PET Scan in Oncology
Massachusetts General Hospital, Boston, MA, USA
1. My patient’s PET–CT had to be rescheduled because his blood glucose was too high. Is it really necessary to reschedule?
Fluoro-deoxyglucose (FDG) is an analog of glucose that is taken up by metabolically active cells using facilitated transport similar to that used by glucose. The rate of uptake of FDG by the cells is proportional to their metabolic activity. Similar to glucose, it undergoes phosphorylation to form FDG–6-phosphate; however, unlike glucose, it does not undergo further metabolism, thereby becoming trapped in metabolically active cells. Good control of blood glucose is required because the uptake of FDG into cells is competitively inhibited by glucose, as they use a common transport mechanism for facilitated transport into both normal and tumor cells.
Furthermore, the administration of insulin for glucose control in diabetes can exaggerate physiologic uptake in muscles (Figure 131.1). Patients are also instructed to avoid any strenuous activity prior to the examination and to lie still following injection of the radioisotope to avoid physiologic muscle uptake of FDG. Exaggerated physiologic muscular FDG uptake limits the amount of FDG available for uptake in the tumor and therefore reduces the sensitivity of the exam.

Other agents interfering with FDG uptake to be aware of include granulocyte colony-stimulating factor, which causes increased marrow and splenic FDG uptake, and metformin, which causes increased colonic FDG uptake.
2. Should a diagnostic computed tomography (CT) be performed as part of the positron emission tomography (PET)–CT, or would the low-dose attenuation correction CT suffice?
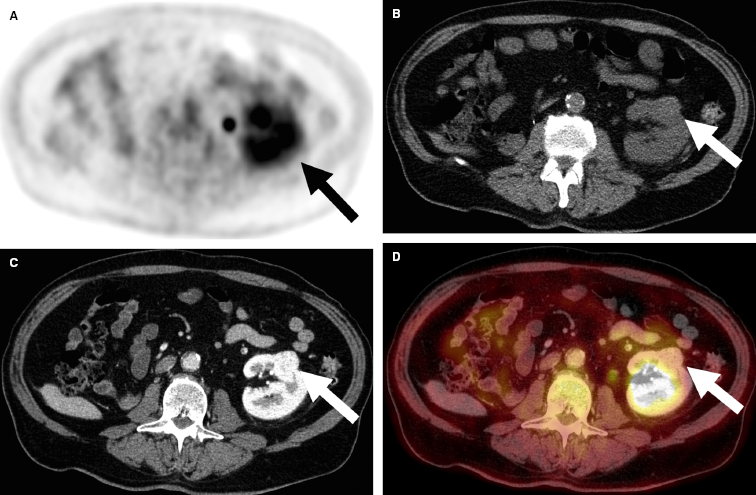
We routinely perform a diagnostic CT with both oral and intravenous contrast as part of our PET–CT protocol. The advantages of administrating intravenous contrast includes (A) increased conspicuity and characterization of lesions, which is of particular importance in lesions in which FDG does not accumulate (Figure 131.2); (B) providing additional information, which can help differentiate benign from malignant lesions that have nonspecific FDG uptake; (C) providing lesions’ vascular relationships important for preoperative planning; and (D) helping to precisely localize lesions that have increased FDG uptake that would not be clearly seen on unenhanced CT because of the absence of contour abnormality or similar attenuation to the surrounding structures. These advantages are particularly helpful in the liver, but some investigators propose that following the initial staging, a lower radiation dose of non-contrast-enhanced CT may be sufficient to follow patients with treated lymphoma who have a low clinical suspicion for recurrence.
The addition of oral contrast can aid in the evaluation of FDG uptake in the bowel. Physiologic bowel uptake is known to be highly variable and range from diffuse low-level uptake to heterogeneous and multifocal uptake. The use of oral contrast can aid in the evaluation of gastrointestinal FDG uptake because distending these segments can allow more confident exclusion or diagnosis of luminal or mural disease. Either negative oral contrast or low-density barium sulphate (LDB) is suitable as LDB does not induce increased FDG bowel activity.
3. How is response determined on PET–CT?
There are two basic approaches for assessing the metabolic changes of treatment: qualitative or quantitative. Most PET–CT scans in clinical practice are typically interpreted using qualitative methods in which the intensity of 18F-FDG uptake in potential tumor foci are compared to blood pool or tracer uptake in nearby normal structures.
The potential to detect small changes in tumor glucose metabolism quantitatively is appealing, especially in clinical trials. The standard uptake value (SUV), defined as 18F-FDG retention normalized to injected dose and patient body weight, is an established index for quantifying glucose metabolic activity in tissues. The determination of SUV is dependent on identical patient preparation and on adequate scan quality that is similar between the baseline and follow-up studies. Ideally, the scans should be performed on the same scanner with comparable injected doses of 18F-FDG and with comparable uptake times before scanning. Although some studies have demonstrated that SUV measurements are highly reproducible, other studies have found a higher variance of SUV measurements. A meta-analysis found that SUVmean had better repeatability performance than SUVmax, and that both measures showed poor repeatability for lesions with low 18F-FDG uptake. Attempts at greater standardization are ongoing and are being supported by various societies involved in PET scanning, but it is important to be aware of the current potential pitfalls of SUV measurements.
4. A 68-year-old man 8 months after Whipple procedure for ampullary cancer has developed an FDG-avid soft tissue mass within the postoperative bed. Could this be anything other than recurrence?
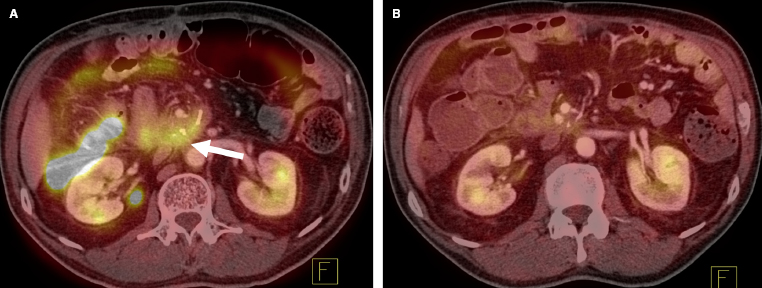
FDG uptake can also occur as a result of granulomatous disease, postsurgical changes, abscess, or inflammation (Figure 131.3). An ongoing bowel leak may simulate recurrent disease. Acute radiation changes can also lead to increased FDG uptake in its field. Several cytotoxic chemotherapy agents, such as 5FU plus leucovorin, can cause enteritis that will show FDG uptake. The CT component of the PET–CT study can often help identify hypermetabolic nonneoplastic conditions, thereby reducing false-positive interpretations. Some benign tumors can also demonstrate intense FDG uptake (Figure 131.4), and their features can sometimes be recognized by CT.

5. A lesion seen on CT is not FDG-avid. Does this mean it is benign?