Atypical presentation
The following considerations, outlined in Chapter 1, are important when assessing older surgical patients. There is often:
- Multiple pathology
- Atypical presentations
- Reduced physiological reserve
- Impaired immunity
- Difficulty weighing the benefits vs risks of treatment
- Capacity or communication problems.
When older people present with an acute illness, they may have more than one acute diagnosis (e.g. intra-abdominal pathology and fast atrial fibrillation), as well as more than one chronic problem, diagnosed or otherwise.
Older people represent a high percentage of patients with acute abdominal pain. They often present late, have a disproportionately severe pathology compared with the pain they complain of, and their physical findings are less sensitive and less specific. Morbidity and mortality among older patients with abdominal pain is higher than in other age groups.
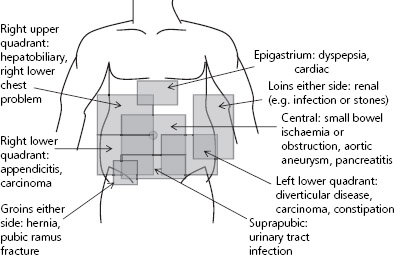
Figure 10.1 An approach to the older patient with acute abdominal pain – site of the pain. Remember that older people may have pain which is less severe than would be expected, and the site of pain may be less well localised and more diffuse than in a younger person.
Because of reduced physiological reserve and impaired immunity, symptoms and signs that one would expect to find in a younger person may be absent (e.g. tachycardia, fever, raised white cells and abdominal rigidity). Evaluating an older patient with acute abdominal pain can be difficult and an experienced surgeon should be involved early in the process.
Figures 10.1 and 10.2 describe an approach to the older patient with acute abdominal pain.
Peri-operative complications
Older people have an increased incidence of peri-operative complications, especially after emergency surgery. This is because of age-related physiological differences and reduced physiological reserve that affect all body systems (see Table 10.1). Some perioperative problems may go unrecognised because of their atypical presentation.
The care of the elderly surgical patient was highlighted in a National Confidential Enquiry into Peri-operative Death (NCEPOD) report in 1999, which looked at over 1000 patients over the age of 90. The recommendations of the report are shown in Box 10.1.
Figure 10.2 An approach to the older patient with acute abdominal pain – general strategy.
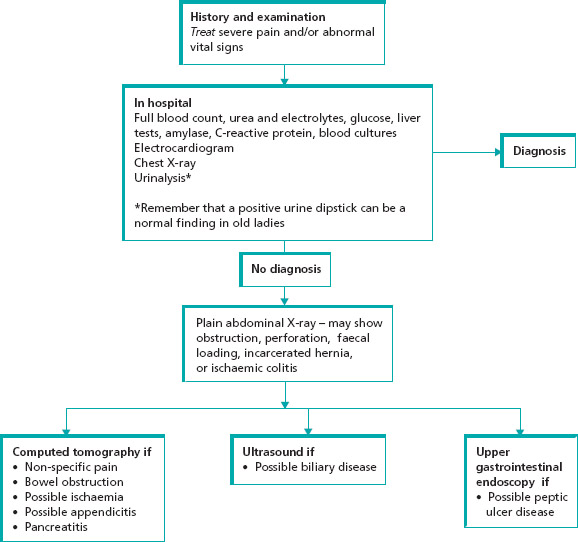
Table 10.1 Effects of ageing on physiological reserve.
| Physiological effects | Diseases that are more prevalent | |
| Cardiovascular system | ↓Cardiac output and stroke volume | Coronary artery disease |
| ↑Systemic vascular resistance | Hypertension | |
| ↓Ability to raise heart rate | Heart failure | |
| Cardiac conduction defects | Valvular heart disease | |
| Respiratory system | ↓Functional residual capacity | Chronic obstructive pulmonary disease |
| V/Q mismatch | ||
| ↓Response to hypoxia and hypercapnia | ||
| Nervous system | ↓Cerebral blood flow | Peripheral neuropathy |
| ↓Peripheral nerve function | Autonomic neuropathy | |
| Stroke | ||
| Dementia | ||
| Parkinson’s disease | ||
| Renal | ↓Renal blood flow and glomerular filtration rate | Chronic renal disease |
| ↓Renal clearance of drugs | ||
| Metabolic | ↓Body metabolism | Diabetes |
| ↓Response to hypothermia | Thyroid disease | |
| Hepatic | ↓Hepatic blood flow | |
| ↓Hepatic excretion of drugs | ||
The NCEPOD report highlighted the following areas.
Fluid management
The mismanagement of fluid prescribing was a contributory factor in many cases of post-operative morbidity and mortality. Patients were given either too little or too much fluid, with inadequate assessment and monitoring – vital in this age group.
Box 10.1 NCEPOD report ‘Extremes of Age’ 1999
Recommendations
- Fluid management in elderly patients is often poor; it should be accorded the same status as drug prescribing. Multidisciplinary reviews to develop good local working practices are required.
- A team of senior surgeons, anaesthetists and physicians needs to be closely involved in the care of elderly patients who have poor physical status and high operative risk.
- The experience of the surgeon and anaesthetist need to be matched to the physical status of the elderly patient, as well as to the technical demands of the procedure.
- If a decision is made to operate on an elderly patient then that must include a decision to provide appropriate post-operative care, which may include high dependency or intensive care support.
- There should be sufficient, fully staffed, daytime theatre and recovery facilities to ensure that no elderly patient requiring an urgent operation waits for more than 24 hours once fit for surgery. This includes weekends.
- Elderly patients need their pain management to be provided by those with appropriate specialised experience in order that they receive safe and effective pain relief.
- Surgeons need to be more aware that in older people, clinically unsuspected gastrointestinal complications are commonly found at post mortem to be the cause, or contribute to the cause, of death following surgery.
Nutrition
Early nutrition after surgery is associated with reduced mortality and length of stay in hospital. The report recommended that feeding should be started as early as possible after surgery.
DVT prophylaxis
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree