The pathophysiology of stroke
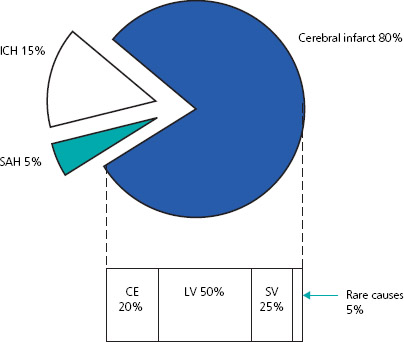
Stroke is caused by a sudden disruption to the blood supply to the brain. There are two main types: cerebral infarction and intracerebral haemorrhage, the latter of which includes subarachnoid haemorrhage (see Figure 7.1). Infarction and haemorrhage are not underlying diagnoses, as there are several different mechanisms (see Figure 7.2).
Cerebral infarction results from a blockage of arterial blood supply either by atherothromboembolism to large or small vessels, or embolisation from a proximal source such as the heart, as in atrial fibrillation. Rarer causes such as arterial dissection and inflammatory vasculopathies also occur. Following disruption of cerebral blood flow, there is disturbance to the neuronal electrical activity (reversible) and cellular membrane integrity (irreversible) through a neurochemical cascade. The ‘ischaemic penumbra’ is an area of brain that has not passed into the irreversible stage and has the potential to recover. This is the rationale for emergency therapy in cerebral ischaemia. Figure 7.3 shows the computed tomography (CT) appearances of various types of infarct.
Figure 7.1 Frequency and mechanism of stroke by pathological subtype. ICH, intracerebral haemorrhage; SAH, subarachnoid haemorrhage; CE, cardio-embolic; LV, large vessel; SV, small vessel. From Warlow C et al. Lancet 2003; 362: 1212.
Primary intracerebral haemorrhage (ICH) follows a rupture of blood vessels into brain tissue, resulting in direct neuronal injury and cerebral oedema (see Figure 7.4).
Clinical assessment
Stroke and TIA are clinical diagnoses, characterised by the sudden onset of a focal neurological deficit. It is impossible to reliably differentiate cerebral infarction from cerebral haemorrhage on clinical grounds alone.
The particular symptoms of stroke and TIA depend on which part of the brain is affected and these are listed in Box 7.1. There are also a number of other disorders that may mimic stroke (Box 7.2), but these can often be differentiated by history and physical examination.
The traditional difference between a stroke and TIA is timing. In TIA, neurological symptoms and signs resolve within 24 hours.
Figure 7.2 Different mechanisms leading to intracerebral haemorrhage.
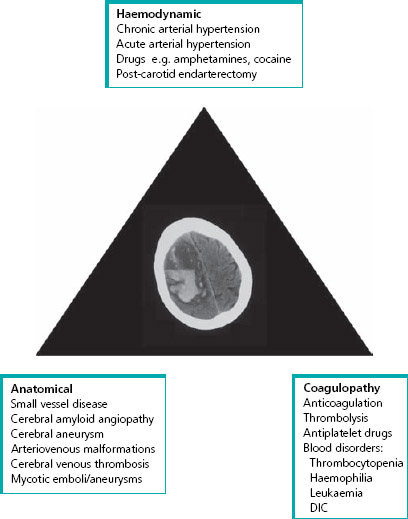
Figure 7.3 CT brain scan showing (A) established lacunar (small vessel) infarct, (B) acute left middle cerebral artery territory infarct, (C) diffuse small vessel disease and (D) established left posterior cerebral artery infarct.
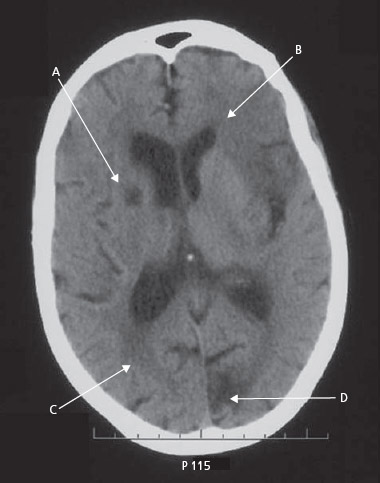
Figure 7.4 CT brain scan showing a large-volume intracerebral haemorrhage (A) in the right cerebral hemisphere, with evidence of intraventricular extension (B).

Box 7.1 Clinical features of stroke/TIA with arterial territory
| Anterior (carotid) circulation | Posterior (vertebrobasilar) circulation |
| Cortical dysfunction: | Cranial nerve palsy |
| dysphasia | Ataxia/incoordination/ |
| sensory/visual inattention | disequilibrium* |
| hemianopia | Diplopia* |
| Isolated homonymous | |
| hemianopia | |
| Monocular blindness | Bilateral visual loss |
| Unilateral weakness | Unilateral/bilateral weakness |
| Unilateral sensory disturbance | Unilateral/bilateral sensory |
| disturbance | |
| Dysarthria* | Dysarthria* |
| Neuromuscular dysphagia* | Neuromuscular dysphagia* |
* Unlikely to be TIA or stroke if symptoms are in isolation.
However, most TIAs last less than 1 hour and those of the eye last for only a few minutes. Many so-called TIAs lasting several hours are actually infarcts (as evidenced on CT scanning).
Our concepts of stroke and TIA are evolving. It is more helpful to think in terms of a ‘brain attack’, particularly for those assessed within the first few hours of their event, in whom it is unclear whether it will turn out to be a TIA or a stroke. For patients who present with a TIA, it is possible to identify those at the highest risk for stroke using a simple score (see the ABCD2 score in Box 7.3). This is crucial in prioritising patients, organising investigations, modifying risk factors and starting effective secondary prevention (see Box 7.4).
Box 7.2 Stroke mimics
- Seizures
- Sepsis with previous stroke (old neurological signs may become more pronounced)
- Cerebral tumour
- Subdural haemorrhage
- Intoxication with alcohol
- Migraine
- Inner ear disease
- Transient global amnesia
- Cervical spondylosis with nerve entrapment
- Functional disorder (rare in old age)
Box 7.3 The ABCD2 score and subsequent stroke risk
The National Stroke Strategy suggests that patients with a TIA and score of 5 or more should be admitted to hospital for immediate specialist investigation.
| ABCD2 | Score | |
| Age | > 60 years | 1 |
| Blood pressure | >140/90 mmHg | 1 |
| Clinical features | Unilateral weakness | 2 |
| Speech disturbance alone | 1 | |
| Other | 0 | |
| Duration of symptoms | >60 minutes | 2 |
| 10–59 minutes | 1 | |
| <10 minutes | 0 | |
| Diabetes mellitus | Present | 1 |
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree