PRETRANSPLANT EVALUATION
Prior to treatment, a thorough discussion highlighting the transplantation procedure as well as risks and benefits associated with the procedure should take place between the physician and the patient.
■HLA typing of the patient and a search for an HLA-matched donor are required if an allogeneic transplant is being considered. Donor search is initiated with siblings as first choice, followed by URDs and alternative donors (UCB and haploidentical).
■Medical history and evaluation.
•Age: Remains an important predictor of treatment-related morbidity and mortality. However, with improving supportive care, HLA typing, and use of RIC regimens, physiologic age is considered more important than chronologic age.
•Review of original diagnosis and previous treatments, including radiation.
•Concomitant medical problems.
•Current medications, important past medications, and allergies.
•Determination of current disease remission status and restaging (by imaging studies, bone marrow biopsy, flow cytometry on blood or bone marrow, lumbar puncture, tissue biopsy as warranted).
•Transfusion history and complications, as well as ABO typing and HLA antibody screening.
•Psychosocial evaluation and delineation of a caregiver.
■Physical examination.
•Thorough physical examination including evaluation of oral cavity and dentition
•Neurologic evaluation to rule out central nervous system involvement, if indicated
•Performance status evaluation
■Organ function analysis.
•Complete blood count.
•Renal function: Preferably a creatinine clearance >60 mL per minute, except in myeloma.
•Hepatic function: Alanine aminotransferase (ALT) and aspartate aminotransferase (AST) less than twice the upper level of normal and bilirubin <2.00 μg/dL.
•Cardiac evaluation: Electrocardiogram and echocardiography or multiple-gated acquisition imaging with ejection fraction.
•Chest x-ray and pulmonary function testing, including diffusing capacity of lung for carbon monoxide and forced vital capacity.
•Scoring schemes such as the hematopoietic cell transplantation-specific comorbidity index (HCT-CI) that can predict NRM based on patient factors may be used to risk-stratify patients.
■Infectious disease evaluation.
•Cytomegalovirus (CMV), HIV, toxoplasmosis, and hepatitis serology
•Serology for herpes simplex virus (HSV), Epstein-Barr virus (EBV), and varicella zoster virus (VZV)
•Assess for prior history of invasive fungal (aspergillus) infection
■Pregnancy testing for all women of child-bearing age and consideration of referral to reproductive center for sperm banking or in vitro fertilization.
AUTOLOGOUS HEMATOPOIETIC CELL TRANSPLANTATION
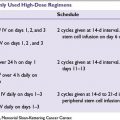
The principle behind high-dose chemotherapy (HDT) is the administration of maximal tolerated doses of cytotoxic agents to maximize tumor kill and overcome relative tumor resistance, which causes prolonged and lethal cytopenias from which the patient may be rescued with the infusion of autologous progenitor cells/HSCs to reconstitute the hematopoietic system. HDT regimens typically use combinations of cytotoxic agents with nonoverlapping organ toxicities. Commonly used regimens include (a) BEAM—carmustine + etoposide + cytarabine + melphalan (lymphoma), (b) CBV—Cy + carmustine + etoposide (lymphoma), and (c) single-agent melphalan 200 mg/m2 (myeloma). HDT is considered in chemotherapy-sensitive tumors or as consolidation therapy for patients in remission (Table 30.1). Overall it is well tolerated with NRM of <5%. Typically the auto-HCT product is mobilized with G-CSF alone or in combination with either chemotherapy or the chemokine antagonist plerixafor. The mobilized PBPC is collected by apheresis and is cryopreserved viably in dimethyl sulfoxide (DMSO) and thawed just prior to infusion. Complications related to HDT and auto-HCT include:
■Rare infusional reactions may include bronchospasm, flushing, hypertension, or hypotension secondary to DMSO.
■Pancytopenia for 10 to 14 days with the predominant use of PBPC and G-CSF. Packed red cell (PRBC) and platelet transfusions may be required.
■Infectious complications—bacterial, viral, and fungal infections may manifest during the cytopenic phase but can be effectively prevented with antimicrobial prophylaxis. Late infections include Pneumocystis jiroveci and varicella requiring continued prophylaxis beyond engraftment.
■Regimen-related toxicities may be (a) acute—infusional reaction (carmustine), hemorrhagic cystitis (Cy), hypotension (etoposide) or (b) delayed—pulmonary toxicity (carmustine, total body irradiation [TBI]), sinusoidal obstruction syndrome (SOS) (TBI or alkylating agents) and myelodysplasia (TBI, alkylating agents, etoposide).
■Relapse of the primary malignancy remains a major barrier to long-term survival.
ALLOGENEIC HEMATOPOIETIC CELL TRANSPLANTATION
Allo-HCT has progressed from an experimental treatment of last resort to standard of care therapy for several disease conditions (Table 30.1). Extensive planning and co-ordination of care is required for all transplant candidates, usually involving a network of physicians and support staff. For patients without a MRD, the NMDP is an invaluable resource for the purpose of URD allo-HCT. All physicians may perform a free initial search for an HLA-matched URD in the NMDP, which maintains a registry of about 9 million potential donors and 145,000 UCB units. As of 2013, the NMDP can search over 16 million URD and 500,000 UCB units as potential donors through its international networks.
Graft-versus-Tumor Effect
In the context of malignancies, the major therapeutic benefit of allo-HCT is the potential for the colonizing donor immune system to recognize and eradicate the malignant or abnormal stem cell clone, the so called graft-versus-tumor (GVT) effect. This immune effect is largely mediated by transplanted donor lymphocytes and is evidenced by the lower relapse rate of hematologic malignancies in patients who undergo allo-HCT than in those who undergo auto-HCT, as well as by an increased relapse rates in syngeneic (identical twin) donor or T-cell–depleted allo-HCT. Arguably the most important and direct evidence for GVT effect comes from the ability of therapeutic donor lymphocyte infusion (DLI) to induce remission in those that relapse after allo-HCT. CML, low-grade lymphomas, chronic lymphocytic leukemia (CLL), and acute myeloid leukemia (AML) are most susceptible to the GVT effects, whereas acute lymphoblastic leukemia and high-grade lymphomas are relatively resistant. Donor-derived T lymphocytes predominantly mediate GVT reactions, although new evidence supports potential contribution from nonspecific cytokines (host and/or donor derived) and alloreactive natural killer (NK) cells (haploidentical allo-HCT).
Human Leukocyte Antigen Typing
The HLA system consists of a series of cell surface proteins and antigen-presenting cells encoded by the major histocompatibility complex located on chromosome 6 and plays a vital role in immune recognition and function. A striking feature of the HLA system is its enormous diversity. HLA class I molecules include HLA -A, -B, and -C antigens and class II molecules are made up of more than 15 antigens (HLA -DP, -DQ, and -DR). The complexity of the HLA system was revealed with the advent of molecular-based HLA typing, which showed that matched HLA phenotypes by serologic testing (antigen level) were actually diverse when classified by DNA analysis (allele level). The importance of careful HLA matching prior to the selection of a donor cannot be overemphasized and independently impacts graft failure, GVHD, and overall survival (OS). High-resolution HLA typing at the allele level is recommended for all recipients at HLA -A, -B, -C, and -DRB1 at the earliest as it avoids unnecessary delays in identifying a donor. The NMDP recommends rigorous matching at the allele level for HLA -A, -B, -C, and -DRB1 (8/8 match) for adult patients and donors, and a less stringent match for HLA -A and -B (antigen level) and HLA -DRB1 (allele level) for UCB units.
Donor Types for Allogeneic Hematopoietic Cell Transplantation
Related Donor
In the United States, approximately 30% of patients will have an HLA-matched sibling and is the preferred donor source. The probability that a sibling pair is HLA matched is about 25%. The risk of GVHD is higher with increasing HLA disparity, and therefore, most transplant centers prefer a 6/6 or 5/6 HLA match (HLA -A, -B, -DRB1).
Syngeneic Donor
Rarely, an identical twin may serve as the donor. As the donor and recipient are genetically identical, GVHD does not typically occur (rarely noted, when a parous female serves as the donor) and post-HCT immunosuppression is not required. By the same principle, such HCT lacks GVT effects and malignancy relapse rates tend to be significantly higher.
Unrelated Donor
As discussed above the search for an appropriate HLA-matched URD is performed through NMDP. It typically takes 3 to 6 months from the time a suitable donor is located to obtaining the allograft, although this period may be shortened when expedited searches are requested. Seventy percent of Caucasians will have an HLA-identical URD, while it is more difficult for ethnic minorities owing to disparities in registered volunteers in the NMDP registry. The risk of GVHD and graft failure increases with HLA mismatch and NMDP requires at least a 6/8 match prior to approving a match. The presence of recipient HLA antibodies against the mismatched donor HLA molecules in the context of a mismatched URD transplant significantly increased the risk of graft failure. Therefore, recipients of mismatched transplants should be screened for the presence of donor-specific HLA antibodies (DSA). Recent data suggest high-resolution matched URD allo-HCT have similar outcomes to MRD allo-HCT.
Alternative Donors
Include UCB and haploidentical-related donors and have been discussed elsewhere in the chapter.
Donor Evaluation
Careful donor selection and evaluation is an integral part of the pretransplantation workup. The donor must be healthy and able to withstand the apheresis procedure or a bone marrow harvest.
■Donor HLA typing.
■ABO typing.
■History-relevant information of the donor: Any previous malignancy within 5 years, except nonmelanoma skin cancer, is considered an absolute exclusion criterion. Age, sex, and parity of the donor impact HCT outcomes, and though they are not exclusion criteria, younger men and nonparous women are preferred when available. Comorbidities like cardiac or coronary artery disease, lung diseases, back or spine disorders, medications, and complications to general anesthesia should be considered.
■
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree