Member
Affiliation
Specialty and APS expertise
North America a
Mary-Carmen Amigo
ABC Medical Center, Mexico City, Mexico
Rheumatology
Damage/risk assessment, cardiac APS
Medha Barbhaiya
Brigham and Women’s Hospital, Boston, USA
Rheumatology, epidemiology
Database management
Ware Branch
University of Utah, Salt Lake City, USA
Maternal and fetal medicine
Obstetric APS
Karen Costenbader
Brigham and Women’s Hospital, Boston, USA
Rheumatology, epidemiology
Classification criteria development
Michael D. Lockshin
Ray Naden
Hospital For Special Surgery, New York, USA
McMaster University,
Hamilton, Ontario, Canada
Rheumatology
Definition, treatment, obstetric APS
Obstetrical Medicine
1000Minds software, classification criteria development
Rohan Willis
University of Texas, Galveston, USA
ImmunologyaPL assays, mechanisms
Europe b
Tadej Avcin
Ljubljana University Medical Centre, Slovenia
Pediatric rheumatology
Pediatric APS, database management
Maria Laura Bertolaccini, MD
St Thomas Hospital, London, United Kingdom
Immunology
aPL assays, mechanisms
Philip G. de Groot
University Medical Centre, Utrecht, Netherlands
Biochemistry
Mechanisms, aPL-related proteins
Francis Guillemin
Lorraine University, Nancy, France
Rheumatology, epidemiology
Outcome measurement
Maria Tektonidou
University of Athens, Athens, Greece
Rheumatology
Renal APS
Denis Wahl
Lorraine University, Nancy, France
Vascular medicine, epidemiology
Meta-analysis
South America
Mirhelen de Abreu
Federal University, Rio de Janeiro, Brazil
Rheumatology, epidemiology
Decision-making
Guilherme de Jesus
State University, Rio de Janeiro, Brazil
Maternal and fetal medicine
Obstetric APS
Roger Levy
State University, Rio de Janeiro, Brazil
Rheumatology
Treatment, SLE-associated APS
Needs Assessment Survey
The task force chairs designed a 14-question needs assessment survey, emailed to 13 members in August 2014. The survey response rate was 100%; responses were analyzed anonymously in a descriptive fashion that revealed consensus regarding the need for new APS Classification Criteria [28]. Ninety-two percent of those queried reported the need for new APS Classification Criteria; 100% agreed that all disease domains are not sampled by current criteria; 85% reported scenarios in which current criteria disagree with expert diagnoses, for instance, “non-criteria” manifestations only with or without aPL, non-criteria obstetrical findings with aPL, and high suspicion for APS in patients without persistent or low titer aPL; and 62% agreed that other aPL tests should be considered. Thus, the task force decided to proceed with efforts to prepare new classification criteria.
Meta-Analysis of Different Antiphospholipid Antibody-Related Manifestations
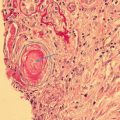
Under the leadership of Dr. Stephane Zuily, four different teams have been working on the meta-analyses of the selected non-criteria manifestations of aPL, i.e., livedo reticularis, thrombocytopenia, hemolytic anemia, and aPL nephropathy [38–41]. These four meta-analyses, together with others [33–35, 42–45], will guide physician-scientists during the new classification criteria development efforts.
Special Sessions Organized by the Task Force
During the 2014–2016 ACR Annual Scientific Meetings , as part of a study group, our classification criteria update efforts have been presented to other task force members, APS researchers, and interested physicians. These sessions share our plans with others and demonstrate inclusiveness. The results of the needs assessment survey were presented at the ACR Annual Scientific Meeting and discussed in detail with worldwide physicians interested in APS. During the 15th International Congress on aPL (www.apsistanbul2016.org), the task force organized a session together with the Scientific Planning Committee of the congress; discussions included the historical aspects, limitations, and strengths of the Sapporo Classification Criteria, the methodology to develop classification criteria, and the accomplishments and future plans of the task force.
Completion of Phase I Item Generation
During phase I, our goal was to identify candidate criteria for the new classification criteria [46–48]. Fifty-four physician-scientists from our master list were asked three questions via e-mail:
- 1.
“Describe all features (historical, clinical, laboratory, radiological, and pathological) that, in your experience, occur as part of the aPL/APS spectrum.” This question allowed us to identify candidate criteria with potential positive weight.
- 2.
“Describe all features (historical, clinical, laboratory, radiological, and pathological) or concomitant diseases that, if present, would make you question the diagnosis of APS even if aPL tests are positive.” This question allowed us to identify criteria with potential negative weight.
- 3.
“When you consider the diagnosis of APS, do you think of APS patients in different subpopulations?” This question allowed us to group the criteria.
We encouraged respondents to consider their real-life experiences with aPL-positive patients, rather than focusing on current APS Classification Criteria. Responses were systematically clustered by the task force members by organ system to avoid duplication and for ease of interpretability.
The phase I response rate was 76% (41/54 respondents), of whom 18 were rheumatologists, five clinical immunologists, five hematologists, five nephrologists/cardiologists/neurologists, four internists, two pediatric rheumatologists, and two obstetricians. One hundred and fifty-two candidate criteria, displayed by organ systems, were generated (Table 15.2, laboratory variables and family history are also included). The distribution of non-obstetrical candidate criteria with potential negative weight generated is shown in Table 15.3. Additional obstetrical candidate criteria with potential negative weight were late reproductive age, early/very early (recurrent) miscarriage, normal placental pathology, and concomitant causes of recurrent miscarriage, such as uterine/cervical abnormality, thyroid diseases, or genetic abnormalities. The reported subpopulations of APS patients, grouped based on age, clinical manifestations, aPL profile, and risk level, are shown in Table 15.4.
Table 15.2
Distribution of 152 candidate criteria by organ system
Organ system | Number of variablesa |
|---|---|
Neurologic | 25 (4) |
Laboratory (aPL) | 23 (12) |
Obstetric | 16 (4) |
Dermatologic | 15 |
Renal | 12 (2) |
Vascular | 10 (5) |
Cardiac | 9 (2) |
Laboratory (non-aPL) | 9 |
Other | 7 |
Hematologic | 5 (2) |
Pulmonary | 5 (1) |
Gastrointestinal | 4 |
Musculoskeletal | 4 |
Endocrinologic | 3 |
Ophthalmologic | 2 |
Auditory | 2 |
Family history | 1 (1) |
Table 15.3
Distribution of candidate criteria with potential negative weight (clustered) (number of responders in parenthesis)
Candidate criteria clustered | Selected responses |
|---|---|
Traditional CVD risk factors (n:12) | Significant atherosclerosis |
Infections (n:15)
Stay updated, free articles. Join our Telegram channel
Full access? Get Clinical Tree
 Get Clinical Tree app for offline access
Get Clinical Tree app for offline access

|