FIGURE 42.1 Biopsy site in the posterior superior iliac spine. The needle should be directed toward the anterior superior iliac spine.
Aftercare
■Place a pressure dressing over the site and apply direct external pressure for 5 to 10 minutes to avoid prolonged bleeding and hematoma formation.
■The pressure dressing should remain in place for 24 hours.
■The patient may shower after the pressure dressing is removed, but should avoid immersion in water for 1 week after the procedure to avoid infection.
Complications
Infection and hematoma are the most common complications of bone marrow biopsy and aspiration. Careful technique during and after the procedure can minimize these effects.
Lumbar Puncture
Indications
■Analysis of cerebrospinal fluid (CSF), including pressure measurement, for diagnosis and to assess adequacy of treatment
■Administration of intrathecal chemotherapy
Contraindications
■Increased intracranial pressure.
■Coagulopathy or thrombocytopenia. There are no significant data regarding the optimum platelet count at which a lumbar puncture (LP) can be performed. American National Red Cross transfusion guidelines suggested a minimum of 40,000.
■Infection near the planned site of LP.
■Heparin, low-molecular heparin, or warfarin should be discontinued before procedure and may be resumed after hemostasis is achieved.
Anatomy
■Avoid interspaces above L3 (Fig. 42.2), as the conus medullaris rarely ends below L3 (L1–L2 in adults, L2–L3 in children).
■The L4 spinous process or L4–L5 interspace lies in the center of the supracristal plane (a line drawn between the posterior and superior iliac crests).
■There are eight layers from the skin to the subarachnoid space: skin, supraspinous ligament, interspinous ligament, ligamentum flava, epidural space, dura, subarachnoid membrane, and subarachnoid space.
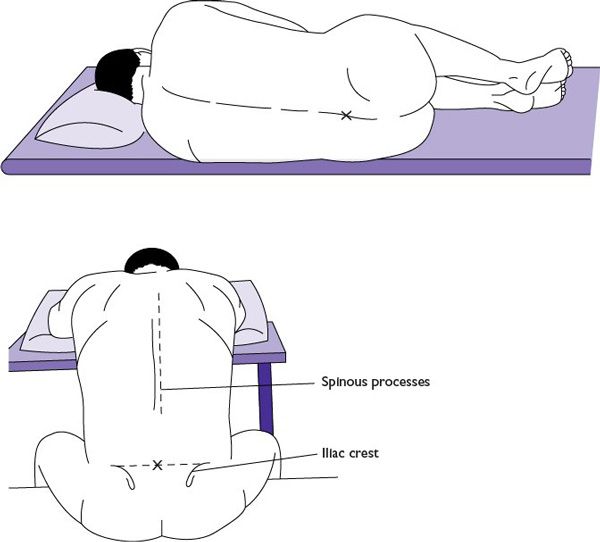
FIGURE 42.2 Anatomy of the lumbar spine. Ideal needle insertion is between L3 and L4 interspace, which can be found where the line joining the superior iliac crests intersects the spinous process of L4. Positioning of the patient for lumbar puncture: in lateral decubitus or sitting position. (From Zuber TJ, Mayeaux EF. Atlas of Primary Care Procedures. Philadelphia, PA: Lippincott Williams & Wilkins; 1994:13.)
Procedure
■Describe the procedure to the patient, with assurances that you will explain what you are about to do before you do it.
■Patient should be in a lateral decubitus or sitting position. The lateral decubitus position is preferable for obtaining opening pressures. The seated position may be used if the patient is obese or has difficulty remaining in the lateral decubitus position. Either seated or lying on one side, the patient should curl into a fetal position with the spine flexed to widen the gap between spinous processes (Fig. 42.2).
■Identify anatomic landmarks and the interspace to be used for the procedure.
■Using sterile technique, prepare the area and one interspace above or below it with povidone–iodine solution. Drape the patient, establishing a sterile field.
■Using 1% lidocaine/bicarb mixture, anesthetize the skin and deeper tissues, carefully avoiding epidural or spinal anesthesia.
■Insert the spinal needle through the skin into the spinous ligament, keeping the needle parallel to the bed or table. Immediately angle the needle 30° to 45° cephalad. The bevel of the spinal needle should be positioned facing the patient’s flank, allowing the needle to spread rather than cut the dural sac. Advance the needle through the eight layers in small increments. With practice, an experienced operator can identify the “pop” as the needle penetrates the dura into the subarachnoid space. Even so, it is wise to remove the stylet to check for CSF before each advance of the needle.
■When the presence of CSF is confirmed, attach a manometer to measure opening pressure. Collect 8 to 15 mL of CSF. If special studies are required, 40 mL of CSF may be safely removed. Four sample tubes should be sent as follows: tube 1, cultures; tube 2, chemistries (especially glucose and protein); tube 3, cell count and differential; tube 4, cytopathology or other special studies (flow cytometry, cytogenetics, etc.).
■Replace the stylet, withdraw the needle, observe the site for CSF leak or hemorrhage, and bandage appropriately.
■Ease the patient into a recumbent position and maintain for 60 minutes.
Complications
■Spinal headache occurs in approximately 20% of patients after LP. Incidence appears to be related to needle size and CSF leak and not to postprocedure positioning. There is no evidence that increased fluid intake prevents spinal headache. It is characterized by pounding pain in the occipital region when the patient is upright. Incidence is highest in female patients, younger patients (peaks 20–40), and patients with a history of headache prior to LP. Patients should be encouraged to remain recumbent if possible, drink plenty of fluids, and take over-the-counter analgesics. For severe, persistent spinal headache (up to 1 week is possible), stronger medication, caffeine, or an analgesic patch may be indicated. Data indicate that a Sprotte (“pencil-tipped”) needle reduces the risk of post-LP headache.
■Nerve root trauma is possible but rare. A low interspace entry site reduces the risk of this complication.
■Cerebellar or medullar herniation occurs rarely in patients with increased intracranial pressure. If recognized early, this process can be reversed.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree