5.1 Urea Cycle Defects
5.1.1 Name of Disorder
Urea cycle defects (UCD).
5.1.2 Clinical Definition
The urea cycle is the enzyme cycle whereby ammonia is converted to urea. Disorders of the urea cycle result from genetic defects in any one of the six enzymes that function in urea production (see nearby table).
5.1.3 How It Is Diagnosed
Increased plasma ammonia. In addition, plasma amino acids and urine organic acids and orotic acid, blood glucose, ketones, anion gap, and pH and CO2 may be abnormal. Increased plasma citrulline, argininosuccinic acid, and arginine occur in citrullinemia, argininosuccinic acidemia, and argininemia, respectively.
5.1.4 Nutritional Implications
In acute hyperammonemia, protein intake elevates ammonia further. However, over-restriction of protein can result in body protein catabolism and can contribute to hyperammonemia.


National Urea Cycle Disorders Foundation Web site. Available at: http://www.nucdf.org/ucd.htm. Accessed April 30, 2011.
5.1.5 Pearls
- Lifelong nutrition therapy is focused on promoting protein anabolism during the chronic dietary restriction of protein as part of the treatment.
- High-quality protein is delivered through the use of medical metabolic formulas that contain essential amino acids (EAAs) to support amino acid/protein needs with reduced nitrogen load.
- The urea cycle not only makes urea but also arginine. Arginine becomes a conditionally EAA. Arginine is an important supplement for all urea cycle disorders except arginase deficiency. Citrulline may be used in OTC or CPS deficiency.
- Some common medical metabolic formulas are Cyclinex-1 (Abbott), Cyclinex-2 (Abbott), EAA supplement (Vitaflo), Essential Amino Acid Mix (Nutricia), WND-1 (Mead Johnson), and WND-2 (Mead Johnson).
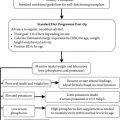
Nutritional Algorithm for Maple Syrup Urine Disease (MSUD)

5.2 Maple Syrup Urine Disease
5.2.1 Name of Disorder
Maple syrup urine disease (MSUD).
5.2.2 Clinical Definition
Disorder of branched-chain amino acid (BCAA) metabolism; block in branchedchain α-ketoacid dehydrogenase complex.
5.2.3 How It Is Diagnosed
Abnormal plasma amino acids (elevated leucine, isoleucine, valine, alloisoleucine) and urine organic acids with abnormal branched-chain hydroxyacids and ketoacids.
5.2.4 Nutritional Implications
Lifelong restriction of leucine, isoleucine, and valine, likely requiring specialized low-protein foods. Supplemental medical formula that is free of BCAAs.
5.2.5 Pearls
- MSUD requires lifelong nutrition therapy.
- If MSUD patient is symptomatic (vomiting, lethargic), it is important to proceed immediately with IV hydration before obtaining laboratory results. Start an IV with D10½ normal saline run at 1.5 maintenance rate. If acidotic, give sodium bicarbonate per biochemical genetics team recommendations.
- If MSUD patient blood leucine is >800 μmol/L or if clinically indicated (excessive vomiting/neurologic compromise), pharmacy may need to order special total parenteral nutrition (free of branched-chain amino acids).
Nutritional Algorithm for Carbohydrate Metabolism Defects: Galactosemia

5.3 Galactosemia
5.3.1 Name of Disorder
Galactosemia.
5.3.2 Clinical Definition
Classic galactosemia is an inherited disorder of galactose metabolism that results from a defect in the enzyme galactose-1-phosphate uridyltransferase (GALT). The accumulation of galactose-1-phosphate (Gal-1-P) and galactose causes multiorgan disease (liver disease, cataracts, renal tubular dysfunction,
growth failure, and ovarian dysfunction in females). Two other very rare forms of galactosemia exist that are due to deficiency in the enzymes galactokinase or uridine diphosphate-Gal-4-epimerase.
5.3.3 How It Is Diagnosed
Quantification of erythrocyte Gal-1-P and GALT activity. Classic galactosemia shows <1% GALT activity and markedly increased Gal-1-P.
5.3.4 Nutritional Implications
Early intervention with a galactose-restricted diet. No breast-feeding. Give powdered soy infant formula. The goal is to restrict galactose to the lowest amount compatible with a diet that is nutritionally adequate. Despite strict elimination of galactose from the diet, outcome is variable. Ensure adequate calcium and vitamin D intake.
Nutritional Algorithm for Carbohydrate Metabolism Defects: Glycogen Storage Disease (GSD) Types 1a and 1b

5.4 Glycogen Storage Disease Types 1a and 1b
5.4.1 Name of Disorder
Glycogen storage disease (GSD) types 1a and 1b.
5.4.2 Clinical Definition
The GSDs are caused by deficiencies of enzymes that regulate the synthesis or degradation of glycogen. The enzyme defect between glucose-6-phosphate and glucose blocks both glycogenolysis and gluconeogenesis. GSD type 1a is due to a deficiency of the enzyme glucose-6-phosphatase, normally found in liver, kidney, and intestinal mucosa. GSD type 1b results from a defect in glucose-6-phosphate translocase, affecting transfer of glucose-6-phosphate into the endoplasmic reticulum. Hypoglycemia occurs when exogenous sources of glucose are exhausted.
5.4.3 How It Is Diagnosed
Liver biopsy and DNA analysis. Clinically suspected in individuals with hepatomegaly, growth retardation, bleeding tendency, severe neutropenia (type 1b), hypoglycemia, and increased lactate, uric acid, triglycerides, and transaminases.
5.4.4 Nutritional Implications
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree