Introduction
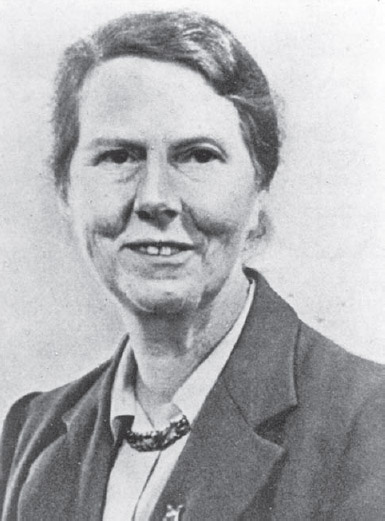
Illness in older people often has functional consequences, especially in relation to mobility and self-care. This was recognised by one of the pioneers of geriatric medicine – Marjory Warren (Figure 11.1). She took over the care of several hundred chronically sick, bedridden, ‘incurables’ in the West Middlesex Hospital in the 1930s and devised a novel programme that was patient-centred and involved multidisciplinary team working. So successful was her approach that most of these incurable patients improved sufficiently to be discharged from hospital. This was the beginning of the specialty of geriatric medicine and her novel approach would today be recognised as rehabilitation.
What is rehabilitation?
Rehabilitation is a complex intervention that aims to address the functional, psychological and social consequences of ill-health in a context that values and promotes independence. It requires a multi-disciplinary team, identifies specific individualised treatment goals, and measures progress against these goals.
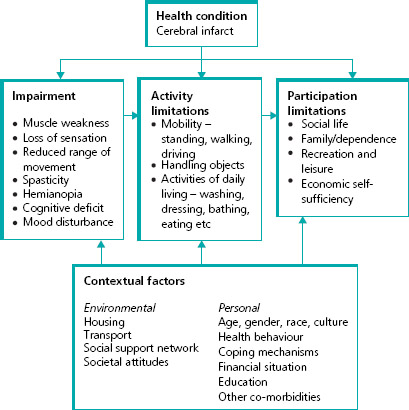
The World Health Organization (WHO) International Classification of Functioning, Disability and Heath (ICF) describes the consequences of illness and provides an important framework within which the rehabilitation process can be understood (Box 11.1). The WHO ICF framework requires a medical diagnosis (the impairments), while examining the functional consequences (activity limitations, formerly known as disability), and set in the context of the person’s daily life (participation limitations, formerly known as handicap). There is often discordance between impairments, activity limitations and participation limitations because of mediating environmental and personal factors. Figure 11.2 provides an example for a person who has a cerebral infarct affecting a parietal lobe.
Figure 11.1 Dr Marjory Warren. ‘The treatment of long-stay cases should be undertaken by a team whose central theme is optimism and hope. It is wise to get elderly folk up as soon as their physical condition warrants, and it is of great value to their morale to get them dressed in their own clothing as soon as possible.’ From Marjory Warren. Care of the chronic sick. Lancet 8 June 1946. Picture reproduced with the permission of the British Geriatrics Society.
Box 11.1 WHO International Classification of Function (1991)
- Body functions: the physiological functions of body systems (including psychological functions)
- Impairments: problems in body function or structure such as a significant deviation or loss
- Activity: the execution of a task or action by an individual
- Participation: involvement in a life situation
Figure 11.2 WHO International Classification of Function (ICF) using the example of a person with a cerebral infarct affecting a parietal lobe.
Who is rehabilitation for?
Activity limitation, or disability, is strongly related to increasing age. This reflects the increasing prevalence of common disabling conditions: stroke, arthritis, heart failure, chronic lung disease, fractured hip and peripheral vascular disease. There are around 1.3 million disabled older people in England and Wales. This is 16% of those aged over 65 years. Nearly all disabled older people, even those categorised as severely disabled, live in their own homes, but many rely on formal and informal support. Rehabilitation can improve the quality of life for these people and make them less dependent on other people. There is randomised controlled trial evidence that rehabilitation interventions can improve outcomes for older people with the following conditions:
- falls
- arthritis of the knees
- Parkinson’s disease
- stroke
- chronic lung disease
- old age and multiple conditions (frailty)
- long-term care home residents.
Who provides rehabilitation?
Rehabilitation is provided by a multidisciplinary team (MDT). Core members of this team include the following.
Nurses and support staff – enable patients to be as independent as possible, even though this is usually more time-consuming than completing tasks for them. This is facilitated by ensuring that patients are dressed and are wearing appropriate footwear, and that hearing aids, dentures and glasses are worn if needed.
Doctors – have a lead role in establishing an accurate diagnosis of the underlying and associated conditions, and in optimising their medical management.
Physiotherapists – are skilled at assessing and managing problems of muscles, movement and mobility. Key aims of physiotherapy are to improve balance, flexibility, strength and stamina, often by practising everyday activities such as walking, transferring and climbing stairs.
Occupational therapists – optimise daily living activities and may recommend the use of different aids to assist rehabilitation or maintain independence.
Speech and language therapists – assess and treat speech (e.g. dysphasia, dysarthria) and swallowing impairments.
Social workers – provide access to benefit and allowance advice, and can co-ordinate home support services.
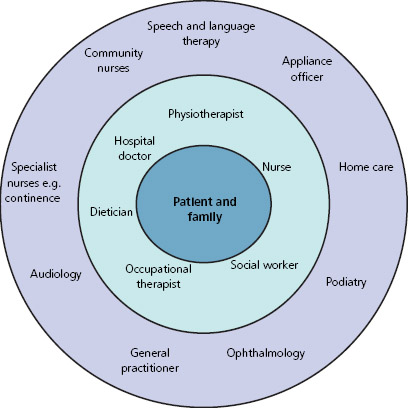
Other staff may need to be involved, depending on the specific needs of the individual patient (Figure 11.3).
Figure 11.3 Members of the multidisciplinary team.
How is rehabilitation organised?
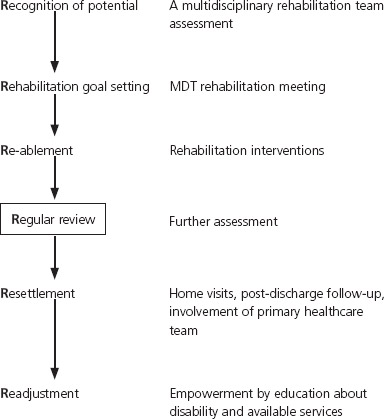
Effective rehabilitation requires several steps (Box 11.2) and requires some key functions described below. Omission of any of these key functions will jeopardise the success of the rehabilitation process.
Assessment – by each member of the MDT to identify the diseases and their consequences, best expressed in terms of impairments, activity limitations and participation limitations.
Co-ordination – each member of the MDT will have a different perspective of the issues. These need to be shared and formulated into an action plan. This is usually achieved through a regular MDT meeting.
Leadership – at the MDT meeting, someone needs to assume the role of a team leader to co-ordinate information, achieve a consensus on rehabilitation priorities and goals and agree tasks.
Communication – an important aspect of the MDT meeting is to ensure that decisions are documented and are discussed fully with the patient and close supporters.
Rehabilitation goals
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree