Abstract
Once an outbreak starts, it is important to quantify how a disease is spreading, how it is affecting the population, and how different public health measures will have an impact on its effects. Epidemiology is the study of how a disease is distributed in a population, and of the different factors that determine this distribution. These studies can help to quantify the main population factors that led to the introduction and spread of an infectious disease in the population and the conditions that are associated with the severity of the disease. Epidemiology can also be used to assess the current extent of the disease and the effectiveness of different interventions, including different therapies and public health measures. Finally, it can also help to make predictions on likely future scenarios, given the current assessment of the situation and the different measures taken.
Once an outbreak starts, it is important to quantify how a disease is spreading, how it is affecting the population, and how different public health measures will have an impact on its effects. Epidemiology is the study of how a disease is distributed in a population, and of the different factors that determine this distribution. These studies can help to quantify the main population factors that led to the introduction and spread of an infectious disease in the population and the conditions that are associated with the severity of the disease. Epidemiology can also be used to assess the current extent of the disease and the effectiveness of different interventions, including different therapies and public health measures. Finally, it can also help to make predictions on likely future scenarios, given the current assessment of the situation and the different measures taken.
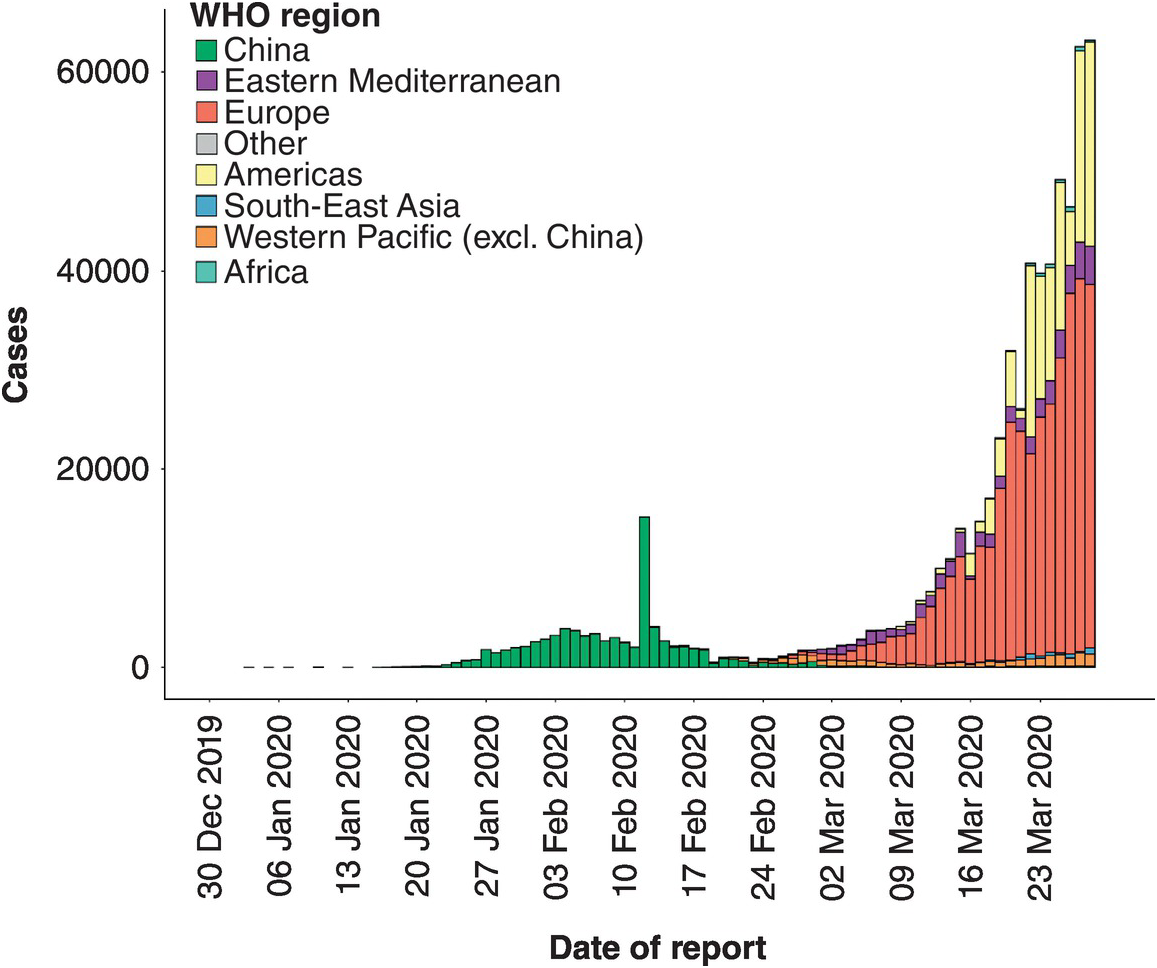
In the first few months of the COVID-19 pandemic we have witnessed an exponential increase in the number of cases and deaths. The implementation of different containment measures in different parts of the world has led to vastly different outcomes. Whereas in some Asian countries early containment measures were able to stop the infections, in many other places the growing number of cases made containment unfeasible, forcing a change to mitigation strategies to reduce the impact on the healthcare system and the number of fatalities associated with lack of adequate care (Figure 2.1). For the current COVID-19 outbreak, we would like to quantify what conditions enabled the emergence of the disease, how fast the disease is spreading in the human population, how deadly it is, the different factors that affect disease severity, how effective the current public health measures are, and the possible future scenarios of the pandemic.
Figure 2.1 The number of confirmed COVID-19 cases reported to the World Health Organization (WHO) from the beginning of the pandemic at the end of December 2019 until March 29, 2020 by different regions of the world. The green bars represent the cases reported to the WHO at the beginning of the pandemic, with the vast majority of cases from Wuhan in Hubei province in China. The outbreak in China was rapidly controlled by imposing a lockdown of the region and strong confinement measures. The total number of deaths in Hubei attributed to the virus during this period was estimated to be over 3000. The number of cases in other regions of the world remain very low until the beginning of March 2020, when an exponentially growing number of infections were identified in Europe and the USA. The number of deaths in Europe and the USA follow suit.
How Long Does It Take to Have Symptoms?
The incubation period is the time from infection to the onset of the disease – that is, the appearance of the first symptoms. This is an important concept, because this period can vary according to the disease and the person. During the incubation period, there are no symptoms, and it is hard to assess whether a person is infectious or will become sick.
A well-known measure against infectious diseases is so-called quarantine. Where does this term come from? In the 1300s, Europe was ravaged by the plague. In order to prevent the disease from entering a city, all boats were required to anchor for 40 days. These 40 days were considered a safe time to assess whether anyone aboard presented the symptoms of the plague. These 40 days, or quaranta giorni, is where the word quarantine comes from. A person will become ill 2–6 days after being infected with the bubonic plague, but it takes almost 40 days from infection to death.
The incubation period varies dramatically across different infectious diseases. The incubation period for influenza, for instance, is a couple of days. For the common cold, it is about four days. However, the incubation period for rabies in humans can be 1–2 months. In the COVID-19 outbreak the incubation period has been estimated to be five days, similar to SARS. However, a few rare cases have been reported in which this incubation period has been more than two weeks. Measures of isolation, as with the original quarantine, should take into consideration these longer incubation periods.
How Many People Will the Virus Infect?
The attack rate is the number of people developing a disease or infected with an infectious agent divided by the total of number of people susceptible to the disease. These rates are usually estimated from all cases from the beginning to the end of the epidemic. In an ongoing epidemic, the rate cannot be measured, but it can be estimated through modeling. In the case of a new infectious agent in the population, such as SARS-CoV-2, everyone is susceptible, and the attack rate is the fraction of the population that has been infected with the virus. The attack rate will depend on many factors, including how quickly the infectious disease spreads, and what measures can be taken to avoid its spread.
In the first influenza pandemic of the twentieth century, the Spanish Influenza, it was estimated that one-third of the global population was infected with the virus. In an ongoing outbreak, it is hard to estimate the fraction of the population that will become infected. It will depend on how fast the infectious agent spreads and how effective the measures taken to control its spread are.
How Quickly Does the Virus Spread in the Population?
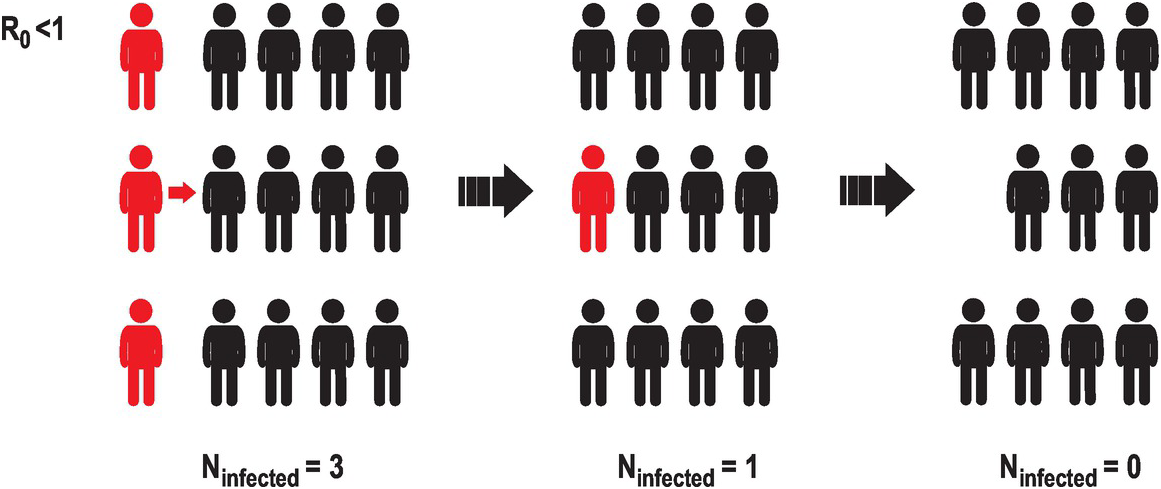
One way of quantifying the infectiousness of a pathogen is the basic reproduction number (R0), which is the estimated number of new infections per infected individual. If this number is smaller than 1, meaning that a person rarely infects another person, the number of infected individuals in the population will decrease with time, until the infectious agent will not be able to propagate (Figure 2.2).
Figure 2.2 A representation of the evolution of an infectious agent with low basic reproduction number or R0. A way to estimate how fast an infectious disease is spreading is to estimate the mean number of infections caused by a single infected individual. This illustration represents a case in which a few infected individuals (three in this case, represented in red) interact with uninfected individuals (in black). If the basic reproduction number is smaller than 1, the number of new infections diminishes. Eventually the infectious agent will disappear from the population.
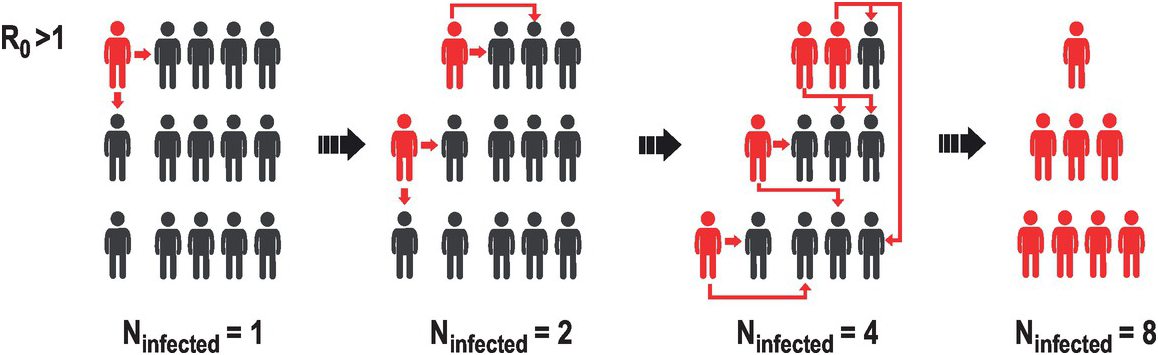
But if the basic reproduction number is greater than 1, the number of infections will grow exponentially. For instance, imagine that an infectious agent has a basic reproduction number of 2. This means that a single infected individual will infect, on average, another two people (Figure 2.3). These two newly infected people could then infect another two each, resulting in four newly infected people. And so on. If these new infections occur five days after the previous infection, then in a 30-day month, there are six five-day periods, and a single person can lead to 2 × 2 × 2 × 2 × 2 × 2 = 64 new infections – and in two months that’s 4096 new infections. By six months, the entire world population will have been infected. This type of growth is called exponential and characterizes the initial growth of infections in an uncontrolled setting. Under exponential growth, the number of cases can increase very quickly (Figure 2.4). Exponential growth nicely illustrates the idea that early interventions are important. For instance, if by social distancing we can reduce the mean number of contacts by 50%, the number of new infections will be reduced to only one. In the first case, thousands of new infections could saturate a hospital, while in the second they can be monitored and contained. This is an example of how social distancing and social responsibility can generate large effects in the course of an infection. Of course, the growth of these numbers will depend on the number of individuals who are susceptible, and the contact between infected and non-infected individuals. Strong quarantine measures can reduce the basic reproductive number to less than 1.
Figure 2.3 A representation of the evolution of an infectious agent with high basic reproduction number or R0. We present a case in which an infectious agent has an estimated R0 bigger than 1. In such a case, a single infected person can infect several others, and in successive infections this number can increase exponentially. R0 depends very much on the infectious agent. The R0 of SARS-CoV-2 is estimated to be 2–3, indicating that the number of infective cases will increase exponentially in the first months of the outbreak.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree