Case study 48.1
Patrick is a 66-year-old man who developed progressively worsening headaches and left-sided weakness over a 2-week period. He fell at home and was taken to a local hospital. A computed tomography (CT) scan of the head demonstrated a mass lesion isodense to gray matter in the right frontal lobe, with a considerable amount of associated vasogenic cerebral edema (see Figure 48.1). After contrast administration, the lesion was noted to enhance homogeneously. A second lesion was seen in the superior right frontal lobe, which also demonstrated homogeneous contrast enhancement. Dexamethasone was administered in the emergency room upon discovery of the tumor, and he was admitted to the hospital for further evaluation.
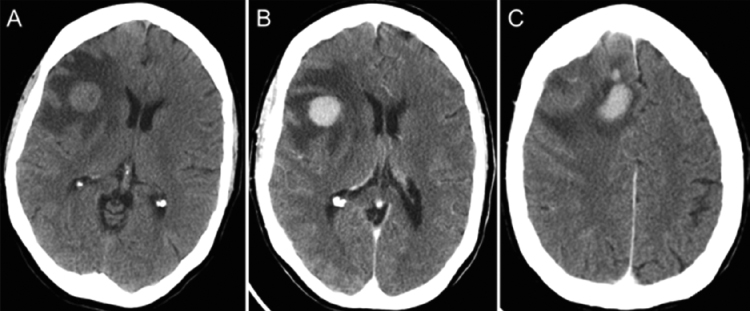 Figure 48.1 Computed tomography scan shows several right frontal mass lesions that are hyperdense prior to (A) and homogeneously enhancing after administration of contrast dye (B and C). The masses are surrounded by a hypodense area with finger-like protrusions consistent with vasogenic edema.
Figure 48.1 Computed tomography scan shows several right frontal mass lesions that are hyperdense prior to (A) and homogeneously enhancing after administration of contrast dye (B and C). The masses are surrounded by a hypodense area with finger-like protrusions consistent with vasogenic edema.
1. When should central nervous system (CNS) lymphoma be considered most likely in the differential diagnosis of a patient with a brain tumor?
- Presentation with a seizure
- Patient younger than 50
- Presence of multifocal enhancing mass lesions
- Prominent visual impairment as a chief symptom
- Presence of fevers
Primary CNS lymphoma (PCNSL) is rare, accounting for 2.2% of primary brain and nervous system tumors. The median age at diagnosis is between 53 and 61 years, although it can occur at any age. Patients often present with focal neurologic deficits or symptoms or signs of increased intracranial pressure, and less commonly present with neuropsychiatric symptoms, seizures, or ocular symptoms. Common imaging findings include the presence of multiple enhancing lesions with associated cerebral edema and mass effect.
Following hospital admission, CNS lymphoma was considered to be the most likely diagnosis, given the history and imaging findings. The differential diagnosis included other primary brain tumors, cerebral abscess or infection, and demyelinating diseases.
2. What is the appropriate diagnostic evaluation for a patient with suspected CNS lymphoma?
- Imaging of the brain, followed immediately by biopsy
- Imaging of the brain, lumbar puncture, and biopsy
- Imaging of the brain, ophthalmologic exam, and biopsy
- CT scan of the chest, abdomen, and pelvis; magnetic resonance imaging (MRI) of the brain and spinal cord; lumbar puncture; and biopsy
- MRI brain; biopsy; if positive, CT scan of the chest, abdomen, and pelvis, lumbar puncture (unless already done preoperatively), ophthalmologic exam, serum lactate dehydrogenase, human immunodeficiency virus (HIV) testing, bone marrow biopsy, and aspiration
The International Primary CNS Lymphoma Collaborative Group (IPCG) has published consensus guidelines for the diagnostic evaluation of patients with suspected primary CNS lymphoma. Patients should undergo a comprehensive physical exam, with particular attention to lymph nodes in all patients and testes in older men, and a comprehensive neurologic exam, including evaluation of cognitive function. A dilated fundoscopic exam should be performed to exclude ocular involvement.
Serum tests should include lactate dehydrogenase, as an elevated level has prognostic implications, as well as the determination of adequate hepatic and renal function (in anticipation of treatment with high-dose methotrexate (MTX) therapy), and HIV testing, as there is an increased risk of PCNSL in this population and HIV status may have an impact on choice of therapy.
Imaging should include gadolinium-enhanced MRI of the brain parenchyma; a contrast-enhanced CT scan can be substituted in patients with a contraindication to MRI. PCNSL in the immunocompetent host typically appears as a single, homogeneously enhancing mass lesion adjacent to the ventricular system. Infiltrative growth along the course of the white matter tract is characteristic. Due to their high cellularity, the tumor masses display restriction of water diffusion, have an iso- to hypointense signal on T2-weighted sequences, and are hyperdense on CT. Premature use of corticosteroids can profoundly alter the tumor’s imaging characteristics. In the immunodeficient host, PCNSL is more often multifocal and the lesions are rim enhancing. A gadolinium-enhanced MRI of the spine is only required in patients demonstrating spinal symptoms, as involvement of the spinal cord parenchyma is rare. Complete systemic staging to exclude occult systemic disease includes a CT scan of the chest, abdomen, and pelvis; a bone marrow biopsy with aspirate; and testicular ultrasound in older men to exclude an occult testicular lymphoma. An 18-fluorodeoxyglucose positron emission tomography (PET) scan increases diagnostic sensitivity but is generally not required.
A lumbar puncture should be performed unless prohibited by increased intracranial pressure and brain herniation. Cerebrospinal fluid (CSF) studies should include cell count, glucose, protein, cytomorphological examination, flow cytometry, as well as immunoglobulin heavy-chain (IgH) and T-cell receptor (TCR) gene rearrangement analysis.
Following admission to the hospital, dexamethasone was discontinued as CNS lymphoma was considered in the differential diagnosis. He underwent an MRI of the brain, which again demonstrated homogeneously enhancing mass lesions in the right frontal lobe (see Figure 48.2). There was no leptomeningeal thickening or enhancement. A CT scan of the chest, abdomen, and pelvis was unremarkable. Lumbar puncture was deferred, given the mass effect visualized on the MRI of the brain. A dilated fundoscopic exam was performed, and no retinal lesions or vitreal cells were seen. Serologic testing for HIV was negative, lactate dehydrogenase was elevated at 264 U/L, liver function tests were within normal limits, and creatinine was 1.1 mg/dL.
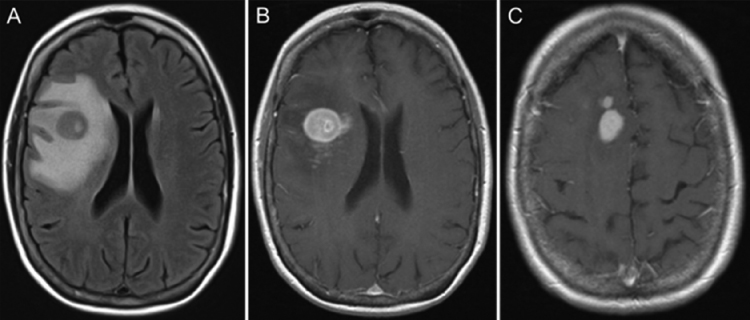 Figure 48.2 The mass lesions are hypointense on fluid attenuated inversion recovery (FLAIR) images (A) and homogeneously enhancing on T1-weighted images after administration of gadolinium (B and C). Surrounding vasogenic edema is hyperintense on FLAIR and hypointense on T1.
Figure 48.2 The mass lesions are hypointense on fluid attenuated inversion recovery (FLAIR) images (A) and homogeneously enhancing on T1-weighted images after administration of gadolinium (B and C). Surrounding vasogenic edema is hyperintense on FLAIR and hypointense on T1.
3. What is the role of surgery in the management of CNS lymphoma?
- Gross total resection of mass lesions if possible
- Diagnostic biopsy only
- Diagnostic biopsy; debulking in the rare case of imminent herniation
- There is no role for surgery
PCNSL is typically diagnosed via a stereotactic biopsy of a brain parenchymal lesion. Rarely, it may be diagnosed with meningeal biopsy or through CSF analysis. Gross total surgical resection does not play a therapeutic role in PCNSL, as the disease is often multifocal, is diffusely infiltrative, and may disseminate to the CSF or eyes. A large meta-analysis found no correlation between extent of resection and overall survival (OS). Furthermore, large resections may result in treatment delays and carry the risk of neurologic deficits. More extensive surgery should be reserved for cases at risk of perioperative herniation.
4. What is the sensitivity of a cerebral biopsy in a patient who has recently received corticosteroids?
- Corticosteroids do not affect the results of a cerebral biopsy
- There is a greater risk of a false-negative result
- The biopsy will be nondiagnostic
Corticosteroids cause rapid apoptosis of lymphocytes, disrupting the cellular morphology of the tumor and normalizing imaging, but the tumor cannot be viewed as cured. Steroid therapy can lead to a false-negative biopsy result, as the tissue may appear diffusely necrotic or merely inflammatory with T-cell predominance. A recent retrospective analysis suggested that corticosteroid administration prior to biopsy does not have a major impact on diagnostic yield. It is currently recommended to hold corticosteroids in a patient with suspected PCNSL until after a biopsy is performed. Mannitol can be used to induce osmotic diuresis in patients with signs and symptoms of elevated intracranial pressure.
Cerebral biopsy confirmed a diagnosis of CNS lymphoma (see Figure 48.3). Pathologic findings included infiltration of numerous large CD20-positive and mitotically active lymphoid cells with prominent nucleoli, intermixed with abundant CD3+ T cells. A bone marrow biopsy was performed, without evidence of a lymphoproliferative disorder. Testicular ultrasound demonstrated no abnormalities. A 24-h urine collection was performed, and creatinine clearance was found to be 102 ml/min. A treatment plan was devised.
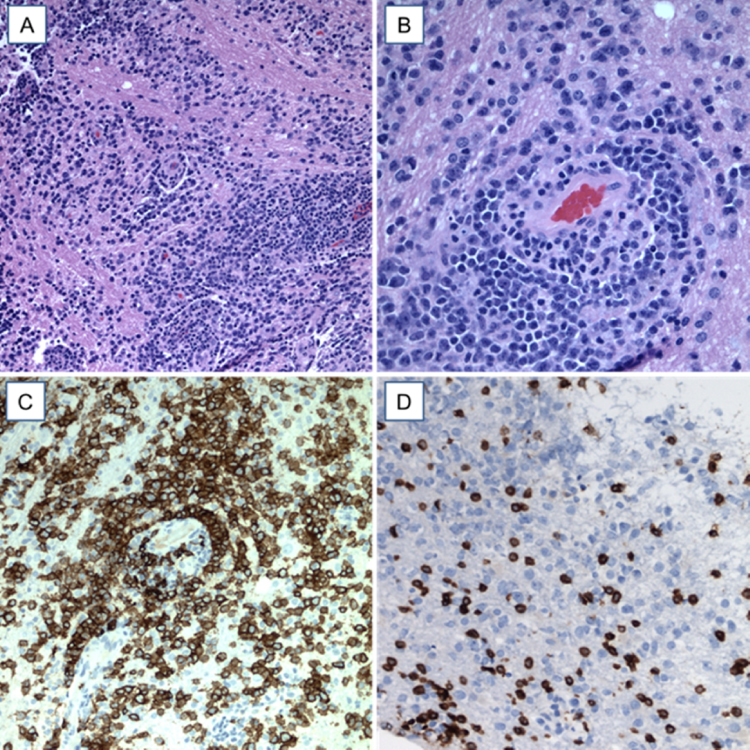 Figure 48.3 (A) Hematoxylin and eosin stain shows a mononuclear cerebral parenchymal cell infiltrate. (B) At higher-power magnification, the angiocentric arrangement of tumor cells is highlighted. (C) Immunohistochemistry using an anti-CD20 antibody identifies the large atypical cells within the infiltrate as B-cells. (D) A CD3-stain shows a reactive T-cellular infiltrate. (Color plate 48.1)
Figure 48.3 (A) Hematoxylin and eosin stain shows a mononuclear cerebral parenchymal cell infiltrate. (B) At higher-power magnification, the angiocentric arrangement of tumor cells is highlighted. (C) Immunohistochemistry using an anti-CD20 antibody identifies the large atypical cells within the infiltrate as B-cells. (D) A CD3-stain shows a reactive T-cellular infiltrate. (Color plate 48.1)
5. What is the current standard of care for initial treatment of primary CNS lymphoma?
< div class='tao-gold-member'>



