune response. The immune responses to some viruses, such as measles, last for a lifetime, whereas the responses to others, including the common coronavirus circulating in humans, last only a couple of years. We do not know yet how long the immune response for SARS-CoV-2 will last.