Poor prognostic factors include the following:
■Male gender
■Adenocarcinoma histology
■Increasing number of involved organ sites
■Hepatic or adrenal involvement
■Supraclavicular lymphadenopathy
Advantageous prognostic factors include the following:
■Nonsupraclavicular lymphadenopathy
■Neuroendocrine histology
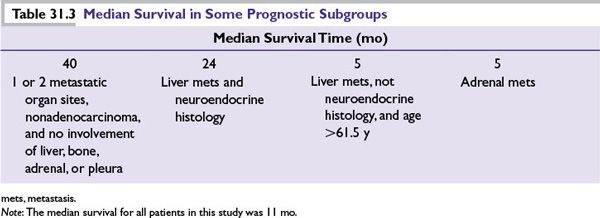
■A study of 1,000 patients (from the M.D. Anderson Cancer Center) revealed several prognostic subgroups. Some of these are shown in Table 31.3.
DIAGNOSIS
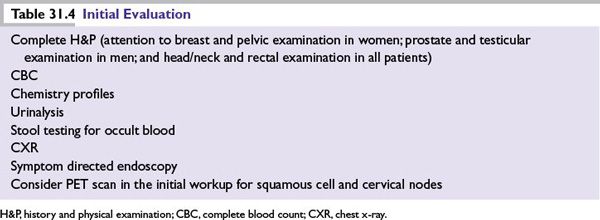
■The recommended initial evaluation is listed in Table 31.4.
■Generous tissue samples should be obtained at the first biopsy.
■Accurate pathologic evaluation is critical.
■Light microscopic examination.
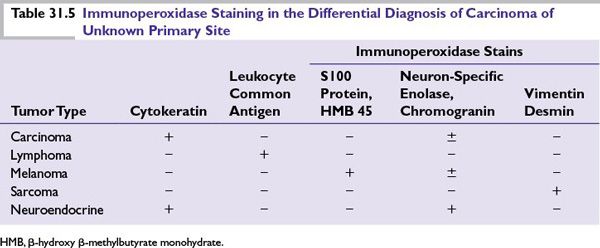
■Immunoperoxidase staining (IPS) should be performed in all CUP cases of poorly differentiated carcinomas (PDCs). Table 31.5 lists some immunoperoxidase stains that are most useful. In addition, some other useful markers are thyroid transcription factor (TTF-1) which is positive in lung and thyroid cancer; WT-1 which is positive in epithelioid mesothelioma, and serous ovarian cancer.
■Electron microscopy should be considered if the tumor cannot be identified by IPS.
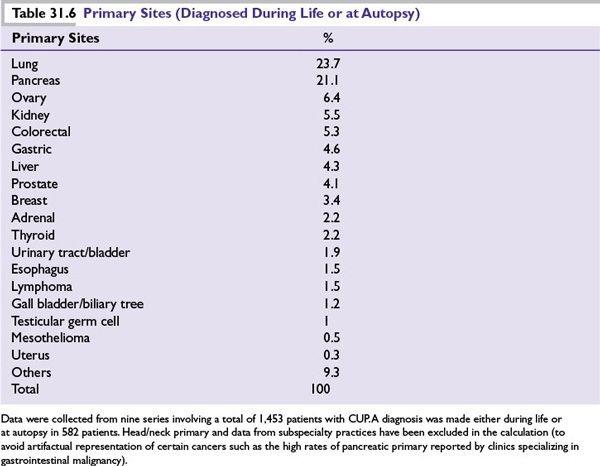
■Most common primary sites are listed in Table 31.6.
■Gene and protein microarray technologies have emerged as valuable tools in the diagnosis of CUP. Three assays that are commercially available in the United States are the bioTheranostics CancerTYPE ID, a 92-gene RT-qPCR that provides a molecular classification of 39 tumor types in metastatic cancer with 85% sensitivity and more than 99% specificity; Pathwork Tissue of Origin Test, a 2000-gene microarray that identifies 15 origin sites, with 89% sensitivity and 99% specificity; and Rosetta miRview mets, a 48 microRNAs RT-qPCR, with 85% to 90% sensitivity and 99% specificity.
WELL-DIFFERENTIATED OR MODERATELY DIFFERENTIATED ADENOCARCINOMA OF UNKNOWN PRIMARY
Clinical Features
■Accounts for about 60% of CUP cases, typically affecting elderly patients.
■Metastatic tumors at multiple sites.
■Poor performance status (PS) at diagnosis.
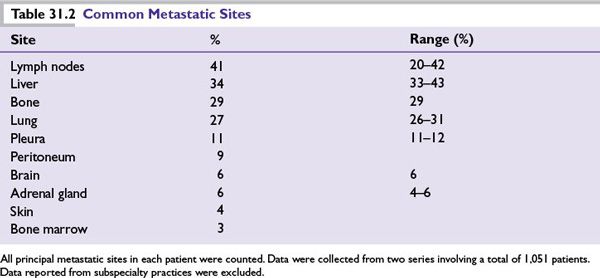
■Common metastatic sites: lymph nodes, liver, lung, and bone.
■Most common primary sites identified: the lung and pancreas (45%) (see Table 31.6).
■Poor prognosis (median survival of 3 to 4 months).
■Primary site is rarely found (<15% before death); an exhaustive search is not indicated.
Further Workup
Additional studies that should be performed include prostate-specific antigen (PSA) serum level and/or IPS for men, and mammography, serum CA 15-3, serum CA 125, and estrogen receptor/progesterone receptor (ER/PR) (IPS) for women. CT scan of the abdomen can identify a primary site in approximately 30% of cases. In patients with CUP who have metastatic adenocarcinoma to the axillary lymph nodes and a negative mammogram, breast magnetic resonance imaging (MRI) detected a primary breast cancer in 9 of 12 (75%) patients in one study and in 19 (86%) of 22 patients in another study.
Treatment
■Most cases (90%) of well-differentiated or moderately differentiated adenocarcinoma of unknown primary show low response rates (RRs) and few complete responses with systemic chemotherapy.
■Patients in this group have a poor prognosis.
■The empiric chemotherapy for CUP is discussed in Table 31.7.
■The various subsets of patients with different types of CUP who can be treated are discussed in the following sections.
Peritoneal Carcinomatosis in Women
■Typical of ovarian cancer.
■Occasionally associated with cancers from the gastrointestinal (GI) tract or breast.
■Serum CA125 level is often elevated.
■Treatment is the same as for stage III ovarian cancer (laparotomy with surgical cytoreduction, followed by platinum-based combination chemotherapy) (see Chapter 17). It should be noted that about 20% of patients have complete remission and 16% have prolonged disease-free survival.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree