Figs. 32.1, 32.2, and 32.3
Small mediastinal parathyroid adenoma on a contrast-enhanced CT
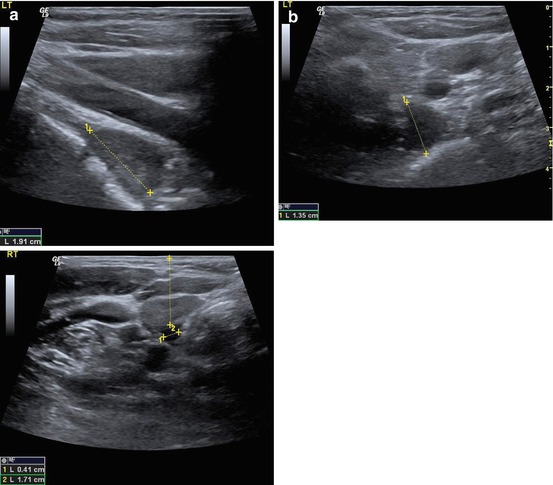
Figs. 32.4a, b, and 32.5
Parathyroid adenoma demonstrated on ultrasound
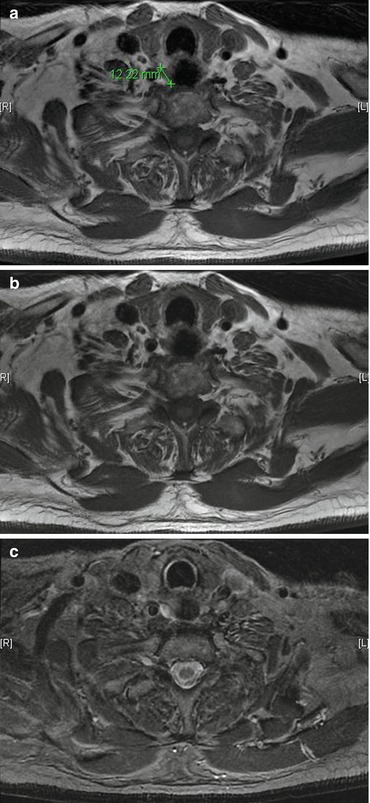
Fig. 32.6
(a, b) T1-weighted MRIs of a small parathyroid adenoma. (c) The same parathyroid adenoma as (a) on fatsat T2-weighted imaging
USS scanning is more likely to be negative where superior tumors have prolapsed behind the inferior thyroid artery to drop behind the esophagus and when the tumor is in the thymus.
Sestamibi
Scanning with 99-Tc-sestamibi is the most reliable way to identify parathyroid tumors preoperatively.
In experienced centers, approximately 60–70 % of patients have a positive scan. SPECT increases the sensitivity of the scan by about 10 % and may be combined with CT scanning.
When USS and sestamibi scans are concordant in identifying a single adenoma, there is about a 98 % likelihood that removing the tumor will result in cure for the patient.
Sestamibi scans are more likely to be negative in small tumors (<500 mg), in multigland disease, and in parathyroid hyperplasia (renal disease, MEN).
As the expected cure rate of >95 % is anticipated even in non-localized patients for first-time parathyroid surgery, the significant additional cost incurred in performing other imaging (CT, MRI) as a matter of routine preoperatively is prohibitive, adds little value, and is not recommended.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree





