NUTRITIONAL REQUIREMENTS
■Indirect calorimetry, the preferred method for estimating resting energy expenditure, measures O2 consumed (VO2) and volume of carbon dioxide produced (VCO2) to determine respiratory quotient (RQ). This can be done with a portable metabolic cart operated by a respiratory therapist, or by a handheld device recently approved by the FDA.
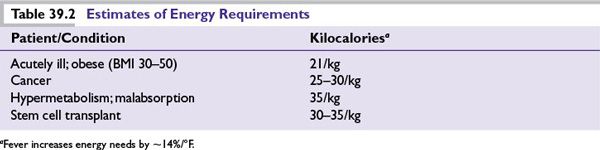
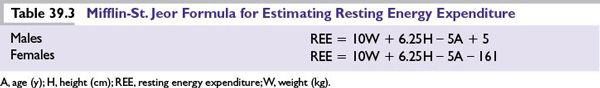
■There are a variety of recommended calculations for estimating energy, fluid, and protein requirements (Table 39.2). However, formulas that rely on stress and activity factors, or calculations such as >45 kcal/kg “for stress,” have been shown to overestimate requirements. It is important not to overfeed cancer patients. Overfeeding can increase infection and induce respiratory distress, hyperglycemia, and fatty liver.
■The initial calorie goal for critically ill patients should be to meet their estimated resting energy expenditure (Table 39.3).
NUTRITIONAL INTERVENTION
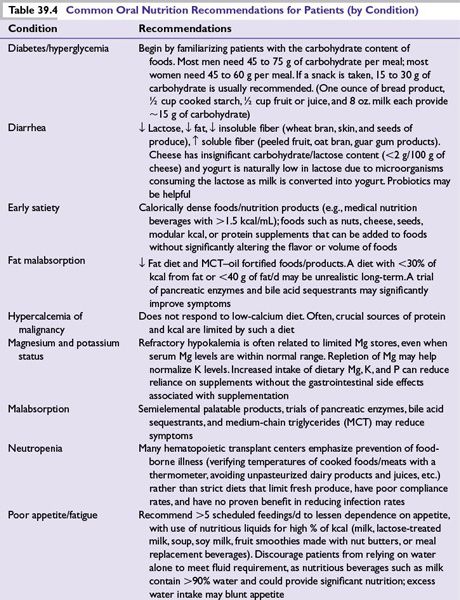
■Nutritional counseling by an RD is associated with improvement in quality of life scores and nutritional parameters, and with success of oral nutritional intervention for oncology patients. Continual reassessment, pharmacologic management, and nutritional counseling can often help avoid costly, risky nutritional support options.
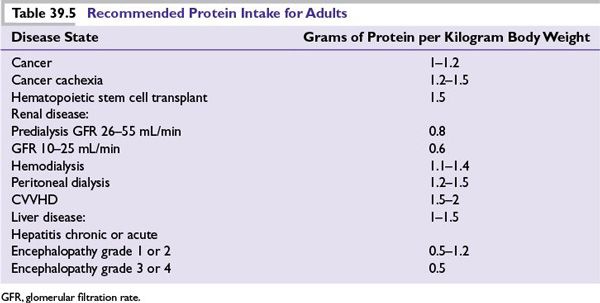
■Nutritional intervention by an RD may include education on individualized nutritional goals for energy, protein, and micronutrients, modification of foods and feeding schedules, fortification of foods with modular nutritional products, supplementation with meal-replacement products, or recommendations for appropriate nutritional support (Tables 39.4 and 39.5).
■Self-imposed diets and the use of dietary supplements should be evaluated by an RD for possible risks to the patient and for their potential to confound protocol results.
■A national registry of RDs is available from the Academy of Nutrition and Dietetics (eatright.org).
MICRONUTRIENT CONSIDERATIONS
■Although two-thirds of American adults are overweight or obese (BMI >25), the majority do not meet their requirements for magnesium, vitamin B6, zinc, and calcium. Optimal dietary intake of vitamins A, C, and E is rare, and patients often take excessive amounts of supplementary antioxidants. Use of dietary supplements should be evaluated as part of a nutritional assessment.
■When treatment involves oxidation (such as radiation therapy), pharmacologic doses of antioxidants might interfere with the treatment objective and may protect the tumor. A diet including foods that are good sources of antioxidants, along with a multivitamin providing 100% to 200% of recommended levels for most nutrients, has not been shown to be harmful and is recommended for patients on limited diets who are undergoing cancer treatment.
■Patients with low levels of ionized calcium, elevated AlkP, and a history of corticosteroid use and risk for osteoporosis should have their vitamin D levels assessed by measuring levels of cholecalciferol [25(OH)D]. Calcitrol, the 1,25 dihydroxy form of vitamin D, is not a reliable indicator of vitamin D status due to its short half-life and dysregulation in the presence of deficiency. The best available current data indicate that a serum 25(OH)D level of >32 ng/mL (80 mmol/L) is a supportable goal.
■Repleting vitamin D stores is associated with improved insulin sensitivity, enhanced immunity, improved musculoskeletal function (reduced falls and fractures), and a beneficial effect on bone mineral density. Low levels of cholecalciferol are commonly found in the elderly, dark-skinned individuals, the obese, and those with malabsorption syndromes and osteoporosis.
NUTRITIONAL SUPPORT
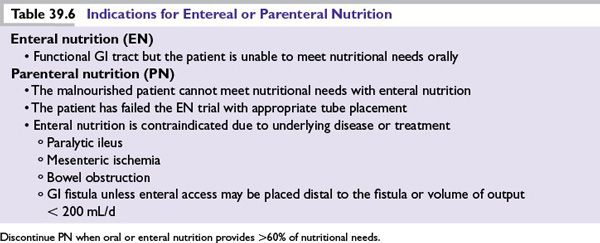
Although tumor growth is stimulated by a variety of nutrients, limiting the nutrients preferred by tumors can be detrimental to the patient. If patients have moderate to severe malnutrition and are unable to meet their nutritional needs with oral intake alone, specialized nutrition support such as parenteral or enteral nutrition is indicated (Table 39.6).
Enteral Nutrition
■Reviews of nutritional support practices indicate that parenteral nutrition (PN) is often instituted even when safer, more physiologic enteral nutritional (EN) support could have been provided. The benefits of EN over PN have been well demonstrated, including fewer infections, decreased catabolic hormones, improved wound healing, shorter hospital stay, and maintenance of gut integrity. In other words, if the gut works, use it.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree