Section 6 Special topics
Childhood and adolescence
Type 1b diabetes has the same clinical presentation as T1aDM, but islet autoantibodies are absent.
The principal aims of treatment of diabetes in childhood are:
• achievement of good metabolic control
• attainment of normal growth and development
• avoidance of serious hypoglycaemia
Management of diabetes in childhood
Cerebral oedema
• more profound dehydration, hyperventilation and acidosis at presentation
• excessive and rapid fluid administration, especially if initial serum osmolality is greater than 320 mOsm/L
• failure of serum sodium level to rise as hyperglycaemia resolves
• initial IV insulin bolus or too early initiation of insulin infusion.
• administration of mannitol (1 g/kg over 30 min)
• decreasing fluid rate to 75% or less of maintenance rate
Insulin therapy
Injection regimens should be individualized and include:
• Basal bolus regimen: 40–60% of the total daily dose as a basal insulin analogue (glargine, detemir) in 1–2 doses a day plus a rapid-acting insulin analogue with each meal (in some patients after the meal); soluble human insulin requires administration at least 20–30 min before each meal
• Intermediate-acting human (or neutral protamine Hagedorm; NPH) insulin twice daily and soluble human insulin 20–30 min before each meal
• Two injections daily of a (pre-mixed) mixture of short or rapid and intermediate-acting insulin before breakfast and before the evening meal
• Three injections using some variation of the following: a mixture of short- or rapid-acting and intermediate-acting insulin before breakfast, rapid-acting or soluble human insulin before the afternoon snack or evening meal, and intermediate or basal/long-acting insulin before bed.
Glargine or detemir insulins should not be mixed with any other insulin.
Paediatric diabetes outpatient care
Diabetes is managed primarily in the outpatient setting by a team including:
• a paediatrician specializing in diabetes
• a paediatric psychologist with knowledge of childhood diabetes and chronic illness
• possibly a paediatric social worker trained in childhood diabetes.
Education
• overall health and well-being is assessed
• growth and vital signs are monitored
• routine screening for diabetes-associated complications and comorbidities is performed
• blood glucose records (including HbA1c) are assessed
The dietitian should review dietary habits and provide ongoing nutrition education as needed.
Diabetes management in school
• contact information for the child’s family as well as their diabetes care providers
• information regarding routine management of diabetes (blood sugar monitoring, insulin administration and dosing, snack times)
• an emergency plan for management of hypoglycaemia and hyperglycaemia.
Sick-day management
• Written instructions are important
• Most parents require telephone advice when first facing sickness in their child and some may need repeated support.
However, infections and other illnesses may be associated with an increase in insulin requirements.
Transition to the adult diabetes clinic
Adolescence is a transitional stage of human development that:
• occurs between childhood and adulthood
• is characterized by significant and complex biological, social and psychological changes.
A powerful predictor of good self-care is self-efficacy. Adolescents should be encouraged to have confidence in their capability to make decisions and take actions that demonstrate good diabetes self-care (see Appendix 6.1: Principles of dietary planning in children with diabetes).
Diabetes in the elderly
Diabetes, mainly type 2 diabetes, is particularly common in the elderly; more than 50% of patients in the UK are over 60 years of age (the majority having type 2 diabetes). In many countries diabetes affects 10–25% of elderly people (> 65 years), with particularly high rates in populations such as Pima Indians, Mexican Americans and South Asians. Glucose tolerance worsens with age, the main factor being impairment of insulin-stimulated glucose uptake and glycogen synthesis in skeletal muscle; progressive insulin resistance also contributes (Table 6.1). Symptoms of diabetes may be non-specific, vague or absent.
Table 6.1 Factors contributing to glucose intolerance in old age
| Impaired glucose disposal and utilization |
NIMGU accounts for 70% of glucose uptake under fasting conditions (primarily into the CNS) and for 50% of post-prandial glucose uptake (especially into skeletal muscle) |
| Impaired glucose-induced insulin secretion |
Aims of treatment
The management of T2DM and its common comorbidity of cardiovascular disease is complicated because of the added effects of ageing on metabolism and renal function, the use of potentially diabetogenic drugs, and low levels of physical activity. Cardiovascular risk is particularly high because many risk factors of the metabolic syndrome can be present for up to a decade before T2DM is diagnosed. Management strategies for many elderly people with diabetes are the same as those for the younger population, with similar lipid-lowering and antihypertensive treatment schedules, and aspirin or clopidogrel for patients with increased cardiovascular risk. Effective delivery of diabetes care depends on close cooperation between hospital and community, the involvement of diabetes teams and practice nurses, and attention to all causes of disability and ill-health (Table 6.2).
Table 6.2 Special characteristics of older subjects with diabetes
Management of diabetes in women of childbearing age
Pre-pregnancy and pregnancy care
Contraception
Pregnancy should be planned; good contraceptive advice and pre-pregnancy counselling are essential.
Pre-pregnancy targets for blood sugar
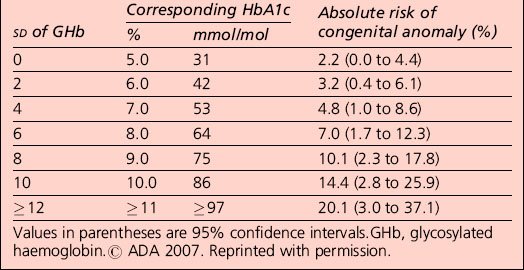
Observational evidence has found an association between maternal glycaemia (before and during pregnancy) and the increased risk of congenital malformation and miscarriage. The risk of congenital anomaly in the offspring of women with pre-pregnancy diabetes is increased with an increasing level of HbA1c. No HbA1c threshold for such effects has been identified (Table 6.3).
Table 6.3 Derived absolute risk of major or minor congenital anomaly in association with the number of standard deviations (SD) of glycosylated haemoglobin above normal, and the approximate corresponding HbA1c concentration, measured periconceptually
Oral medication before and during pregnancy
Nutritional management
It is good clinical practice to provide dietary advice to women before, during and after pregnancy.
Advice on diet and exercise should be offered in line with recommendations for adults with diabetes.
Optimization of glycaemic control
Glucose monitoring
All women with pre-gestational diabetes should be encouraged to achieve excellent glycaemic control.
• between 4 and 6 mmol/L preprandially
• < 8 mmol/L 1 hour postprandially, or
• < 7 mmol/L 2 hours postprandially
Complications during pregnancy
Fetal assessment
All women should be offered scanning to include:
• a gestational age scan between 11 and 13 weeks (+ 6 days) in association with biochemical screening and nuchal translucency measurement to risk assess for trisomies
• a detailed anomaly scan including four-chamber cardiac view and outflow tracts between 20 and 22 weeks.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree