Definitions
Discharge planning is the process by which the hospital team, liaising with relatives and carers, community services and general practitioners, organises the return of patients to their homes or transfer to other places of care. It is often a multidisciplinary process, which ensures that patients spend no unnecessary time in hospital. Some discharges can be time-consuming and complex. The keys to a successful discharge are information gathering, sharing this information, and planning (Box 13.1). Every detail needs to be considered, especially if the patient has several different problems.
The discharge planning process
Discharge planning starts on admission, by collecting information from the patient and relatives and/or carers about social circumstances and function. It includes a risk assessment for those who are frail or cognitively impaired, or have inadequate social support. It prepares the patient, relatives, multidisciplinary team and other healthcare providers for a safe and efficient discharge back to the pre-admission destination or suitable alternative. The stages of discharge planning are shown in Figure 13.1.
Discharge planning involves good communication:
- with the patient and relatives or carers, whose active involvement is central to the success of the discharge
- within the ward-based multidisciplinary team (e.g. at formal meetings, during ward rounds or at other times). See Figure 13.2.
- between the ward staff and members of the community team. The different members of the multidisciplinary team are shown in Box 13.2.
Box 13.1 Successful discharge planning
Successful discharge planning involves the following.
- Assessing the patient: to determine his or her medical, social, psychological and functional needs
- Discussion with the family or care givers: their ability to care for the patient, whether they are under strain, whether care services will be needed, and the carers’ educational needs are met
- Sharing information with the patient, family and other team members
- Implementation of the plan: arranging for the provision of services and equipment
- Follow-up: the evaluation stage provides feedback that enables the effectiveness of the discharge process to be measured
Figure 13.1 The stages of discharge planning.
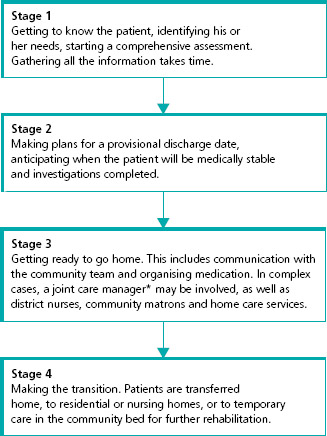
 A joint care manager is a person with a nursing or social work background who deals with people who require both health and social care in the community.
A joint care manager is a person with a nursing or social work background who deals with people who require both health and social care in the community.
Figure 13.2 A typical weekly multidisciplinary team meeting.

Comprehensive geriatric assessment
Patients identified as high risk (e.g. recurrent falls, dementia, struggling at home) should have a comprehensive geriatric assessment (see Chapter 1). In the context of discharge planning, this involves the following.
- Medical assessment and treatment.
- Review of medicines and concordance (see Chapter 2).
- Gathering information about social circumstances, including details of carers, social services, benefits and whether there is any carer strain.
- Assessment of cognitive function, including the patient’s ability to participate in discharge planning, and if not, identifying a representative.
- Assessment of functional ability (i.e. ability to perform activities of daily living and instrumental – or extended – activities of daily living which is helpful in assessing a patient’s need for rehabilitation or support – see Box 13.3).
- Asking about living arrangements (e.g. whether there are stairs at home).
- Formulating goals, which should be specific and agreed with the patient, relatives and carers.
- Eliciting patient preferences about discharge plans.
Following this, referrals may be made to social services or mental health teams. Physiotherapy and occupational therapy input may be needed. An estimation of when patients will be medically fit is made – this may include when they will be ready to go to a rehabilitation facility, if needed.
The single assessment process (SAP)
The SAP brings together health and social services information in a single document. It aims to improve communication between healthcare and social care workers, in theory allowing services to be more responsive to the patient’s needs. It avoids the patient having to repeat the same information to a range of professionals and is started in hospital if the patient does not have one already. The file follows the patient. The language used is clear and concise, avoiding jargon and abbreviations.
| Team members | Role |
| Doctors | Assess, diagnose, treat and review medical conditions A consultant geriatrician often ‘chairs’ the MDT meetings |
| Nurses |