Introduction 151
History of blood glucose monitoring 152
Monitoring in type 2 diabetes 153
Monitoring options 160
Testing for ketones 167
Other factors that can influence monitoring of diabetes 168
Conclusion 169
References 169
Research has clearly demonstrated the link between elevated blood glucose levels and diabetic microvascular complications in people with type 1 diabetes (The Diabetes Control and Complications Trial (DCCT) 1993) and type 2 diabetes (UK Prospective Diabetes Study (UKPDS) 1998). There is evidence that elevated blood glucose levels are also linked to macrovascular complications (UKPDS 1998) (see Chapter 8). Self-monitoring, by measuring glucose levels in either blood or urine, can help people with diabetes make sense of and contribute to the decisions about self-management. Self-monitoring improves the individual’s understanding of his or her diabetes and assists the person to maintain day-to-day control of his or her blood glucose. This can enable the individual to explore the impact of exercise, diet and treatment on blood glucose levels. The value of self-monitoring of blood glucose in people with type 1 diabetes is well established, however, self-monitoring – especially blood glucose monitoring by people with type 2 diabetes – remains fiercely debated (Gallichan 1997, Reynolds & Strachan 2004, Reynolds & Webb 2006). One of the challenges for both the person with diabetes and the healthcare professional is to make this serious and complicated disease become ‘real’ so that it can be controlled successfully enough to avoid diabetic complications. It would seem reasonable, therefore, that self-monitoring, which allows the person with diabetes to recognise and correct abnormal results, could be a cornerstone to self-management of diabetes.
The two methods for self-monitoring of glucose in diabetes are through blood glucose monitoring or urine testing for glucose. An alternative to self-monitoring would be to provide a blood test at the surgery or hospital for measurement of glycated haemoglobin (HbA1c) (Owens et al 2005).
This chapter addresses monitoring in type 1 diabetes and discusses some of the controversies of monitoring in type 2 diabetes.
Self-monitoring of blood glucose (SMBG) became available to people with type 1 diabetes only in the late 1970s, initially with the availability of reagent strips that required a lengthy complex procedure including visual reading of colour change for an accurate result. In the UK, provision of strips came from the hospital pharmacy budget and there was no provision for them in primary care.
In recent years, blood glucose meters have been developed and refined and are available at relatively low cost to individuals or obtainable at no cost from many hospital clinics and GP surgeries. Strips and lancets to prick a finger to obtain a blood sample require to be prescribed by the GP. Alternatively, they can be bought at significant cost from the pharmacist (£15–£25 per box of 50 strips). Results are precise providing technique is accurate although are less exact at whole blood glucose levels less than 3.5 mmols/L. Blood glucose meters have improved significantly over recent years with more sophisticated technology and are easier and quicker to use. The procedure involves obtaining a fingertip drop of blood placing it onto a strip that has been sited or about to be sited, in a meter. The result is available anywhere within 5–30 seconds. More recently, some pharmaceutical companies have modified their meters to accept blood from alternative, less painful sites to the fingertips. The amount of blood required for an accurate result has reduced significantly and is as little as 0.3 microlitres.
URINE TESTING
Before blood glucose monitoring (BGM) becoming available, people with diabetes were asked to perform tests to measure glucose in the urine. As with measuring blood glucose, urine testing has also become a less complex procedure, which involves dipping a reagent strip into urine for 2 seconds then waiting up to 30 seconds for the strip to change colour if glucose is present. No glycosuria indicates that the blood glucose level several hours before was probably under 10 mol/L and likely to be in the acceptable range for preventing long-term complications. People with diabetes do not like urine testing, saying that repeated ‘negative’ results can lead them to believe that diabetes has gone away (Lawton et al 2004). Urine testing does not give any indication of hypoglycaemia, which can be an immediate complication of too much insulin or oral hypoglycaemic therapy. Caution should be exercised in interpreting urine testing results in the older population. The renal threshold is higher in this group and hence an individual might have a high blood glucose but no glycosuria. In this situation, regular blood glucose monitoring would detect any progressing hyperglycaemia.
HBA1C MEASUREMENT
Alternatives to self-monitoring are to do no monitoring at all and instead have a test performed by the healthcare professional known as a ‘long-term’ test: glycated haemoglobin or HbA1c. Red blood cells containing haemoglobin are made in the bone marrow, circulate for 120 days and are then removed by the spleen and liver. These millions of red cells have a mean life of around 49 days when prevailing blood glucose binds irreversibly with haemoglobin to form glycated haemoglobin or HbA1c. Measuring glycated haemoglobin is done in most laboratories and the result offers a very good test of how average the blood glucose level has been in the previous seven weeks. The DCCT (1993) demonstrated that to minimise complications in type 1 diabetes, the HbA1c should be below 7.5%. The UKPDS (1998) demonstrated that to minimise complications in type 2 diabetes the HbA1c should be below 7.1%. Nearly all research looking at glycaemic control outcomes uses HbA1c as the outcome measure. The disadvantage of the HbA1c is that it does not indicate swings in blood glucose or hypoglycaemia, nor give immediate feedback to enable the individual to make decisions regarding self-treatment or lifestyle adjustments. It remains debatable as to whether swings in blood glucose levels are damaging (Buse 2003, Davidson 2003).
The Clinical Standards Board for Scotland (2001) recommends an absolute minimum of an annual HbA1c measurement and more often as indicated. The exception to this is in pregnant women with diabetes, in whom it is important to know the trend in glycaemic control on a month-to-month basis. For someone with changing diabetes management the HbA1c would be checked not more than 2-monthly and 3- to 6-monthly in others.
FRUCTOSAMINE
This is another form of assay used to measure glucose binding to proteins in the blood. It reflects the average blood glucose level over the preceding 2–3 weeks. It is really only of value in people who suffer from a haemoglobinopathy in whom an HbA1c measurement is not accurate (Owens et al 2005).
MONITORING IN TYPE 2 DIABETES
In the early years, BGM was taught to people with type 1 diabetes to enable the regulation of glycaemic control through adjustment of insulin by the person with diabetes. In recent years, as the seriousness of type 2 diabetes has become increasingly recognised, so has the move to encourage people with type 2 diabetes to self-monitor (European NIDDM Policy Group 1994).
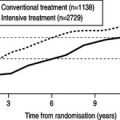
A major factor contributing to the increase in BGM in type 2 diabetes has been the recognition that type 2 diabetes is a progressive disease that, over time, requires increasing and changing treatment. Although someone with type 2 diabetes might start treatment with a modified diet, the UKPDS (1998) demonstrated progression to one or more types of oral hypoglycaemic agent and then to insulin therapy.
Pharmacists are keen to support people with diabetes and this includes educating individuals on how to use a meter.
The American Diabetes Association declared that SMBG has revolutionised management of diabetes (ADA 2003):
Using SMBG, patients with diabetes can work to achieve and maintain specific glycemic goal targets.
Although the above quote is questionable in terms of the evidence available, the ADA also states that SMBG can monitor the efficacy of diet, medications and exercise. The Association recommends that all people on insulin or oral hypoglycaemic agents should perform SMBG on a daily basis. The number of tests a day should be agreed between the healthcare professional and the individual. The ADA affirms that the role of SMBG in people who control their diabetes with diet alone is not known.
The European consensus guidelines states that urine testing can be useful for people who cannot manage blood testing where this is indicated in people whose glucose control is deteriorating or who take insulin (European Diabetes Policy Group 1999). This suggests that BGM is the first choice of monitoring but it also suggests that self-monitoring in people whose diabetes is stable might be unnecessary.
Within the UK there has been the continued development of a consensus statement around the debate of SMBG and recommendations are presented in Table 7.1 (Owens et al 2005). These recommendations have been developed around current research and expert opinion (Reynolds & Webb 2006).
| Diabetes type | Treatment group | Monitoring regimen |
|---|---|---|
| Type 1 diabetes | All people with type 1 diabetes | SMBG should be regarded as an integral part of treating all people with type 1 diabetes People with type 1 diabetes should be educated to SMBG and adjust treatment appropriately The majority of patients with type 1 diabetes should consider SMBG four or more times per day to prevent hypoglycaemia and control hyperglycaemia Avoiding metabolic emergencies such as diabetic ketoacidosis might require frequent SMBG |
| Diabetic pregnancy | Diabetic pregnancy | Pregnant women with type 1 diabetes, plus those with type 2 diabetes requiring insulin and patients with gestational diabetes requiring insulin should SMBG at least four times per day to include both fasting and post-meal blood glucose measurements In diet-treated patients it may be necessary to SMBG with the same frequency as insulin-treated patients to ensure strict glycaemic control In insulin-treated patients increased frequency of testing may be necessary in the first trimester when the risk of hypoglycaemia is greatest |
| Type 2 diabetes | Intensive insulin therapy | People who adopt intensive insulin therapies require regular feedback regarding SMBG levels People with type 2 diabetes who use a multiple daily insulin regimen should SMBG in the same way as those with type 1 diabetes Fasting blood glucose should be tested daily during basal insulin dose titration |
| Type 2 diabetes | Conventional insulin therapy | People with type 2 diabetes who are using a conventional insulin regimen and who have stable control should SMBG two or three times a week People with type 2 diabetes who are using a conventional insulin regimen and who have less stable control should SMBG at least once daily, varying the time of testing between fasting, pre-meal and post-meal Fasting blood glucose should be tested daily during basal insulin dose titration |
| Type 2 diabetes | Combined insulin and oral antidiabetic therapy | Fasting blood glucose should be tested daily during basal insulin dose titration People with type 2 diabetes who use insulin or oral hypoglycaemic agents should SMBG at least once daily, varying the time of testing between fasting, pre-meal and post-meal |
| Type 2 diabetes | Diet and exercise | People with type 2 diabetes who have good control on diet and exercise, metformin or glitazone treatment do not need SMBG monitoring, unless they are destabilized by other factors Glycaemic control managed through diet and exercise in people with type 2 diabetes is best monitored through HbA1c testing Patients with type 2 diabetes managed only by diet and exercise do not normally require routine SMBG Informed patients might choose SMBG as a means of monitoring lifestyle changes |
| Type 2 diabetes | Metformin (±glitazone) | As for diet and exercise |
| Type 2 diabetes | Glitazone (±metformin) | As for diet and exercise |
| Type 2 diabetes | Sulphonylurea alone (or in combination with oral antidiabetic agents) | Hypoglycaemia can be more common than assumed in people with type 2 diabetes on sulphonylureas and SMBG will reveal this situation |
THE EVIDENCE
A health technology assessment (HTA) systematic review examining blood glucose monitoring in diabetes was published in 2000 (Coster et al 2000). Part of the review related to BGM in type 2 diabetes. Only eight randomised controlled trials (RCTs) in relation to BGM in type 2 diabetes were identified as being robust enough to be included in the review. The eight RCTs included comparisons of blood testing, urine testing and no testing. Interventions were not standardised and training of individuals and adherence were not addressed systematically. No trial required subjects to modify their drug therapy in accordance with self-monitoring results. Six studies were included in a meta-analysis. The review concluded:
…that the results do not provide evidence for clinical effectiveness of an item of care with appreciable costs. Further work is needed to evaluate self-monitoring so that resources for diabetes care can be used more efficiently. (Coster et al 2000)
A more recent meta-analysis of SMBG in people with type 2 diabetes not using insulin looked at six RCTs and concluded cautiously that SMBG has a small beneficial effect on glycaemic control but, again, stated that there were methodological issues with the studies (Welschen et al 2005). From these studies it would appear that some people benefit more from SMBG than others; however, the cost of SMBG is very likely to be offset against the longer-term costs of care for the same people (Bandolier 2005). Given that BGM in type 2 diabetes remains so controversial, it is prudent at this point to consider why clinicians appear to be ignoring the evidence, or, rather, ignoring the lack of evidence (Barraclough 2003). There are several ways of interpreting ‘lack of evidence’:
▪ The research has not measured what it should have measured.
▪ The intervention might have had positive effects for some, but not all subjects and an RCT would not necessarily identify these differences.
▪ The research might not have been done.
▪ There is no supporting evidence, even when trials with adequate power have been properly conducted.
▪ Some people believe that the only evidence worth considering is that obtained from RCTs.
▪ Some studies might not have been able to separate other factors that could influence glycaemic control; they might not have had control groups (Gallichan 1997).
Clues about ‘other factors’ are hinted at in the three qualitative studies described below.
A qualitative study of people with type 1 diabetes found that, although there is no doubt that blood glucose monitoring is acceptable and useful for some, it is clearly difficult and painful, both physically and psychologically, for others (Fox et al 1994). Some people are unable to make the connection between testing and using test results to influence glycaemic control (Fox et al 1994).
A more recent grounded theory study of 40 people with type 2 diabetes diagnosed within the previous 6 months and interviewed twice during a 9-month period found that those who had optimal glycaemic control viewed monitoring in a positive light. However, the reverse was true for those who observed results outside the recommended range (Peel et al 2004). Positive aspects of monitoring were stated as modifying lifestyle and adjusting regimens based on results. Negative aspects identified were: evidence of the existence of their diabetes; additional distress if results were inexplicable; they did not know what to do with the results; monitoring for the benefit of the doctor, which was especially annoying if health professionals did not enquire about results. Not enquiring about results might reflect the reliance of healthcare professionals on HbA1c.
The same research group also recently completed a grounded theory study on urine testing (Lawton et al 2004). Forty people with newly diagnosed type 2 diabetes were interviewed three times over 1 year. They expressed ‘profoundly negative views’ on urine testing. Urine testing was perceived as less accurate, less hygienic and less convenient than BGM. Negative urine results were seen as an indicator that they did not have diabetes. It is interesting to compare these results with those of a study where a more positive view of urine testing was taken (Miles et al 1997). It suggests differences in diabetes education programmes and might reflect the personal views of the diabetes educators.
The fact that SMBG, from the point of view of the person with diabetes, has many costs and benefits is reflected in a survey of people with type 1 and type 2 diabetes who take insulin in the Tayside Region of Scotland (Evans et al 1999). This study showed that uptake of BGM strips from pharmacists was far below that prescribed, suggesting that people are not testing as often as requested by health professionals.
Another study showed that for those with type 2 diabetes taking insulin, SMBG was a useful aid and improved glycaemic control when insulin adjustment had been taught (Franciosi et al 2001). However, the same study showed that, in those not treated with insulin, SMBG was associated with higher HbA1c levels and higher psychological burden. The authors stated that SMBG should be part of wider educational programme but at the same time recommended that SMBG should be limited to those on insulin therapy.
Conversely, a prospective, multicentre randomised controlled study showed that glycaemic control improved significantly in the intervention group (Schwedes et al 2002). The intervention group received a structured diabetes education programme that included feedback. Participants maintained a diary of eating habits and SMBG results. Self-monitoring resulted in marked improvement in general well-being with significant improvement in the subitems depression and lack of well-being (Schwedes et al 2002). The researchers concluded that meal-related SMBG within a structured counselling programme improved glycaemic control in the majority of the intervention group of this study. The weakness of the study was that the final outcome measures were assessed at 6 months after the completion of the intervention and it is well recognised that an intervention effect can wear off after 6 months. However, the point is that it is still possible for SMBG to be effective if it is presented in the correct context of an effective education programme. In a later study, the same group demonstrated that SMBG was beneficial in the context of a short, structured education programme that included considering options for action (self-reflection) and believing in self-efficacy (self-regulation) (Siebolds et al 2006).
FINANCIAL IMPLICATIONS TO THE HEALTH SERVICES
Blood glucose monitoring is a costly procedure. The publication of the National Institute for Health and Clinical Excellence (NICE) guideline on blood glucose control in type 2 diabetes (NICE 2002) resulted in restrictions by GPs on the prescribing of blood glucose strips. The NICE guideline stated that self-monitoring:
▪ should not be considered as a stand-alone intervention
▪ should be taught if the needs and purpose are clear and agreed with the individual
▪ can be used in conjunction with appropriate therapy as part of integrated care.
Some primary care organisations have interpreted these guidelines to mean that as SMBG in type 2 diabetes has no evidence base, substantial cost savings can be gained from restrictions on prescribing SMBG strips. This has been refuted by Diabetes UK (2004). It is acknowledged that there are resource implications in utilising SMBG. Such resources include the actual equipment for BGM as well as the support required from health professionals to teach the skill and assist individuals to place SMBG within their own lifestyle context.
The NHS National Prescribing Centre (2002) produced a bulletin summarising the evidence for SMBG in type 2 diabetes. The first point was that the NHS spends 40% more on BGM materials than it does on oral hypoglycaemic agents (£90 million versus £64 million in 2001). The bulletin goes on to repeat the recommendations of the NICE report as above but also points out that there is no evidence that BGM is more effective than urine testing. It concludes that measurement of HbA1c is likely to provide more helpful information than day-to-day monitoring. This ignores the fact that SMBG and HbA1c are different measures measuring different aspects of glycaemic control. It is possible for people with diabetes to have HbA1c levels at target but be experiencing both frequent hypoglycaemia and/or hyperglycaemia. The above statement also raises the issue of patient empowerment.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree