FIGURE 7.1 Barcelona Clinic Liver Cancer (BCLC) HCC staging classification. The classification includes an algorithmic treatment recommendation and outlines the approximate percentage of patients likely diagnosed within each stage in a Western population, as well as their estimated survival with the relevant treatment modalities. HCC, hepatocellular carcinoma; PST, ECOG performance status; CLT, cadaveric liver transplantation; LDLT, living donor liver transplantation; RF, radiofrequency ablation; PEI, percutaneous ethanol injection; TACE, transarterial chemoembolization; OS, overall survival. (Adapted from Bruix J, Sherman M. Management of hepatocellular carcinoma. Hepatology. 2005;42(5):1208-1236. With permission of John Wiley and Sons, Inc.)
The consensus of the American Hepato-Pancreato-Biliary Association (updated in 2010) reasserts the need to use different systems in different patients. Their consensus statement recommends the use of the TNM system to predict the outcome following resection or liver transplantation and the BCLC scheme for patients with advanced HCC who are not candidates for surgery.
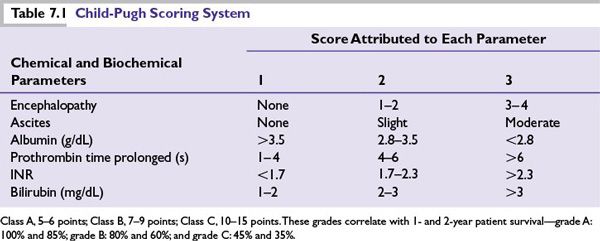
■The Child-Pugh grading system has been incorporated into the management of HCC because it evaluates the status of the underlying liver function and influences treatment (Table 7.1).
TREATMENT
Surgery
■Surgery remains the only possibility for cure in HCC, but it is applicable to only 5% of US population.
■The treatment of HCC is determined by two factors: tumor extent and the severity of the underlying hepatic parenchymal disease.
■Partial hepatectomy: Only 13% to 35% are surgical candidates. Small tumors have the best outcomes. Recurrence is most commonly seen in the remnant liver. Repeat hepatectomy is possible in 10% to 29% of patients. Operative mortality is <5%, but is higher in the presence of cirrhosis. Long-term relapse-free survival rates average 40% or better, and 5-year survival rates as high as 90% are reported in carefully selected patients.
•Postoperative morbidity and mortality are related to the extent of operative resection.
•Major postoperative complications include bile leak and pleural effusion.
■Total hepatectomy and liver transplantation: Transplantation is indicated in patients with severe cirrhosis or where extensive resection leaving minimal liver reserve is required.
■Orthotopic liver transplantation (OLT) is a suitable option for unresectable patients who have a solitary HCC ≤5 cm in diameter or up to three separate lesions none of which is larger than 3 cm, no evidence of gross vascular invasion, and no regional nodal or distant metastases (the Milan/Mazzaferro criteria). Based on these criteria, 4-year survival was reported as 75% to 85%.
■Survival outcomes may be further improved by living donor transplantation, although this remains controversial.
■Disadvantages of transplantation are the expense, the lack of specialty centers performing operations, and the lack of donor livers.
POSTTREATMENT SURVEILLANCE
Even patients who have a good response to treatment are at risk for disease recurrence and second primary HCC. Guidelines from the National Comprehensive Cancer Network (NCCN) suggest the following posttreatment surveillance after resection:
a)Imaging every 3 to 6 months for 2 years, and then annually.
b)Assay of serum AFP, if initially elevated, every 3 months for 2 years then every 6 months.
c)In addition, all patients with the underlying liver disease should be monitored and treated appropriately.
Ablative Techniques
■Local ablation is safe and effective therapy for patients who cannot undergo resection, or as a bridge to transplantation.
■Percutaneous ethanol injection (PEI) and radiofrequency ablation (RFA) are equally effective for tumors <2 cm. However, the necrotic effect of RFA is more predictable in all tumor sizes and its efficacy is clearly superior to that of ethanol injection in larger tumors. PEI is now less commonly used because it is uncomfortable and requires more treatment sessions than RFA, and in addition, it can be difficult to visualize the limits of the lesion on ultrasound because of the bubbles formed during the alcohol injection.
■The main drawbacks of RFA are its higher cost, limited efficacy in lesions adjacent to major blood vessels, and the higher rate (up to 10%) of adverse events (pleural effusion and peritoneal bleeding).
■The recurrence rate after ablation is as high as for resection. Some recurrences will occur in the vicinity of the treated nodule and are due to the presence of microscopic satellites not included in the ablation zone.
■Cryotherapy is also safe and more effective than RFA for larger tumors, but is less suited to a percutaneous approach.
■Hepatic artery chemoembolization (transarterial chemoembolization [TACE]) is based on the principle that >80% of the blood supply to tumors is from the hepatic artery, which supplies only 20% to 30% of normal liver parenchyma. Ligation or embolization of the hepatic artery can induce temporary tumor responses, and when combined with chemotherapy (TACE) may be more efficacious, although data are conflicting. The efficacy of TACE has been shown in a number of meta-analyses, revealing superior progression-free survival (PFS) when compared with best supportive care in locally advanced HCC.
■Indications of TACE:
a)Treatment of large unresectable HCCs not suitable for local ablation.
b)In patients awaiting OLT to reduce the rate of dropout because of local tumor progression.
Benefit in any of these settings is highly dependent upon case mix, including tumor-related factors and the severity of preexisting liver dysfunction.
■The best candidates for TACE are patients with unresectable lesions without vascular invasion or extrahepatic spread and preserved liver function (i.e., Child-Pugh A or B cirrhosis).
■Conventional TACE using doxorubicin (50 to 75 mg/m2) was directly compared with TACE with drug-eluting beads (DEBs) (150 mg doxorubicin per procedure) in a randomized trial of 212 patients with Child-Pugh A/B cirrhosis and unresectable HCC. The DEB group had higher rates of objective response at 6 months (52 versus 44 but the difference was not statistically significant), and significantly lower rates of serious hepatobiliary toxicity and doxorubicin-related side effects. DEBs may be preferred, although long-term outcomes using this technique are not available.
■Absolute contraindications to TACE include the complete absence of hepatopetal blood flow (portal vein thrombosis), encephalopathy, biliary obstruction, and Child-Pugh C cirrhosis.
Radiation
■HCC is a radiosensitive tumor, but it is located in an extremely radiosensitive organ. Normal liver can only tolerate about 20 Gy. The major drawbacks with radiotherapy (RT) are the poor radiation tolerance of normal liver and difficulty with tumor localization. However, safe and effective doses can be given to palliate pain.
■
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree