CASE 40
Bill has cystic fibrosis and received a double-lung transplant approximately 8 months ago. When you see him in your follow-up clinic today he looks far more short of breath than on his last appearance. Your nurse measures his oxygen saturation at rest on room air (normal, nonsmoker: 97%-100%), and you are disturbed to find his level only 88%. He becomes quite cyanotic (low oxygen supply to peripheral tissues) with minimal exertion in your office. He has diffuse wheezes throughout the lung fields and is afebrile. There has been no recent change in immunosuppressive therapy. You admit him to a hospital for further investigation.
QUESTIONS FOR GROUP DISCUSSION
1. What is the genetic defect in cystic fibrosis? To what types of infections are these patients particularly prone?
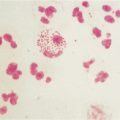
2. Explain why patients with cystic fibrosis are prone to infection with Staphylococcus aureus and Pseudomonas aeruginosa.
3. One of the first considerations in a patient with a relatively recent transplant is acute rejection. However, evidence of acute rejection typically occurs in the first 2 months, and so one would have expected some earlier indication that this was occurring. What is the accepted therapy for a patient who is undergoing acute rejection of the transplanted tissue? (See Introduction to Transplantation and Case 42.)
4. This patient had received a double-lung transplant (instead of a single lung). This is a generally accepted procedure for patients with cystic fibrosis. Explain.
5. What is your primary concern in a patient who is immunosuppressed? Explain why immunosuppressive therapy would predispose an individual to viral and fungal infections, in particular.
6. To which viral infections are immunosuppressed patients particularly prone? Describe the immunoevasive strategies that are protective for these viruses and explain why they hinder destruction of the virally infected cells.
7. The wheezing probably reflects generalized airway irritation/hyperreactivity and not a type I hypersensitivity reaction in that no change in medication is reported. Type I hypersensitivity reactions are associated with the production of IgE, mast cell degranulation, histamine and leukotriene release, and eosinophilia. As a review, discuss the mechanisms by which each of these occurs with emphasis on the role of interleukin (IL)-4 and IL-5.
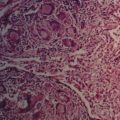
8. A bronchoscopy sample of this patient’s lung revealed a chronic inflammatory/fibrosing picture referred to as bronchiolitis obliterans (loss of small airways and chronic graft loss). Explain why increasing immunosuppressants would not help this patient yet would help a patient experiencing acute rejection. (Bronchoscopy is a diagnostic technique in which a tiny camera, within a tube, is inserted into the lungs via the nose or mouth. In addition to generating a “picture” of the airways, it is possible to obtain samples of the lung tissue and secretions.) (See Introduction to Transplantation and Case 42.)
9. Treatment measures are still in their infancy, among which is the administration of IL-10 in aerosolized fashion. Explain the rationale for this approach. Include in your discussion each of the following: antigen-presenting cells; natural killer (NK) cells; Thp, Th0, and Th1 cells; and type 1 cytokines.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree