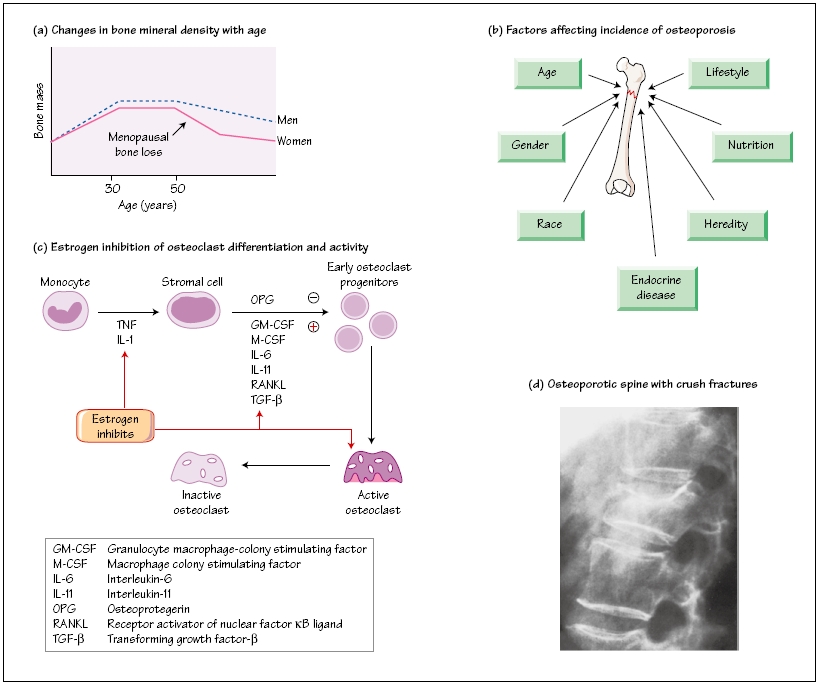
Osteoporosis is a common disease of the elderly, affecting over 2 million women in the UK, and associated with significant morbidity and mortality. It is characterized by ‘fragility fractures’, defined as a fracture occurring after a fall from standing height or less and it is estimated that 33% of women and 20% of men over the age of 80 will sustain a hip fracture due to osteoporosis. Other common sites for osteoporotic fractures include the spine and distal radius (Colles’ fracture) and it is estimated that the cost to the UK National Health Service and social services of treatment for osteoporotic fractures of the hip alone is in the order of £2.3 billion per annum. Primary osteoporosis in women is due to a combination of age and estrogen deficiency; the cause in men is less clear but probably includes age-related falls in both estrogen and androgen concentrations.
Osteoporosis occurs in the context of lifetime changes in bone density. Peak bone density in both males and females is achieved in the late 20’s and age-related bone loss begins at the start of the fifth decade. Peak bone mass is genetically determined and a major predictor of osteoporosis risk in later life. Other factors include sex hormone status, nutrition, calcium and vitamin D status and levels of physical activity. Both men and women exhibit age-related bone loss from the fifth decade, but the process in women is accelerated during the menopause, reflecting the role of estrogen as a major factor in the maintenance of bone mineral density. Osteoporosis is diagnosed by assessing bone mineral density by means of dual-energy X-ray absorptiometry (DEXA) scanning. The patient’s score is measured according to standard deviation scores below normal peak bone mass.
A number of risk factors for osteoporosis have been identified and include age, sex, family history, Caucasian or Asian ethnicity, history of thyroid disease, cigarette smoking and excessive alcohol intake. The major risk factor for fractures in the elderly with osteoporosis is falling. Assessment of the patient should always include risk factors for falling such as visual impairment, cardiovascular disease with syncope, neuromuscular weakness and environmental hazards such as steps or poorly fitting carpets.
Therapeutic intervention may be offered as primary prevention to postmenopausal women, with significant risk factors depending upon their bone density and as secondary prevention following a fracture (see Chapter 55).
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree