Osteoporosis
Osteoporosis is defined by the World Health Organization (WHO) as ‘a progressive, systemic skeletal disease characterised by low bone mass and micro-architectural deterioration of bone tissue, with a consequent increase in bone fragility and susceptibility to fracture.’ Often known as ‘the silent disease’, due to the slowly progressive and asymptomatic decline of skeletal tissue, there may be no clinical signs until a person presents with a painful fracture. The most common areas for fracture are the spine (Figure 5.1), wrist and hip (Figure 5.2); but the general nature of the condition means that any bone may be involved. Chronic pain, disability, loss of independence and premature death may result, which is why it is important to identify and manage those at risk.
Aetiology
Osteoporosis predominantly affects post-menopausal women as a result of oestrogen deficiency but it also occurs in men. One in three women and one in twelve men will suffer an osteoporotic fracture after the age of 50. The incidence of osteoporosis rises with increasing age but fracture risk is higher in older people compared with younger people with the same bone mineral density. Around half of cases in men are associated with hypogonadism (20%), corticosteroid use (20%) or alcohol excess (5%) so these risk factors should be specifically sought. Secondary causes of osteoporosis (see Box 5.1) occur in both sexes.
Diagnosis
The standard for the diagnosis of osteoporosis is assessment of bone mineral density (BMD) by axial dual-energy X-ray absorptiometry (DEXA). A diagnosis of osteoporosis may also be suspected from any of the following:
- marked osteopenia on plain X-ray
- a previous fragility fracture
- the identification of risk factors for osteoporosis.
The WHO classification of osteoporosis has been widely adopted and is based on the measurement of BMD with reference to the number of standard deviations (SD) from the mean in an average 25-year-old woman, known as the T-score (see Box 5.2). The threshold for osteoporosis is at least 2.5 SD below this reference point (i.e. a T-score of –2.5 or more). T-scores can vary by anatomical site so the prediction of fracture risk is usually based on measurements estimated at the femoral neck as this is most predictive of hip fracture (the major cause of loss of independence, mortality and cost).
Assessing fracture risk
Although low BMD is helpful in assessing fracture risk, it does not alone predict whether a person will sustain a fracture in absolute terms. Other factors such as a tendency to fall should also be considered. Those who have already had one fragility fracture are at highest risk of sustaining further fractures and should be prioritised for investigation and treatment. Over the past few years many meta-analyses have been carried out to identify risk factors that could be used to identify those at risk of osteoporosis and fracture. A 10-year fracture prediction tool, currently in development, incorporates clinical risk factors that are independent of BMD. These include:
- age
- prior fragility fracture
- smoking history
- excess alcohol use
- a family history of hip fracture
- rheumatoid arthritis
- systemic corticosteroid use.
Figure 5.1 Lateral thoracic spine X-ray showing osteopenia and multiple wedge vertebral collapses.
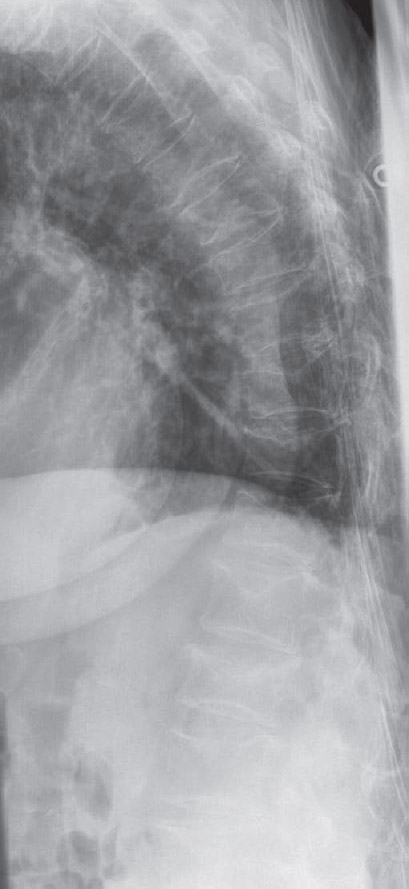
Figure 5.2 Pelvic X-ray showing osteopenia and a displaced subcapital fracture of the left neck of femur.

Box 5.1 Risk factors for the development of osteoporosis
Non-modifiable
- Female gender
- Family history of osteoporosis (especially maternal history of hip fracture at less than 75 years old)
- Caucasian or Asian ethnicity
- Age more than 65 years
- Previous fragility fracture
Modifiable
- Low body mass index (less than 19 kg/m2)
- Smoking
- Alcohol excess
- Low calcium intake and vitamin D deficiency
- Inactivity
Hormonal
- Menopause before age 45 years or prolonged untreated amenorrhoea
- Male hypogonadism
Secondary causes
- Rheumatoid arthritis
- Hyperthyroidism
- Malabsorption (particularly coeliac disease)
- Chronic liver disease
- Primary hyperparathyroidism
- Prolonged immobilisation
- Anorexia nervosa
Drugs
- Glucocorticoids
- Anticonvulsants
- Prolonged heparin therapy
- Cytotoxic therapy
Box 5.2 WHO classification of osteoporosis based on bone mineral density
- Normal: T-score of –1 SD or more
- Low bone mass (osteopenia): T-score between –1 and –2.5 SD
- Osteoporosis: T-score below –2.5 SD
- Severe (established) osteoporosis: T-score below –2.5 SD, with one or more associated fragility fractures
SD, standard deviation.
Box 5.3 Further investigation of fragility fractures and possible osteoporosis
- Full blood count
- Erythrocyte sedimentation rate or plasma viscosity
- Serum urea, creatinine and electrolytes
- Serum calcium, alkaline phosphatase and phosphate
- Thyroid function tests
- Liver function tests
- Serum electrophoresis and urinary Bence-Jones protein
Additional investigations that may be required
- Lateral thoracic spinal X-ray
- Testosterone and luteinising hormone (men)
- Parathyroid hormone
- Vitamin D levels
Investigations in osteoporosis or after a fragility fracture
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree








