Case study 63.1
A 55-year-old male presented with a 2-month history of an enlarging, painless right neck mass. The mass was mobile, measuring 3 cm in dimension. Excisional biopsy demonstrated diffuse large B-cell lymphoma (DLBCL). Bone marrow biopsy was negative, lactate dehydrogenase was within normal limits, and positron emission tomography and computed tomography (PET–CT) demonstrated hypermetabolic adenopathy confined to the right neck. He denied fevers, drenching night sweats, or unexplained weight loss. Thus, the stage is IA. The patient received four cycles of R-CHOP (rituximab, cyclophosphamide, doxorubicin, vincristine, and prednisone), and postchemotherapy PET–CT showed a complete remission (CR) (Figure 63.1).
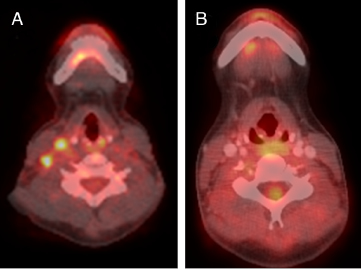 Figure 63.1 PET-CT of the neck showing hypermetabolic lymph nodes in the right neck (A), which resolved after chemotherapy (B). (Color plate 63.1)
Figure 63.1 PET-CT of the neck showing hypermetabolic lymph nodes in the right neck (A), which resolved after chemotherapy (B). (Color plate 63.1)
• Is consolidation radiation therapy (RT) necessary if a CR by PET is achieved after R-CHOP for DLBCL?
The randomized trials that demonstrated that consolidation RT decreases the risk of relapse after CHOP were all conducted in the pre-rituximab and pre-PET era. With more effective systemic therapy (rituximab) and improved chemotherapy response assessment (PET), some have contended that if a CR is achieved by PET, then consolidation RT is no longer necessary.
No phase III trials, however, in the rituximab–PET era have as yet addressed this issue. Retrospective studies evaluating patients in a CR by PET after R-CHOP have shown that RT still decreases the risk of relapse, in both early and advanced disease. It must be remembered that a negative PET does not necessarily indicate that all disease has been eradicated. A critical mass of tumor cells is necessary for a PET signal to be detected. There are currently no radiological studies that can detect microscopic disease. Thus, the standard of care remains consolidation RT after chemotherapy for localized DLBCL.
The contrasting clinical scenario also deserves attention, specifically a persistently positive PET scan after completion of chemotherapy. If a patient with localized disease has clearly not responded well to chemotherapy, treatment options include high-dose chemotherapy and autologous stem cell transplantation or RT to the local area. Few studies have compared the two. Historical data indicate that ∼50% of patients achieve long-term failure-free survival with RT alone for stage I disease but much inferior results for stage II (∼20%). Therefore, we favor the transplant approach for stage II patients and an individualized approach for stage I. Prior to a fairly radical change in treatment such as stem cell transplant, biopsy confirmation of active disease is mandatory.
For a patient who has responded well clinically but has a positive postchemotherapy PET scan, proceeding with consolidation RT is still a reasonable option, perhaps using a higher total dose (∼40 Gy). Clinical outcomes are best when the PET is negative after chemotherapy, but a significant percentage of patients who are still PET positive remain disease-free after consolidation RT.
This patient received 30 Gy of consolidation RT to the right neck. Treatment was well tolerated with transient odynophagia and fatigue.



