Neuropathy might also result in damage to the soft tissue of the foot because, having lost sensation, the individual is unaware of trauma to the foot. Hence people are advised not to walk around on bare feet (
Box 10.1 and
Box 10.2). Prior to the neurological assessment being undertaken it is essential what is involved is explained to the person with diabetes. It is also useful to let the person experience the perceived sensation on an area where there is no sensory loss.
Box 10.1
Foot health education for the person with healthy feet
▪ Wash feet daily, dry carefully in between the toes
▪ Apply a cream to the soles and heels
▪ Inspect feet daily for corns/callosities/plantar warts/athlete’s foot
▪ If any of the above is present, they should only be treated by a registered podiatrist
▪ With the slightest abrasion or infection in your feet, contact your GP, community nurse, diabetic nurse specialist, diabetic consultant or podiatrist
▪ Never use proprietary treatments for callus or corns, as they contain acids
▪ Cut toenails straight across
▪ Buy new shoes from a shop that measures your feet and fits the shoes for you
▪ Never wear new shoes for a long period of time
▪ Only attend a podiatrist registered by the Health Professions Council
Box 10.2
Foot health education for the person with an ‘at risk’ foot
▪ Do not cut your own toenails
▪ Inspect feet daily for any open lesions, cracking, dryness, change in colour, swelling, corn, callus, blisters, warts or signs of infection
▪ Use a mirror to inspect the soles of your feet or ask someone to look for you
▪ Only use a hot water bottle to heat your bed: never place it next to your feet
▪ Never sit close to the fire or heater
▪ Check inside shoes for foreign objects
▪ Wear shoes with soft uppers, preferably lacing
▪ Never wear garters to hold up stockings or socks
Sharp and blunt sensation
A Neurotip can be used to identify if sharp and blunt sensation is present or absent. Again, the person’s eyes should be closed during this examination and the assessor should commence distally and work proximally.
Pressure
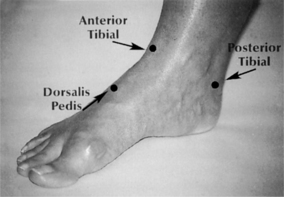
Pressure can effectively be assessed using a 10-g Semmes–Weinstein monofilament in predicting the risk of foot ulceration (
Abbott et al 1998). Monofilaments are cheap and easy to use, making them an ideal screening tool. The sites tested are usually defined by local protocols but are generally agreed to be plantar aspects of the hallux, first, third and fifth metatarsal heads, heel and apices of the fourth and/or fifth digits; these are the most common sites for ulceration to develop. The monofilament is calibrated to buckle when a force of 10 g is exerted and if the person cannot feel the pressure the foot is considered to be insensate. The greater the number of negative responses identified, the greater the risk (
Baker et al 2005).
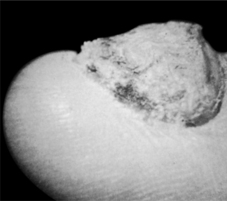
It is important to ensure that any areas of hyperkeratosis are removed before carrying out this test (
Figure 10.6).
Autonomic neuropathy
Individuals with autonomic neuropathy usually have dry and flaky skin on their feet, and sometimes fissuring in the heel area. This can be a potential site for bacterial infection, which might result in ulceration.
Other tests, which require specialised equipment, can be used to enhance the examination of the diabetic foot. These are usually carried out by the podiatrist. The purpose of assessing the diabetic foot under the various parameters outlined above is to determine the foot which is ‘at risk’ and undertake a management strategy according to
SIGN (2001).
The ‘at risk’ foot may, therefore, be defined as the foot which has any one of the clinical signs detailed in
box 10.3Box 10.3
The ‘at risk’ foot has any one of these clinical signs
▪ Absence of pedal pulses
▪ A capillary refill time in excess of 3 seconds
▪ Limb pain and/or paraesthesia
▪ Intermittent claudication
▪ Loss of sensation of light touch, sharp and blunt touch
Further detailed instructions in foot health care (see
Box 10.2) should be given if the person is assessed as having an ‘at risk’ foot. Patient education in the prevention of foot problems is the first line of defence. The individual’s ability to understand the importance of foot health education should be assessed. The person should also receive regular podiatry care and be made aware of a system for seeking immediate medical attention if a foot problem arises. All healthcare professionals must continually reinforce appropriate foot health education.




![]()