Chronic Myeloid Leukemia: Chronic Phase
Fred Hutchinson Cancer Research Center, Seattle, WA, USA
Introduction
Tyrosine kinase inhibitors (TKIs) have irrevocably changed the care of chronic myeloid leukemia (CML) patients, dramatically changing the natural history of this disease. With multiple TKIs available, we now have an “embarrassment of riches” in treatment options. Below are some common questions and clinically relevant answers for patients with chronic-phase CML.
Multiple Choice and Discussion Questions
1. Is there one best TKI that is preferred over others for patients with chronic-phase CML?
The choices are imatinib, and the more potent second-generation TKIs nilotinib and dasatinib. Here are some basic considerations for selection of therapy: (i) What are the treatment goals? For instance, for someone in their 70s, it may be appropriate to extend survival without concerns of potential serious toxicities. For someone much younger, it may be appropriate to achieve “deeper responses” with counseling about the management of concurrent, manageable side effects in order to allow discontinuation of a particular TKI (see question 4, this chapter). (ii) Conduct an avid evaluation of preexisting comorbidities. It may not be best to prescribe dasatinib or nilotinib, respectively, to a patient with cardiopulmonary problems or vascular disease, given the emerging evidence of pulmonary hypertension and peripheral vascular occlusion, respectively, associated with these medications. (iii) Another important consideration is as follows: is the chronic-phase disease status at the time of diagnosis a low or high Sokal (or Hasford) risk? If the patient seems to be on the verge of transition to an accelerated or blast phase, there may be a reason to start therapy with a more potent TKI. (iv) The personal experience and comfort level of a physician in managing various side effects of specific TKIs remain crucial in the decision-making process (Table 21.1).
Table 21.1 Some consideration for the selection of tyrosine kinase inhibitor (TKI) therapy in chronic myeloid leukemia.
| TKI | Advantage | Disadvantage |
|---|---|---|
| Imatinib | Long-term data available Less expensive | Lower rates of complete cytogenetic remission (CCyR) compared to second-generation TKIs Fluid retention Musculoskeletal aches and pains |
| Dasatinib |
| Pleural effusion Pulmonary arterial hypertension Thrombocytopenia Hemorrhage |
| Nilotinib | >10% higher CCyR compared to Imatinib ∼2× higher rates of MMR | Cumbersome dosing schedule Skin rash Pancreatitis QT prolongation Dyslipidemia or hyperglycemia Peripheral arterial disease |
All things being equal, the second-generation TKIs do yield superior progression-free survival (PFS) compared to imatinib. Three separate randomized trials showed that nilotinib or dasatinib yielded more frequent complete cytogenetic remissions (CCyRs) and major molecular responses (MMRs) by 12 months, as well as fewer progressions to the accelerated or blast phase, compared to imatinib (1–3). To date, however, no randomized trial has shown a benefit in overall survival (OS) of nilotinib or dasatinib over imatinib.
2. In the modern era, what are the strengths and weaknesses of the Sokal, Hasford, and Euro scores?
Table 21.2 displays the variables used in these clinical scores. The Sokal score was created to predict the natural history of CML in the era of hydroxyurea and busulfan therapy; Hasford was based on the experience of patients treated with interferon; and the Euro score is based on modern experience with TKI therapy. Because we do not ever know how long patients have had CML prior to their diagnosis, the scores are a rough measure of time of Bcr–Abl exposure [since, e.g., the spleen size and white blood cell count presumably were normal at the time the patient acquired the Philadelphia (Ph) chromosome]. All of these scores are effective at predicting the behavior of CML and the response to therapy. Predictably, patients with low-risk scores do best with TKIs, whereas patients with high-risk disease have worse achievement of treatment milestones.
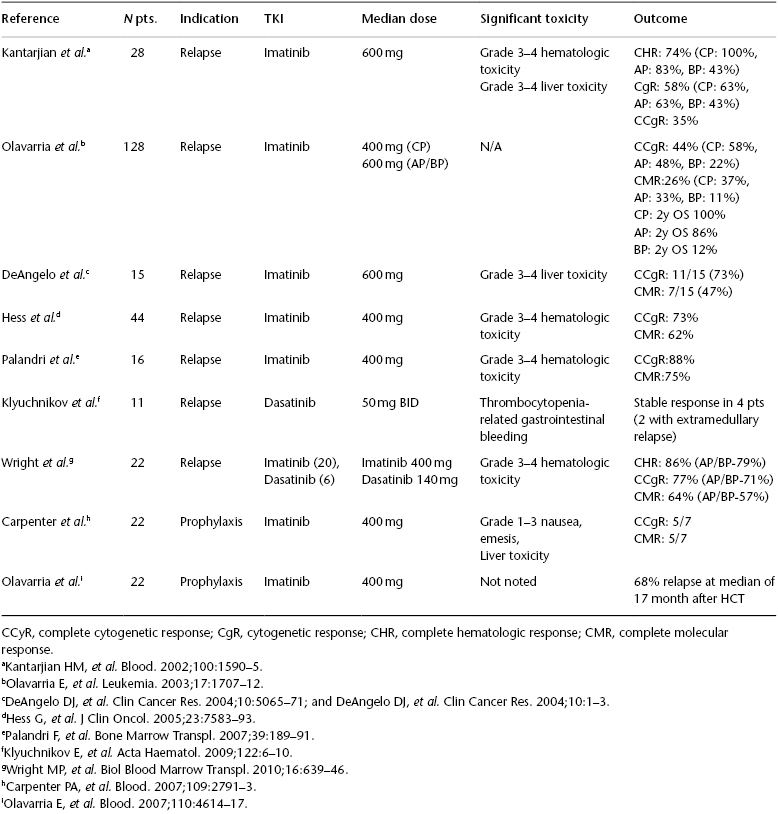
Table 21.2 Posttransplant use of tyrosine kinase inhibitors (TKIs) in patients with chronic myeloid leukemia (CML) (adapted from Bar M, et al. J Natl Comp Cancer Network. 2013;11(3):308–15).
3. Peripheral blood– and bone marrow aspirate–retrieved cytogenetic and molecular studies provide unusually concordant results in the majority of patients. Can they preclude the need for bone marrow biopsy every 3 months?
- Yes
- No
Peripheral blood monitoring of the Bcr–Abl transcript is a sensitive and accurate method of following disease burden in CML. The peripheral blood value correlates well with bone marrow Bcr–Abl testing, as well as cytogenetic chromosomal karyotyping. Bone marrow chromosomal testing is important at diagnosis, because it is needed to identify both the Ph chromosome and other cytogenetic changes that would change the diagnosis to the accelerated phase. However, once therapy is initiated, National Comprehensive Cancer Network (NCCN) guidelines call for q3 month peripheral blood polymerase chain reaction (PCR) testing alone, with bone marrow reserved for cases that do not meet treatment milestones or have evidence of relapse.
4. How hard should we push for an MMR?






